Abstract
Development of new antibacterial agents is necessary as drug-resistant bacteria are a threat to global health. In Europe, the European Medicines Agency has been guiding this development process for more than two decades. We investigated preclinical and clinical pre-approval studies to illuminate the current authorization process with emphasis on pharmacokinetic/pharmacodynamic approaches and clinical phases. All centrally authorized systemic antibacterial and antimycobacterial drugs within the European Union were included without any time restriction. Additionally, US Food and Drug Administration-approved antibiotics of the previous 3 years, which were not yet approved by the European Medicines Agency, were included. We focused on preclinical pharmacokinetic/pharmacodynamic studies and phase II and phase III clinical trials. Furthermore, we looked at the recommended dosing regimens and approved indications. In this review, we designed tree diagrams as a new means of illustrating the development process of antibiotics to relate pharmacokinetic/pharmacodynamic phase II and III studies to approved indications. We included 23 (European Medicines Agency, 18; US Food and Drug Administration, 5) antimicrobial agents. Tetracyclines, carbapenems, and cephalosporins were the leading classes. The recommended dosing intervals were significantly shorter in time- vs exposure-dependent drugs (median 8 vs 12, p = 0.006). The majority of approved indications (i.e., acute bacterial skin and soft-tissue infection, community-acquired pneumonia, complicated intra-abdominal infection, complicated urinary tract infection, and complicated skin and soft-tissue infection) used non-inferiority trials. Phase II and III clinical trials investigating community-acquired pneumonia involved the fewest patients. Some promising drugs were marketed in recent years; the individual steps to their authorizations are illuminated. We confirmed the relevance of preclinical pharmacokinetic/pharmacodynamic studies in dosing optimization and decision making in antimicrobial drug development. Non-inferiority clinical trials predominated.
Similar content being viewed by others
Results from in vitro and animal pharmacokinetic/pharmacodynamic studies correlate with recommended dosing intervals. |
We provide an overview of all European Medicines Agency-approved antibiotics and describe some trends of their development. |
We present novel tree diagrams that demonstrate the authorization process at a glance. |
1 Introduction
Because of fast-adapting microbes and inadequate usage of antibacterial drugs, new and clinically relevant resistances constitute a major threat to global health [1]. Although improvements have been made, bacterial infections remain one of the leading causes of death [2]. Therefore, continual and effective development of new antibacterial agents is of utmost importance.
1.1 Authorization Process of Antibacterial Agents in the European Union
The European Medicines Agency (EMA) was founded in 1995 [3]. Since then, the process of authorization has been centralized to a large extent in Europe. The centralized authorization procedure is mandatory for new active substances intended for the treatment of cancer, diabetes mellitus, neurodegenerative diseases, immune dysfunctions, and viral diseases (including human immunodeficiency virus). Furthermore, orphan drugs and more advanced medicines (i.e., gene therapy, somatic cell therapy, or tissue-engineered medicines) have to be approved centrally. Other drugs (e.g., antibiotics) undergo a decentralized or national procedure. Because the entire European market is from an economic point of view more attractive than the markets of single-member states, companies seek central approvals of innovative and promising drugs. The national procedure is almost exclusively followed by generics, herbal medicines, and over-the-counter drugs [4].
To assure quality, the EMA and its Committee for Medicinal Products for Human Use (CHMP) provide guidelines on what the evaluation of medicinal products should include. In the field of antibacterial agents, guidelines cover microbiological investigations, animal studies, pharmacokinetic/pharmacodynamic (PK/PD) studies, and clinical trials [5,6,7].
The EMA publishes the summarized authorization process of every centrally approved medicinal product. Such a scientific review is called a European Public Assessment Report (EPAR). European Public Assessment Reports provide key information on why applications were approved [8] and hence provide a considerable summary of the pre-approval development steps of a drug.
1.2 Role of Preclinical Pharmacokinetic/Pharmacodynamic Studies
Pharmacokinetic/pharmacodynamic indices are a quantitative approach to predict clinical efficacy on the basis of combined PK and PD information. Minimum inhibitory concentration (MIC), i.e., the concentration that inhibits visual bacterial growth in vitro over 18–24 h, is the most important PD parameter. In contrast, PK parameters are measured in vivo by plasma sampling and the determination or calculation of free (i.e., not protein bound) drug concentrations [9]. Furthermore, plasma antibiotic concentrations are also frequently determined in other compartments such as urine, epithelial lining fluid (ELF), or soft tissues. Depending on the antimicrobial class, three relevant indices are traditionally described:
-
1.
the ratio of the (unbound) 24-h area under the curve to MIC (fAUC24/MIC);
-
2.
the ratio of the free peak concentration to MIC (fCmax/MIC); and
-
3.
the time above the MIC expressed as a percentage of the dosing interval (f%T>MIC).
The index showing the best correlation to killing describes the antibacterial profile of an antibiotic. Hence, three patterns of bactericidal activity are distinguished: exposure-dependent (best correlation to fAUC24/MIC), concentration-dependent (best correlation to fCmax/MIC), and time-dependent killing (best correlation to f%T > MIC). Correlations between efficacy (i.e., bacterial killing) and PK/PD indices can be determined using different dosing regimens. In animal models, efficacy is defined as the reduction in colony-forming units (CFU) at the infection site (e.g., murine thigh) [10]. However, the literature on this topic and the terminology are not always strictly consistent. Some authors described only two types: concentration-dependent activity (fAUC24/MIC or fCmax/MIC) and time-dependent activity (f%T > MIC) [10, 11]. Recently, an in silico PK/PD simulation was used not only to test the predictability of in vivo responses on the basis of in vitro results, but also to challenge some basic assumptions of the traditional PK/PD approach. These assumptions include constant MICs, steady pharmacokinetics, and the ignorance of heterogenous bacterial subpopulations [12]. In this model, the predicted magnitudes of the PK/PD indices were in good agreement with actual in vivo results and were sensitive to the misspecification of MICs and other aspects of experimental design. According to the authors, adjustable simulations might be superior to using fixed PK/PD targets, although it should be remembered that these methods are not yet established for antibiotic drug development.
Another pitfall regarding PK/PD descriptions of antibacterial drugs is the correct determination of protein binding. Confounding factors such as temperature, pH, electrolytes, and concentration-dependent protein binding may influence results. In particular with regard to antibacterial drugs characterized by a high protein binding, little deviations can have considerable impacts. For example, a difference in protein binding of 99% vs 97% would result in a difference of 200% regarding the free fraction as well as the fAUC/MIC target. The lack of a standard method for the determination of protein binding aggravates this issue [7, 13].
Even more discerning and arguably more relevant is the determination of the free fraction of antibacterials at the site of infection (e.g., ELF or cerebrospinal fluid). While data on concentrations in these fluids are considered important, the CHMP does not explicitly demand data derived from infected subjects or the assessment of drug concentrations in non-homogenate tissues (e.g., using microdialysis) [7]. Exposures of antibiotics in ELF can differ considerably between critically ill patients and healthy volunteers. Both increased (e.g., piperacillin [14]) and reduced ELF penetrations (e.g., levofloxacin [15]) in critically ill subjects have been observed. In addition to penetration, binding to a pulmonary surfactant may determine the efficacy of antibacterial drugs in lung infections [16]. With respect to cerebrospinal fluid, inflamed meninges generally lead to higher concentrations of antibiotics owing to an impaired function (i.e., increased permeability) of the blood–brain barrier [17].
The murine neutropenic thigh and lung infections are the most relevant models of animal PK/PD studies. Neutropenia is mostly induced to minimize the effect of the immune system as a confounder. For the thigh model, an inoculum of 105–8 CFU of a certain pathogen is injected intra-muscularly. To provide a clinically relevant prediction, clinical isolates of the intended indication are preferred. After antimicrobial therapy and euthanization, tissue is homogenized and the reduction in bacterial burden expressed as CFU/mL in the mice’s thighs indicates the magnitude of efficacy [10]. The CHMP guidelines encourage applicants to provide pathogen-specific PK/PD targets resulting in a net stasis, a 1-log10, and a 2-log10 reduction of CFU [7].
Whereas antimicrobial agents showing time-dependent activity are administered more often or even as a continuous infusion, antimicrobial agents showing concentration-dependent activity are applied less frequently at high doses to attain high peaks. Antimicrobial agents showing an exposure-dependent (sometimes also called dose-dependent) pattern of activity are hardly affected by the dosing interval. For practical reasons, they are given less frequently [18]. The PK/PD assessment is more complex in combination drugs, e.g. when beta-lactamase inhibitors (BLIs) are added to support the efficacy of the main substance by preventing their degradation. The principal assumption is that beta-lactam antibiotics (BLs) in the presence of beta-lactamases are not stable (i.e., not efficacious) but can be protected by BLIs (i.e., efficacious despite the presence of beta-lactamases). The CHMP recommends in vitro testing of BLs in the absence and presence of various concentrations of the BLIs to characterize their interplay. The supporting effect of BLIs can be time dependent, which was the case for avibactam in the presence of ceftazidime [19], or exposure dependent, which was the case for vaborbactam in the presence of meropenem [20]. Ultimately, the actual clinical benefit of BLIs can only be tested in trials involving subjects infected by beta-lactamase-producing bacterial strains. However, clinical studies do not always provide an adequate number of subjects with beta-lactam-resistant but BLI-susceptible pathogens. Hence, preclinical PK/PD studies are particularly essential for the identification of adequate dose regimens of BL-BLI fixed-dose combination regimens.
Because preclinical models are robust indicators for antibacterial activity in humans, they help to optimize dose regimens for efficacy and resistance prevention [9, 21]. Of note, the exposure for preventing the emergence of bacterial resistance appears to be higher than that required for a clinical response [22].
Consequently, well-conducted preclinical PK/PD studies may lower costs and prevent failures in clinical trials by avoiding inadequate study designs in phases II and III. The relevance of PK/PD studies is reflected in an specific CHMP guideline on this topic [7].
1.3 Clinical Drug Development
Historically, the US Food and Drug Administration (FDA) divided clinical trials into three phases [23] and this pattern is widely followed in other parts of the world including Europe. Phase I studies, including first-in-human studies, aim to assess the human pharmacology in healthy volunteer subjects. Data on safety, tolerability, and pharmacokinetics are gathered. Design and inclusion criteria are not very drug specific. The main focus of phase II trials is on exploring therapeutic efficacy and dose finding. Preferably, enrolled patients have conditions that are related or identical to the sought indications. Phase III studies are designed to provide confirmatory evidence of clinical efficacy and safety [24]. In the absence of a licensed standard of care, a superiority trial is requested. Furthermore, specific indications require proof of superiority, even if an approved treatment exists (e.g., acute sinusitis, acute otitis media, and recently also pathogen-related indications with limited treatment options). Otherwise, the evidence of non-inferiority to the standard of care meets the requirements for supporting infection site-specific indications. These indications include amongst others acute bacterial skin and skin structure infections, community-acquired pneumonia (CAP), hospital-acquired pneumonia (HAP), complicated intra-abdominal infections (cIAI), complicated urinary tract infections (cUTI), and uncomplicated urinary tract infections [5]. According to the FDA, phase I, II, and III studies involve a magnitude of ten to a hundred, several hundreds, and hundreds to thousands of subjects, respectively [23]. However, this scheme is simplified and is not always followed strictly. For example, an approach to evade the rather rigid and cost-ineffective three-phase model is a merge of phase I/II and phase II/III studies [25].
The EMA introduced with Adaptive Pathways a new tool to accelerate the proceeding accessibility of highly needed drugs by approving them in earlier stages to small and well-defined populations [26]. After the withdrawal of big companies from the US antibiotics market as a result of unfavorable financial prospects [27], the FDA started the project Generating Antibiotic Incentives Now (GAIN) in 2012, to make the development of new agents more profitable and attractive [28].
Phase IV studies are conducted after marketing. The approval for pediatric use is also often obtained after the initial authorization. Therefore, these studies are not further discussed within this review.
1.4 Aims
In this review, we aimed to provide:
-
1.
a summary of central authorizations of systemic antibacterial substances;
-
2.
an insight into preclinical PK/PD studies and their role in antimicrobial drug development; and
-
3.
a new method of presenting and illustrating the road to antibiotic approval at a glance.
2 Methods
2.1 Inclusion and Exclusion Criteria
This review was mainly prepared by extracting data from EPARs. We included systemic antibacterial substances that were authorized by the EMA without any time restriction. The EMA website was screened applying the following filters [29]:
-
1.
“Human” AND “European public assessment reports (EPAR)” AND “Authorised” AND “antibacterials in systemic use”;
-
2.
“Human” AND “European public assessment reports (EPAR)” AND “Authorised” AND “antimycobacterials”.
Furthermore, antibiotics approved by the FDA since 2017 but not yet by the EMA were included. Therefore, the Centerwatch website was screened for “FDA approved drugs” in the area “Infections and Infectious Diseases” [30]. Only systemic antibacterial substances were selected. The relevant reviews were taken from the FDA access data website [31]. The last revision of the websites was on 3 October, 2019. The FDA-approved antibiotics were added as the EMA will potentially authorize them within the next months or years. The last three EMA-approved antibacterial drugs were all previously accepted by the FDA [32]. On 4 October, 2019, the EMA published the monthly update of applications for new human medicines and it listed all five FDA-approved antibiotics included in this review [33].
Generics and hybrid medicines were excluded because they do not undergo the same authorization process as a novel drug. Missing information in the EPARs was completed, if original publications were found on PubMed and could be identified as the source that the EPAR was referring to with high likelihood. Additionally, we used information from FDA authorization reviews to fill gaps.
2.2 Data Analysis
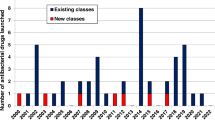
In this review, different PK/PD targets of the various antibiotics are shown. The impact of PK/PD parameters on dosing frequency is demonstrated by plotting and using the Mann–Whitney U test to compare dosing intervals between time- and exposure-dependent agents. Furthermore, information about infection-specific indications and the number of enrolled subjects in phase II and phase III studies are visualized in a bar chart. Innovative tree organization charts present preclinical and clinical pathways to authorization at a glance.
2.3 Applied Software
We performed the statistical analysis using SPSS (SPSS® Statistics, Version 26.0; IBM, Armonk, NY, USA). The tree organization charts were designed using PowerPoint (Microsoft® PowerPoint®, 2019).
3 Results
3.1 Overview of Included Objects
Figure 1 shows the flowchart of the selection process for this review. Overall, 25 antibiotics were identified and 23 included. Tedizolid was assigned to the group of EMA-approved “antibacterials for systemic use”, although it was not labeled as one by the EMA website (Pharmacotherapeutic group: “Not yet assigned”). The generic Daptomycin Hospira® (daptomycin) and the hybrid medicine Vantobra® (inhaled tobramycin) were excluded. Only about half of all authorization reports provided detailed information on the PK/PD targets.
Table 1 provides an overview of all drugs including their marketing name, approval date, and class. Out of the 23 medications, four were combination drugs. Marketing authorization holders were determined in accordance with the EMA website. The leading holder was Merck Sharp & Dome with five approved antibacterial drugs. Tetracyclines, carbapenems, and cephalosporins were the top classes with 13% each. Four drugs were inhaled antimicrobial agents.
3.2 Pharmacokinetic/Pharmacodynamic Indices and Targets
Preclinically determined PK/PD targets for achieving stasis, 1-log reduction, and 2-log reduction are shown in Table 2. The drugs were divided into two groups: exposure- and time-dependent bactericidal profiles. We selected only one exemplary preclinical dataset for each drug. Additionally, data of studies investigating ertapenem [34], telithromycin [35], and tigecycline [36] were included in Table 2. The PK/PD targets of these three antibiotics were not provided in their marketing authorization documents but were investigated afterwards.
The targets of combination drugs refer either to the main antibacterial substance (ceftolozane and ceftazidime) or to compound indices. With respect to meropenem-vaborbactam, the EPAR provided the ratio of AUC24h of vaborbactam to the MIC of meropenem-vaborbactam (fAUCvaborbactam/MICmeropenem-vaborbactam) as the PK/PD index. MICmeropenem-vaborbactam was defined as the MIC of meropenem in the presence of vaborbactam at 8 mg/L [20].
Figure 2 compares recommended dosing intervals between the two groups by using a boxplot. The median (range) values for the time between administrations (hours) of the time-dependent (n = 8) and exposure-dependent (n = 13) groups were 8 (6–24) and 12 (12–24), respectively. Using the non-parametric Mann–Whitney U test, intervals were significantly lower in time-dependent agents (p = 0.006). Dalbavancin and oritavancin are single administered drugs and were therefore excluded (both showed exposure-dependent activity). The outlier in the time dependency group was ertapenem.
3.3 Protein Binding
Protein bindings ranged from 2% (meropenem) to over 99%. The three antibiotics with the highest binding were delamanid, ertapenem, and dalbavancin with > 99.5%, 94%, and 93%, respectively. According to the EPARs, protein binding was exclusively assessed in vitro. The applied methods were only scarcely described. The scientific review of lefamulin reported a dose-dependent binding range of 73–88% using an equilibrium dialysis. In contrast, pooled clinical data of phase I studies suggested values of 94.5–97.2% with a mean unbound fraction of 3.8%. Ultracentrifugation was used to assess the protein binding of relebactam (22%).
3.4 Epithelial Lining Fluid Penetration
Only two of the five antibiotics approved for CAP provided detailed data regarding lung penetration. Using a bronchoalveolar lavage, lefamulin and omadacycline showed a total AUCELF/fAUCplasma ratio of 20 and 2.06, respectively.
Ceftazidime-avibactam and meropenem-vaborbactam are both indicated for HAP. The total AUCELF/fAUCplasma ratios of meropenem and vaborbactam in healthy subjects were 0.65 and 0.79, respectively. With respect to ceftazidime and avibactam, the ratios of total ELF to total plasma concentration were about 0.31 and 0.35, respectively.
3.5 Phase II and III Clinical Trials and Enrolled Subjects
Figure 3a, b presents the six leading indications in phase II and III clinical trials and the mean number of enrolled subjects. In 14 phase III trials of other acute bacterial skin and skin structure infections, a total of 9059 (mean 647) subjects were included, leading to five authorizations (mean enrolled subjects per indication, 1812). With regard to the mean number of enrolled patients per trial, cIAI and cUTI led in phases II and III, respectively. Trials with Pseudomonas aeruginosa infections in patients with cystic fibrosis and CAP involved the fewest subjects. Figure 3c shows the quantity of authorized antibiotics for each indication. About a third of all antibiotics are approved for the treatment of cIAI (n = 7). Table 3 lists all 11 phase III CAP pivotal trials together with parameters of the sample size calculations and observed study outcomes. Trials including fewer patients were mainly conducted in the early 2000s. The CAP studies of the last 10 years included a mean number of 661 patients. With respect to the sample size calculations, non-inferiority margins with a range from − 15 to − 10% and clinical response rates with a range from 79 to 90% were assumed.
a, b Show mean enrolled patients by indication in phase II and III trials, c shows the number of authorized antibiotics for each indication. ABSSSI acute bacterial skin and skin structure infection, CAP community-acquired pneumonia, CF Pseudomonas aeruginosa infection in patients with cystic fibrosis, cIAI complicated intra-abdominal infection, cSSSI complicated skin and skin structure infection, cUTI complicated urinary tract infection
3.6 Pathway to Authorization
Figure 4 demonstrates the pathway to approval for selected antibiotics as the evidence for efficacy grows. Each of the four trees stands for one antibiotic. Information was extracted from EPARs. The trees symbolize the timeline starting with preclinical PK/PD studies, followed by phase II and III clinical trials and finally obtaining an approval for site-specific indications (illustrated as green boxes). Boxes delineating phase II and III trials also give information about the time course by providing the study start date and the study duration in months. Omadacycline, as shown in Fig. 4d, represents a comparable authorization process within the FDA. Despite conducting a phase III trial, it was not indicated for complicated skin and skin structure infections (cSSSI).
Tree organization charts explaining the various steps to approval of indications (a–c European Medicines Agency, d US Food and Drug Administration). The dates and months refer to the start and duration of the phase II and III studies. The dotted lined branch (c) indicates the process after the initial marketing authorization. ABSSSI acute bacterial skin and skin structure infection, AP acute pyelonephritis, BAT best available therapy, BSI blood stream infection, CABP community-acquired bacterial pneumonia, CAZ ceftazidime, cIAI complicated intra-abdominal infection, comp comparator, CRE carbapenem-resistant Enterobacteriaceae, cSSSI complicated skin and skin structure infection, cUTI complicated urinary tract infection, DOR doripenem, HAP hospital-acquired pneumonia, IPM imipenem, LVX levofloxacin, LZD linezolid, MEM meropenem, mos months, MXF moxifloxacin, PIP piperacillin, TAZ tazobactam
4 Discussion
4.1 New Antibacterial Drugs
In the last 10 years, no new group of antibiotics has been marketed in Europe. Food and Drug Administration-approved lefamulin is the first drug of the pleuromutilin class. However, new fixed-dose combinations were created. The evolution and spread of carbapenemase-producing Enterobacteriacae spp. (primarily Escherichia coli and Klebsiella pneumoniae) demanded the addition of BLIs to carbapenems (meropenem-vaborbactam and imipenem-cilastatin-relebactam) [37]. Combinations of cephalosporins and BLIs, such as ceftazidime-avibactam, were also intended to treat drug-resistant pathogens [38]. The two tetracyclines eravacycline and omadacycline are further options for the treatment of infections caused by multidrug-resistant microbes including methicillin-resistant Staphylococcus aureus, vancomycin-resistant Enterococci spp., extended-spectrum BL-producing and carbapenem-resistant Enterobacteriaceae spp. and Acinetobacter baumannii [39,40,41].
Recently, it has been claimed that the antibiotics industry is not profitable enough to push the development forward [42]. However, the stream of new drugs in the European Union has persisted up to now at a low level (1.6 approvals per year in the last 5 years). With regard to the USA, the number of FDA-approved antibiotics have been decreasing linearly from 1980 to 2012 (3.2 per year from 1983 to 1987 vs 0.4 per year from 2008 to 2012). In the last few years, there has been a slight tendency upwards (1.75 per year from 2013 to 2016). This could be related to newly established incentives, which were mentioned earlier [43]. Further efforts will be necessary to stimulate the antibiotics market and above all the development of innovative drugs both in Europe and in the USA.
4.2 Relevance of Pharmacokinetic/Pharmacodynamic Studies
Many publications in the past two decades have dealt with the meaning and implications of PK/PD studies in particular in the field of antimicrobial dose optimization. As a result, both the EMA and the FDA implemented PK/PD experiments and simulations as a key step in development processes. In this review, we provided an overview of selected PK/PD targets and the bactericidal profiles of approved antibiotics. For example, dalbavancin and daptomycin were investigated using comparable models. The required PK/PD target (fAUC/MIC) of daptomycin for achieving a 2-log10 reduction of Streptococcus pneumoniae was two-fold higher than that of dalbavancin (49.8 vs 24.3). This appears to indicate a higher efficacy of dalbavancin as the required fAUC/MIC index for the same effect against the same pathogen is lower. However, comparisons of absolute target values have to be drawn cautiously as models may differ considerably with respect to pathogen strains and the exact conduct of the experiments, but also on the drug exposure that is achieved in vivo and the therapeutic index (ratio between drug exposure needed for therapeutic effect and for occurrence of side effects).
The recommended dosing regimens depended on the results from animal models as well as of clinical safety margins. Indeed, time-dependent antimicrobial drugs were given significantly more frequently. Ertapenem was an exception. When compared to the other carbapenems (meropenem with 2.1 h and imipenem with 1 h), the half-life of ertapenem of 4 h is relatively long. Furthermore, the EPAR referred to calculations that indicated that one administration per day was enough to achieve sufficient target attainment provided MICs did not exceed 4 mg/L.
While new methods of PK/PD modeling are emerging (see Sect. 1.2), recent antibiotic authorizations only focused on the simplified view of time- vs exposure-dependent activity. This may change with growing evidence that more complex models are superior in predicting clinical efficacy and optimizing dosing.
With an increasing number of combination antibiotics on the market, the traditional PK/PD approach is challenged. A single drug can contain a time-dependent as well as an exposure-dependent agent. This is the case for meropenem-vaborbactam. Clearly, the dosing regimen cannot fully consider the PK/PD properties of both substances. With respect to meropenem-vaborbactam, which is administered three times daily, the dosing frequency equals that of meropenem without vaborbactam.
4.3 Pharmacokinetic Considerations
Pharmacokinetic/pharmacodynamic targets rely on the correct assessment of free drug concentrations. This free fraction is predominantly calculated using protein-binding data derived from in vitro experiments. However, in vitro experiments are prone to fallacies. The EPAR of delamanid reported a protein binding of > 99.5%. Such high binding questions the reliability of in vitro methods in this context. Drug stability, precipitation, and adsorption are considered pitfalls in an equilibrium dialysis, which is often regarded as the “gold standard” [13, 44].
An adequate delivery to the sites of infection is of utmost importance for the efficacy of drugs. Although this is widely accepted, the thorough investigation of tissue penetration has been lacking in some of the presented antibiotics. However, more recently authorized antibacterial drugs such as lefamulin, omadacycline, meropenem-vaborbactam, and ceftazidime-avibactam were investigated with respect to their lung penetration using a bronchoalveolar lavage. A bronchoalveolar lavage only allows the assessment of the total concentration of a drug in the ELF. Binding to proteins or surfactants is ignored. The AUCELF/fAUCplasma ratio of lefamulin was ten times higher than that of omadacyline (20 vs 2.06). This is interesting as both were comparable regarding cure rates in clinical trials (86.9% vs 81.1%), plasma AUC/MIC targets for a 1log reduction of S. pneumoniae in a murine model (7 vs 13.6), and in vitro MIC90 against S. pneumoniae (0.25 mcg/mL vs 0.12 mcg/mL). A possible explanation for this discrepancy could be a greater bound fraction of lefamulin in the ELF. Lefamulin also showed in vitro a higher plasma protein binding than omadacycline (73–88% vs 21.3%). Of note, the original publication investigating the ELF penetration of lefamulin reported an AUCELF/fAUCplasma ratio of 5.7 assuming a plasma protein binding of 87% [45]. In the FDA review of lefamulin, a ratio of approximately 20 was stated. This was not an error. The ratio was updated considering the protein binding derived from phase I studies. Hence, assuming an unbound fraction of 3.8% rather than 13% led to a 3.4-fold increase of the AUCELF/fAUCplasma ratio (19.5 instead of 5.7) due to a reduction in the denominator. Undeniably, such processed data are highly vulnerable to misinterpretation and should be handled carefully. More research is required to interpret such results with more confidence and certainty.
4.4 Sample Size and Design of Clinical Trials
Both phase II and III clinical trials investigating CAP and infections with P. aeruginosa in patients with cystic fibrosis involved a smaller number of subjects compared with the other relevant infections. While the prevalence of cystic fibrosis provides a good explanation for this observation, the reasons for lower sample sizes in CAP studies are not so obvious [46]. This might be related to difficulties in diagnosing CAP early and correctly, which are associated with hurdles for the recruitment of previously untreated patients [47]. The EMA-CHMP guidelines recommend a predefined number of the following symptoms as inclusion criteria: dyspnea, increased respiratory rate, increased body temperature, cough, purulent sputum, and pleuritic chest pain. Furthermore, clinical findings such as pathological x-rays, percussion and/or auscultation should be present [6]. Arguably, these inclusion criteria are more complicated, and their assessment requires more clinical experience than a positive test for white blood cells in urine such as in UTIs for example. A more conclusive explanation for this finding is that fewer patients were included in the older studies, mainly in studies investigating telithromycin (four trials) and ertapenem (two trials). In particular, studies investigating telithromycin involved only a few patients. While the pre-defined non-inferiority margins in telithromycin studies were − 15%, the other studies used a non-inferiority margin of − 10% (see Table 3). The latter were in accordance with the EMA-CHMP guidelines that recommend a non-inferiority margin of − 10% for the primary analysis of CAP trials [5].
It should be noted that all of the top five approved ‘side-specific’ indications (acute bacterial skin and skin structure infections, CAP, cIAI, cSSSI, and cUTI) employ non-inferiority trials for which some major concerns exist regarding their sensitivity to detect potential differences in efficacy. First, they do not actually prove non-inferiority, but rather prove that the tested drug is not appreciably worse (i.e., not worse than a pre-defined margin like for example -10%) [48]. Second, inadequacies of the trial conduct (e.g., missing data, low adherence, violation in entry criteria) tend to bias toward non-inferiority [49]. Third, the sample size calculations and estimates of effect sizes (cure rates) are based on data from previous trials investigating the active control drug. The reliability of these data requires a constancy assumption, which particularly in the field of antimicrobial agents is not valid. Because of the new emerging resistance mechanisms, the efficacy of specific antibiotics can vary significantly over time, but also improved concomitant treatment might impact survival, e.g., in the case of sepsis [50]. Finally, there are also ethical concerns regarding this study design. Patients agree to participate in clinical trials because of the reasoned chance of receiving a superior treatment. In the case of non-inferiority trials, they might have only the chance of receiving a not appreciably worse treatment accompanied by potentially higher risks because of a less understood safety profile of the novel treatment [51]. Overall, the current trend of almost exclusively employing non-inferiority trials should be critically scrutinized.
4.5 A Closer Look
4.5.1 Ceftazidime-Avibactam
The cephalosporin-BLI combination drug, which is named in the World Health Organization List of Essential Medicines, and its efficacy against P. aeruginosa were investigated in an murine lung infection model (Fig. 4a) [52]. With regard to the infection site and pathogen, this was a predictive model for the indication HAP that was afterwards supported by a phase III clinical trial [53].
Furthermore, over 300 patients infected by ceftazidime-resistant Gram-negative bacteria could be included in a single study [54]. The comparator was the best available therapy (carbapenems, colistin, or in the case of cIAI, tigecycline). Ceftazidime-avibactam was not inferior in this study.
4.5.2 Meropenem-Vaborbactam
Meropenem-vaborbactam is the first fixed-dose combination drug of carbapenems and BLIs in Europe and also listed as an essential medicine by the World Health Organization [52]. Using a hollow fiber model, the PK/PD profile was investigated in vitro (Fig. 4b). In this experiment, an in-vivo situation is mimicked by simulating dynamical PK changes (changing concentration in the bacteria compartment). Semi-permeable fibers are passed by small drugs, nutrients, and metabolic waste but not bacteria. An environment similar to the extra-capillary space is thereby created [55]. Potential advantages are individual settings of PK parameters, lower costs, and longer experiment durations in comparison with animal PK/PD studies [56]. Both in vivo and in vitro, the efficacy against Enterobacteriaceae spp. was studied. This was the basis for clinical trials with cUTIs and cIAIs. Moreover, the sponsor was able to conduct the biggest clinical trial in patients with carbapenem-resistant Enterobacteriaceae spp. published so far (TANGO II, n = 77) [57]. Indeed, carbapenem-resistant A. baumannii, P. aeruginosa, and Enterbacteriaceae spp. are three of the most critical pathogens. The World Health Organization assigned them exclusively to the Priority 1 group in the list of antibiotic-resistant bacteria [58].
To achieve an indication for the treatment of bacteremia, data of 50 or more patients with this condition are expected according to the CHMP guidelines [5]. Although only 26 patients with bloodstream infections in the phase III trials received meropenem-vaborbactam, the indication was approved because of the clinical experience with meropenem alone, the effects in cUTIs and cIAIs, and support by PK/PD simulations. This was the first example of a pathogen-driven indication pathway of approval.
4.5.3 Ceftolozane-Tazobactam
The pathway to approval involved animal PK/PD studies with clinically relevant Gram-negative bacteria followed by one phase II trial and one phase III trial for each indication (Fig. 4c). In September 2019, the ASPECT-NP trial showed the efficacy and non-inferiority of ceftolozane-tazobactam vs meropenem in 726 patients with ventilator-associated pneumonia [59]. Based on these (at that time unpublished) findings, the EMA extended the indications for the treatment of HAP including ventilator-associated pneumonia in August 2019, 4 years after the initial marketing authorization. This new branch was added in dotted lines to the tree diagram as it was not part of the primary authorization process.
4.5.4 Omadacycline
A murine lung infection model and thigh infection model were the foundations for clinical development in lung infection and soft-tissue infection, respectively (Fig. 4d). Omadacycline was non-inferior to moxifloxacin in almost 800 patients with CAP [60]. With regard to the soft-tissue infections, phase II and phase III clinical trials of patients with cSSSI were conducted. However, this indication was not approved. The sponsor, Paratek Pharmaceuticals Inc., decided to terminate the cSSSI trial as the FDA established new terminology and clinical endpoints regarding skin infection trials. Only 140 out of 790 planned subjects were included. Subjective clinicians’ assessments were recommended as primary endpoints by the prior FDA guidance from 1998 [61]. Since 2013, the clinical response has been defined as a reduction in lesion size of 20% or more [62].
5 Summary
This is the first publication providing a comprehensive review of the development process of all EMA-approved antibiotics. New potent medications are combination drugs or representatives of known classes. Only the pleuromutilin lefamulin represents a novel class. We confirmed the relevance of animal PK/PD studies and in vitro models by showing the influence of their results on indications and recommended dosing regimens. Moreover, considerably smaller sample sizes were found in clinical trials investigating CAP. This might be related to diagnostic difficulties.
To summarize the relevant steps in the development program of antibacterial agents in a single chart, we designed novel tree diagrams. Different information is presented at a glance, e.g., a different type of preclinical PK/PD study (hollow fiber model), failed indications (cSSSI), and straightforward approvals of the selected drugs.
The demand for new antimicrobial agents will continue. Constant reassessment and optimization of the development process in this field are imperative to provide physicians with a variety of options for the treatment of infectious diseases in a world of increasing antimicrobial resistance.
References
World Health Organization. Global antimicrobial resistance surveillance system (GLASS) report: early implementation 2016–2017. Geneva: World Health Organization; 2017.
Global Health Metrics. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1151–210.
Woods K, Wathion N. European Medicines Agency: 20th anniversary book. London: Core Media Services UK Ltd.; 2015.
EMA. Authorisation of medicines. Available from: https://www.ema.europa.eu/en/about-us/what-we-do/authorisation-medicines. Accessed 8 Nov 2019.
EMA-CHMP. Guideline on the evaluation of medicinal products indicated for the treatment of bacterial infections: revision 3 (EMA/844951/2018). London: European Medicines Agency; 2018.
EMA-CHMP. Addendum to the guideline on the evaluation of medicinal products indicated for treatment of bacterial infections (EMA/CHMP/351889/2013). London: European Medicines Agency; 2013.
EMA-CHMP. Guideline on the use of pharmacokinetics and pharmacodynamics in the development of antimicrobial medicinal products (EMA/CHMP/594085/2015). London: European Medicines Agency; 2016.
EMA. European public assessment reports: background and context. Available from: https://www.ema.europa.eu/en/medicines/what-we-publish-when/european-public-assessment-reports-background-context. Accessed 11 Oct 2019.
Andes D, Craig WA. Animal model pharmacokinetics and pharmacodynamics: a critical review. Int J Antimicrob Agents. 2002;19(4):261–8. https://doi.org/10.1016/s0924-8579(02)00022-5.
Zhao M, Lepak AJ, Andes DR. Animal models in the pharmacokinetic/pharmacodynamic evaluation of antimicrobial agents. Bioorg Med Chem. 2016;24(24):6390–400. https://doi.org/10.1016/j.bmc.2016.11.008.
Andes DR, Lepak AJ. In vivo infection models in the pre-clinical pharmacokinetic/pharmacodynamic evaluation of antimicrobial agents. Curr Opin Pharmacol. 2017;36:94–9. https://doi.org/10.1016/j.coph.2017.09.004.
Kristoffersson AN, David-Pierson P, Parrott NJ, Kuhlmann O, Lave T, Friberg LE, et al. Simulation-based evaluation of PK/PD indices for meropenem across patient groups and experimental designs. Pharm Res. 2016;33(5):1115–25. https://doi.org/10.1007/s11095-016-1856-x.
Zeitlinger MA, Derendorf H, Mouton JW, Cars O, Craig WA, Andes D, et al. Protein binding: do we ever learn? Antimicrob Agents Chemother. 2011;55(7):3067–74. https://doi.org/10.1128/AAC.01433-10.
Felton TW, Ogungbenro K, Boselli E, Hope WW, Rodvold KA. Comparison of piperacillin exposure in the lungs of critically ill patients and healthy volunteers. J Antimicrob Chemother. 2018;73(5):1340–7. https://doi.org/10.1093/jac/dkx541.
Heffernan AJ, Sime FB, Lipman J, Dhanani J, Andrews K, Ellwood D, et al. Intrapulmonary pharmacokinetics of antibiotics used to treat nosocomial pneumonia caused by Gram-negative bacilli: a systematic review. Int J Antimicrob Agents. 2019;53(3):234–45. https://doi.org/10.1016/j.ijantimicag.2018.11.011.
Schwameis R, Erdogan-Yildirim Z, Manafi M, Zeitlinger MA, Strommer S, Sauermann R. Effect of pulmonary surfactant on antimicrobial activity in vitro. Antimicrob Agents Chemother. 2013;57(10):5151–4. https://doi.org/10.1128/AAC.00778-13.
Nau R, Seele J, Djukic M, Eiffert H. Pharmacokinetics and pharmacodynamics of antibiotics in central nervous system infections. Curr Opin Infect Dis. 2018;31(1):57–68. https://doi.org/10.1097/QCO.0000000000000418.
Hoo GSR, Liew YX, Kwa AL. Optimisation of antimicrobial dosing based on pharmacokinetic and pharmacodynamic principles. Indian J Med Microbiol. 2017;35(3):340–6. https://doi.org/10.4103/ijmm.IJMM_17_278.
Berkhout J, Melchers MJ, van Mil AC, Seyedmousavi S, Lagarde CM, Schuck VJ, et al. Pharmacodynamics of ceftazidime and avibactam in neutropenic mice with thigh or lung infection. Antimicrob Agents Chemother. 2016;60(1):368–75. https://doi.org/10.1128/AAC.01269-15.
Griffith DC, Sabet M, Tarazi Z, Lomovskaya O, Dudley MN. Pharmacokinetics/pharmacodynamics of vaborbactam, a novel beta-lactamase inhibitor, in combination with meropenem. Antimicrob Agents Chemother. 2018;63(1):e01659–e1718. https://doi.org/10.1128/AAC.01659-18.
Owens RC Jr, Shorr AF. Rational dosing of antimicrobial agents: pharmacokinetic and pharmacodynamic strategies. Am J Health Syst Pharm. 2009;66(12 Suppl. 4):S23–30. https://doi.org/10.2146/090087d.
Sumi CD, Heffernan AJ, Lipman J, Roberts JA, Sime FB. What antibiotic exposures are required to suppress the emergence of resistance for Gram-negative bacteria? A systematic review. Clin Pharmacokinet. 2019;58(11):1407–43. https://doi.org/10.1007/s40262-019-00791-z.
US FDA. Step 3: clinical research. 2018. Available from: https://www.fda.gov/patients/drug-development-process/step-3-clinical-research#Clinical_Research_Phase_Studies. Accessed 11 Oct 2019.
EMA-ICH. E8: general considerations for clinical trials: Step 5 (CPMP/ICH/291/95). London: European Medicines Agency; 1998.
Bamberger M, Moore N, Lechat P. How to improve the clinical development paradigm and its division into phases I, II and III. Therapie. 2011;66(4):331–334, 27-30. https://doi.org/10.2515/therapie/2011046.
Nicotera G, Sferrazza G, Serafino A, Pierimarchi P. The iterative development of medicines through the European Medicine Agency's adaptive pathway approach. Front Med (Lausanne). 2019;6:148. https://doi.org/10.3389/fmed.2019.00148.
Projan SJ. Why is big Pharma getting out of antibacterial drug discovery? Curr Opin Microbiol. 2003;6(5):427–30.
US FDA. Generating antibiotic incentives now. Available from: https://www.fda.gov/media/110982/download. Accessed 17 Apr 2020.
European Medicine Agency. Medicines. Available from: https://www.ema.europa.eu/en/medicines. Accessed 3 Oct 2019.
CenterWatch. FDA approved drugs. Available from: https://www.centerwatch.com/drug-information/fda-approvals/. Accessed 3 Oct 2019.
US FDA. FDA-approved drug products. Available from: https://www.accessdata.fda.gov/scripts/cder/daf/. Accessed 17 Apr 2020.
US FDA. New drugs at FDA: CDER’s new molecular entities and new therapeutic biological products. 2018. Available from: https://www.fda.gov/drugs/development-approval-process-drugs/new-drugs-fda-cders-new-molecular-entities-and-new-therapeutic-biological-products. Accessed 17 Apr 2020.
EMA. Applications for new human medicines under evaluation by the Committee for Medicinal Products for Human Use. Amsterdam: European Medicines Agency; 2019.
Maglio D, Banevicius MA, Sutherland C, Babalola C, Nightingale CH, Nicolau DP. Pharmacodynamic profile of ertapenem against Klebsiella pneumoniae and Escherichia coli in a murine thigh model. Antimicrob Agents Chemother. 2005;49(1):276–80. https://doi.org/10.1128/AAC.49.1.276-280.2005.
Tessier PR, Mattoes HM, Dandekar PK, Nightingale CH, Nicolau DP. Pharmacodynamic profile of telithromycin against macrolide- and fluoroquinolone-resistant Streptococcus pneumoniae in a neutropenic mouse thigh model. Antimicrob Agents Chemother. 2005;49(1):188–94. https://doi.org/10.1128/AAC.49.1.188-194.2005.
Nicasio AM, Crandon JL, Nicolau DP. In vivo pharmacodynamic profile of tigecycline against phenotypically diverse Escherichia coli and Klebsiella pneumoniae isolates. Antimicrob Agents Chemother. 2009;53(7):2756–61. https://doi.org/10.1128/AAC.01678-08.
Dunn SJ, Connor C, McNally A. The evolution and transmission of multi-drug resistant Escherichia coli and Klebsiella pneumoniae: the complexity of clones and plasmids. Curr Opin Microbiol. 2019;51:51–6. https://doi.org/10.1016/j.mib.2019.06.004.
Hidalgo JA, Vinluan CM, Antony N. Ceftazidime/avibactam: a novel cephalosporin/nonbeta-lactam beta-lactamase inhibitor for the treatment of complicated urinary tract infections and complicated intra-abdominal infections. Drug Des Dev Ther. 2016;10:2379–86. https://doi.org/10.2147/DDDT.S110946.
Sutcliffe JA, O'Brien W, Fyfe C, Grossman TH. Antibacterial activity of eravacycline (TP-434), a novel fluorocycline, against hospital and community pathogens. Antimicrob Agents Chemother. 2013;57(11):5548–58. https://doi.org/10.1128/AAC.01288-13.
Livermore DM, Mushtaq S, Warner M, Woodford N. In vitro activity of eravacycline against carbapenem-resistant Enterobacteriaceae and Acinetobacter baumannii. Antimicrob Agents Chemother. 2016;60(6):3840–4. https://doi.org/10.1128/AAC.00436-16.
Pfaller MA, Huband MD, Shortridge D, Flamm RK. Surveillance of omadacycline activity tested against clinical isolates from the United States and Europe as part of the 2016 SENTRY Antimicrobial Surveillance Program. Antimicrob Agents Chemother. 2018;62(4):e02327–e2417. https://doi.org/10.1128/AAC.02327-17.
Daniel GW, McClellan MB, Schneider M, Qian J, Lavezzari G, deGraffenreid E. Value-based strategies for encouriging new development of antimicrobial drugs. Washington, D.C.: Duke-Margolis Center for Health Policy; 2017.
Zheng W, Sun W, Simeonov A. Drug repurposing screens and synergistic drug-combinations for infectious diseases. Br J Pharmacol. 2018;175(2):181–91. https://doi.org/10.1111/bph.13895.
Zhang F, Xue J, Shao J, Jia L. Compilation of 222 drugs' plasma protein binding data and guidance for study designs. Drug Discov Today. 2012;17(9–10):475–85. https://doi.org/10.1016/j.drudis.2011.12.018.
Zeitlinger M, Schwameis R, Burian A, Burian B, Matzneller P, Muller M, et al. Simultaneous assessment of the pharmacokinetics of a pleuromutilin, lefamulin, in plasma, soft tissues and pulmonary epithelial lining fluid. J Antimicrob Chemother. 2016;71(4):1022–6. https://doi.org/10.1093/jac/dkv442.
Farrell PM. The prevalence of cystic fibrosis in the European Union. J Cyst Fibros. 2008;7(5):450–3. https://doi.org/10.1016/j.jcf.2008.03.007.
Kosov M, Riefler J, Belotserkovskiy M. Community-acquired bacterial pneumonia: a challenging diagnosis in clinical trials. J Clin Stud. 2015;7:38–40.
Hills RK. Non-inferiority trials: no better? No worse? No change? No pain? Br J Haematol. 2017;176(6):883–7. https://doi.org/10.1111/bjh.14504.
Fleming TR, Powers JH. Issues in noninferiority trials: the evidence in community-acquired pneumonia. Clin Infect Dis. 2008;47(Suppl. 3):S108–S120120. https://doi.org/10.1086/591390.
Fleming TR. Current issues in non-inferiority trials. Stat Med. 2008;27(3):317–32. https://doi.org/10.1002/sim.2855.
Garattini S, Bertele V. Non-inferiority trials are unethical because they disregard patients' interests. Lancet. 2007;370(9602):1875–7. https://doi.org/10.1016/s0140-6736(07)61604-3.
WHO. Model list of essential medicines, 21st list. Geneva: World Health Organization; 2019.
Torres A, Zhong N, Pachl J, Timsit JF, Kollef M, Chen Z, et al. Ceftazidime-avibactam versus meropenem in nosocomial pneumonia, including ventilator-associated pneumonia (REPROVE): a randomised, double-blind, phase 3 non-inferiority trial. Lancet Infect Dis. 2018;18(3):285–95. https://doi.org/10.1016/S1473-3099(17)30747-8.
Carmeli Y, Armstrong J, Laud PJ, Newell P, Stone G, Wardman A, et al. Ceftazidime-avibactam or best available therapy in patients with ceftazidime-resistant Enterobacteriaceae and Pseudomonas aeruginosa complicated urinary tract infections or complicated intra-abdominal infections (REPRISE): a randomised, pathogen-directed, phase 3 study. Lancet Infect Dis. 2016;16(6):661–73. https://doi.org/10.1016/S1473-3099(16)30004-4.
Cadwell J. The hollow fiber infection model for antimicrobial pharmacodynamics and pharmacokinetics. Adv Pharmacoepidem Drug Safety. 2012;S1:007.
Velkov T, Bergen PJ, Lora-Tamayo J, Landersdorfer CB, Li J. PK/PD models in antibacterial development. Curr Opin Microbiol. 2013;16(5):573–9. https://doi.org/10.1016/j.mib.2013.06.010.
Wunderink RG, Giamarellos-Bourboulis EJ, Rahav G, Mathers AJ, Bassetti M, Vazquez J, et al. Effect and safety of meropenem-vaborbactam versus best-available therapy in patients with carbapenem-resistant Enterobacteriaceae infections: the TANGO II randomized clinical trial. Infect Dis Ther. 2018;7(4):439–55. https://doi.org/10.1007/s40121-018-0214-1.
WHO. Global priority list of antibiotic-resistant bacteria to guide research, discovery, and development of new antibiotics. Geneva: World Health Organization; 2017.
Kollef MH, Novacek M, Kivistik U, Rea-Neto A, Shime N, Martin-Loeches I, et al. Ceftolozane-tazobactam versus meropenem for treatment of nosocomial pneumonia (ASPECT-NP): a randomised, controlled, double-blind, phase 3, non-inferiority trial. Lancet Infect Dis. 2019;19(12):1299–311. https://doi.org/10.1016/S1473-3099(19)30403-7.
Stets R, Popescu M, Gonong JR, Mitha I, Nseir W, Madej A, et al. Omadacycline for community-acquired bacterial pneumonia. N Engl J Med. 2019;380(6):517–27. https://doi.org/10.1056/NEJMoa1800201.
Pulido-Cejudo A, Guzman-Gutierrez M, Jalife-Montano A, Ortiz-Covarrubias A, Martinez-Ordaz JL, Noyola-Villalobos HF, et al. Management of acute bacterial skin and skin structure infections with a focus on patients at high risk of treatment failure. Ther Adv Infect Dis. 2017;4(5):143–61. https://doi.org/10.1177/2049936117723228.
US FDA. Guidance for industry: acute bacterial skin and skin structure infections: developing drugs for treatment. Silver Spring: US Food and Drug Administration; 2013.
File TM Jr, Low DE, Eckburg PB, Talbot GH, Friedland HD, Lee J, et al. FOCUS 1: a randomized, double-blinded, multicentre, phase III trial of the efficacy and safety of ceftaroline fosamil versus ceftriaxone in community-acquired pneumonia. J Antimicrob Chemother. 2011;66(Suppl. 3):iii19–iii32. https://doi.org/10.1093/jac/dkr096.
Low DE, File TM Jr, Eckburg PB, Talbot GH, David Friedland H, Lee J, et al. FOCUS 2: a randomized, double-blinded, multicentre, phase III trial of the efficacy and safety of ceftaroline fosamil versus ceftriaxone in community-acquired pneumonia. J Antimicrob Chemother. 2011;66(Suppl. 3):iii33–iii44. https://doi.org/10.1093/jac/dkr097.
Ortiz-Ruiz G, Caballero-Lopez J, Friedland IR, Woods GL, Carides A, Protocol 018 Ertapenem Community-Acquired Pneumonia Study G. A study evaluating the efficacy, safety, and tolerability of ertapenem versus ceftriaxone for the treatment of community-acquired pneumonia in adults. Clin Infect Dis. 2002;34(8):1076–83. https://doi.org/10.1086/339543.
Vetter N, Cambronero-Hernandez E, Rohlf J, Simon S, Carides A, Oliveria T, et al. A prospective, randomized, double-blind multicenter comparison of parenteral ertapenem and ceftriaxone for the treatment of hospitalized adults with community-acquired pneumonia. Clin Ther. 2002;24(11):1770–855. https://doi.org/10.1016/s0149-2918(02)80078-9.
File TM, Goldberg L, Das A, Sweeney C, Saviski J, Gelone SP, et al. Efficacy and safety of intravenous-to-oral lefamulin, a pleuromutilin antibiotic, for the treatment of community-acquired bacterial pneumonia: the phase III Lefamulin Evaluation Against Pneumonia (LEAP 1) trial. Clin Infect Dis. 2019;69(11):1856–67. https://doi.org/10.1093/cid/ciz090.
Alexander E, Goldberg L, Das AF, Moran GJ, Sandrock C, Gasink LB, et al. Oral lefamulin vs moxifloxacin for early clinical response among adults with community-acquired bacterial pneumonia: the LEAP 2 randomized clinical trial. JAMA. 2019;322(17):1661–71. https://doi.org/10.1001/jama.2019.15468.
Van Rensburg DJ, Matthews PA, Leroy B. Efficacy and safety of telithromycin in community-acquired pneumonia. Curr Med Res Opin. 2002;18(7):397–400. https://doi.org/10.1185/030079902125001191.
Hagberg L, Torres A, van Rensburg D, Leroy B, Rangaraju M, Ruuth E. Efficacy and tolerability of once-daily telithromycin compared with high-dose amoxicillin for treatment of community-acquired pneumonia. Infection. 2002;30(6):378–86. https://doi.org/10.1007/s15010-002-2096-z.
Mathers Dunbar L, Hassman J, Tellier G. Efficacy and tolerability of once-daily oral telithromycin compared with clarithromycin for the treatment of community-acquired pneumonia in adults. Clin Ther. 2004;26(1):48–62. https://doi.org/10.1016/s0149-2918(04)90005-7.
Pullman J, Champlin J, Vrooman PS Jr. Efficacy and tolerability of once-daily oral therapy with telithromycin compared with trovafloxacin for the treatment of community-acquired pneumonia in adults. Int J Clin Pract. 2003;57(5):377–84.
Acknowledgements
Open access funding provided by Medical University of Vienna.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No sources of funding were used to assist with the preparation of this review.
Conflict of interest
Anselm Jorda and Markus Zeitlinger have no conflicts of interest that are directly relevant to the content of this review.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Jorda, A., Zeitlinger, M. Preclinical Pharmacokinetic/Pharmacodynamic Studies and Clinical Trials in the Drug Development Process of EMA-Approved Antibacterial Agents: A Review. Clin Pharmacokinet 59, 1071–1084 (2020). https://doi.org/10.1007/s40262-020-00892-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-020-00892-0