Abstract
Background
Warfarin is a difficult drug to dose accurately and safely due to large inter-individual variability in dose requirements. Current dosing strategies appear to be sub-optimal, with reports indicating that patients achieve international normalized ratios (INRs) within the therapeutic range only 40–65 % of the time. The consequences of poor INR control are potentially severe with INRs below 2 carrying an increased risk of clotting while INRs >4 increase the risk of major bleeding events. Bayesian forecasting methods have the potential to improve INR control.
Aims
The aims of this study were to (1) prospectively assess the predictive performance of a Bayesian dosing method for warfarin implemented in TCIWorks; and (2) determine the expected time in the therapeutic range (TTR) of INRs predicted using TCIWorks.
Methods
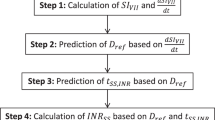
Patients who were initiating warfarin therapy were prospectively recruited from Dunedin Hospital, Dunedin, New Zealand. Warfarin doses were entered into TCIWorks from the first day of therapy until a stable steady-state INR (INRss) was achieved. The predicted INRss values were determined using the first zero to six serially collected INR observations. Observed and predicted INRss values were compared using measures of bias (mean prediction error [MPE]) and imprecision (root mean square error [RMSE]). The TTR was determined by calculating the percentage of predicted INRss values between 2 and 3 when zero to six serially collected INR observations were available.
Results
A total of 55 patients were recruited between March and November 2011. When no observed INR values were available the resulting INRss predictions were positively biased (MPE 0.52 [95 % CI 0.30, 0.73]); however, this disappeared once observed INR values were entered into TCIWorks. The precision of the predicted INRss values improved dramatically once three or more observed INR values were available (RMSE <0.53) compared with no INRs (RMSE 0.96). These results suggest that TCIWorks will be effective at maintaining the INR within the therapeutic INR range (2–3) 65 % of the time when three INR measurements are available and 80 % of the time when six INR measurements are available.
Conclusion
The TCIWorks warfarin dosing method produced accurate and precise INRss predictions. We predict that the method will provide an INR value within the therapeutic range 65–80 % of the time once three or more INR observations are available, making this a useful tool for clinicians and warfarin clinics. Further research to assess the impact of this method on long-term INR control is warranted.





Similar content being viewed by others
References
Chiquett E, Amato MG, Bussey HI. Comparison of an anticoagulation clinic with usual medical care: anticoagulation control, patient outcomes, and health care costs. Arch Intern Med. 1998;158:1641–7.
Matchar DB, Jacobson A, Dolor R, et al. Effect of home testing of international normalized ratio on clinical events. N Engl J Med. 2010;363:1608–20.
van Walraven C, Jennings A, Oake N, et al. Effect of study setting on anticoagulation control. Chest. 2006;129(5):1155–66.
Witt DM, Sadler MA, Shanahan RL, et al. Effect of a centralized clinical pharmacy anticoagulation service on the outcomes of anticoagulation therapy. Chest. 2005;127:1515–22.
Anticoagulants in the Secondary Prevention of Events in Coronary Thrombosis (ASPECT) Research Group. Effect of long-term oral anticoagulant treatment on mortality and cardiovascular morbidity. Lancet 1994;343(8896): 499–503.
The Stroke Prevention in Atrial Fibrillation Investigators. Bleeding during antithrombotic therapy in patients with atrial fibrillation. Arch Intern Med. 1996;156(4):409–16.
Jones M, McEwan P, Morgan CL, et al. Evaluation of the pattern of treatment, level of anticoagulation control, and outcome of treatment with warfarin in patients with non-valvar atrial fibrillation: a record linkage study in a large British population. Heart. 2005;91(4):472–7.
Hylek EM, Evans-Molina C, et al. Major hemorrhage and tolerability of warfarin in the first year of therapy among elderly patients with atrial fibrillation. Circulation. 2007;115(21):2689–96.
Oake N, Fergusson DA, Forster AJ, et al. Frequency of adverse events in patients with poor anticoagulation: a meta-analysis. CMAJ. 2007;176(11):1589–94.
Oake N, Jennings A, Forster AJ, et al. Anticoagulation intensity and outcomes among patients prescribed oral anticoagulant therapy: a systematic review and meta-analysis. CMAJ. 2008;179(3):235–44.
Hamberg AK, Wadelius M, Lindh JD, et al. A pharmacometric model describing the relationship between warfarin dose and INR response with respect to variations in CYP2C9, VKORC1, and age. Clin Pharmacol Ther. 2010;87(6):727–34.
Lind M, Fahlen M, Kosiborod M, et al. Variability of INR and its relationship with mortality, stroke, bleeding and hospitalisations in patients with atrial fibrillation. Thromb Res. 2012;129(1):32–5.
Lader E, Martin N, Cohen G, et al. Warfarin therapeutic monitoring: is 70% time in the therapeutic range the best we can do? J Clin Pharm Ther. 2012;37(4):375–7.
White RH, Hong R, Venook AP, et al. Initiation of warfarin therapy: comparison of physician dosing with computer-assisted dosing. J Gen Intern Med. 1987;2(3):141–8.
Motykie GD, Mokhtee D, Zebala LP, et al. The use of a Bayesian forecasting model in the management of warfarin therapy after total hip arthroplasty. J Arthroplasty. 1999;14(8):988–93.
Wright DFB, Duffull SB. Development of a bayesian forecasting method for warfarin dose individualization. Pharm Res. 2011;28(5):1100–11.
The International Warfarin Pharmacogenetics Consortium. Estimation of the warfarin dose with clinical and pharmacogenetic data. N Engl J Med. 2009;360(8):753–64.
Anderson JL, Horne BD, Stevens SM, et al. Randomized trial of genotype-guided versus standard warfarin dosing in patients initiating oral anticoagulation. Circulation. 2007;116(22):2563–70.
Lenzini P, Wadelius M, Kimmel S, et al. Integration of genetic, clinical, and INR data to refine warfarin dosing. Clin Pharmacol Ther. 2010;87(5):572–8.
Sheiner LB, Beal SL. Bayesian individualization of pharmacokinetics: simple implementation and comparison with non-Bayesian methods. J Pharm Sci. 1982;71(12):1344–8.
Holford NH. The target concentration approach to clinical drug development. Clin Pharmacokinet. 1995;29(5):287–91.
Holford NHG, Tett S. Therapeutic drug monitoring: the strategy of target concentration intervention. In: Speight E, Holford NGH, editors. Avery’s drug treatment. 4th ed. Auckland: Adis International; 1997. p. 225–59.
Holford NH. Target concentration intervention: beyond Y2K. Br J Clin Pharmacol. 2001;52(Suppl 1):55S–9S.
Matthews I, Kirkpatrick C, Holford N. Quantitative justification for target concentration intervention–parameter variability and predictive performance using population pharmacokinetic models for aminoglycosides. Br J Clin Pharmacol. 2004;58(1):8–19.
Wadelius M, Chen LY, Lindh JD, et al. The largest prospective warfarin-treated cohort supports genetic forecasting. Blood. 2009;113(4):784–92.
Takahashi H, Wilkinson GR, Padrini R, et al. CYP2C9 and oral anticoagulation therapy with acenocoumarol and warfarin: similarities yet differences. Clin Pharmacol Ther. 2004;75(5):376–80.
Sheiner LB, Beal SL. Some suggestions for measuring predictive performance. J Pharmacokinet Biopharm. 1981;9(4):503–12.
Rosendaal FR, Cannegieter SC, van der Meer FJ, Briët EA. Method to determine the optimal intensity of oral anticoagulant therapy. Thromb Haemost. 1993;69:236–9.
Fennerty A, Dolben J, Thomas P, et al. Flexible induction dose regimen for warfarin and prediction of maintenance dose. Br Med J (Clin Res Ed). 1984;288(6426):1268–70.
Tait RC, Sefcick A. A warfarin induction regimen for out-patient anticoagulation in patients with atrial fibrillation. Br J Haematol. 1998;101(3):450–4.
Gedge J, Orme S, Hampton KK, et al. A comparison of a low-dose warfarin induction regimen with the modified Fennerty regimen in elderly inpatients. Age Ageing. 2000;29(1):31–4.
Ryan PJ, Gilbert M, Rose PE. Computer control of anticoagulant dose for therapeutic management. BMJ. 1989;299(6709):1207–9.
Manotti C, Moia M, Palareti G, et al. Effect of computer-aided management on the quality of treatment in anticoagulated patients: a prospective, randomized, multicenter trial of APROAT (Automated PRogram for Oral Anticoagulant Treatment). Haematologica. 2001;86(10):1060–70.
Poller L, Shiach CR, MacCallum PK, et al. Multicentre randomised study of computerised anticoagulant dosage. Lancet. 1998;352(9139):1505–9.
Ageno W, Johnson J, Nowacki B, et al. A computer generated induction system for hospitalized patients starting on oral anticoagulant therapy. Thromb Haemost. 2000;83(6):849–52.
Wilson R, James AH. Computer assisted management of warfarin treatment. Br Med J (Clin Res Ed). 1984;289(6442):422–4.
Gage BF, Eby C, Johnson JA, et al. Use of pharmacogenetic and clinical factors to predict the therapeutic dose of warfarin. Clin Pharmacol Ther. 2008;84(3):326–31.
McMillin GA, Melis R, Wilson A, et al. Gene-based warfarin dosing compared with standard of care practices in an orthopedic surgery population: a prospective, parallel cohort study. Ther Drug Monit. 2010;32(3):338–45.
Caraco Y, Blotnick S, Muszkat M. CYP2C9 genotype-guided warfarin prescribing enhances the efficacy and safety of anticoagulation: a prospective randomized controlled study. Clin Pharmacol Ther. 2007;83(3):460–70.
Sconce EA, Khan TI, Wynne HA, et al. The impact of CYP2C9 and VKORC1 genetic polymorphism and patient characteristics upon warfarin dose requirements: proposal for a new dosing regimen. Blood. 2005;106(7):2329–33.
Duffull SB, Begg EJ, Robinson BA, et al. A sequential Bayesian algorithm for dose individualisation of carboplatin. Cancer Chemother Pharmacol. 1997;39(4):317–26.
Duffull SB, Kirkpatrick CM, Begg EJ. Comparison of two Bayesian approaches to dose-individualization for once-daily aminoglycoside regimens. Br J Clin Pharmacol. 1997;43(2):125–35.
Peng B, Boddy AV, Cole M, et al. Comparison of methods for the estimation of carboplatin pharmacokinetics in paediatric cancer patients. Eur J Cancer. 1995;31A(11):1804–10.
Burton ME, Brater DC, Chen PS, et al. A Bayesian feedback method of aminoglycoside dosing. Clin Pharmacol Ther. 1985;37(3):349–57.
de Jonge ME, van den Bongard HJ, Huitema AD, et al. Bayesian pharmacokinetically guided dosing of paclitaxel in patients with non-small cell lung cancer. Clin Cancer Res. 2004;10(7):2237–44.
Staatz CE, Tett SE. Maximum a posteriori Bayesian estimation of mycophenolic acid area under the concentration-time curve: is this clinically useful for dosage prediction yet? Clin Pharmacokinet. 2011;50(12):759–72.
Vadher B, Patterson DLH, Leaning M. Prediction of the international normalized ratio and maintenance dose during the initiation of warfarin therapy. Br J Clin Pharmacol. 1999;48(1):63–70.
Pitsiu M, Parker EM, Aarons L, et al. A Bayesian method based on clotting factor activity for the prediction of maintenance warfarin dosage regimens. Ther Drug Monit. 2003;25(1):36–40.
Boyle DA, Ludden TM, Carter BL, et al. Evaluation of a Bayesian regression program for predicting warfarin response. Ther Drug Monit. 1989;11(3):276–84.
Svec JM, Coleman RW, Mungall DR, et al. Bayesian pharmacokinetic/pharmacodynamic forecasting of prothrombin response to warfarin therapy: preliminary evaluation. Ther Drug Monit. 1985;7(2):174–80.
White RH, Mungall D. Outpatient management of warfarin therapy: comparison of computer-predicted dosage adjustment to skilled professional care. Ther Drug Monit. 1991;13(1):46–50.
Farrow L, Mungall D, Raskob G, et al. Predicting the daily prothrombin time response to warfarin. Ther Drug Monit. 1990;12(3):246–9.
Kravitz RL, Neufeld JD, Hogarth MA, et al. From insight to implementation: lessons from a multi-site trial of a PDA-based warfarin dose calculator. In: Henriksen K, Battles JB, Marks ES, Lewin DI, editors. Advances in patient safety: from research to implementation (volume 3: implementation issues). Rockville: Agency for Healthcare Research and Quality (US); 2005 Feb. p. 395–409.
Theofanous TG, Barile RG. Multiple-dose kinetics of oral anticoagulants: methods of analysis and optimized dosing. J Pharm Sci. 1973;62(2):261–6.
Holford NHG. Clinical pharmacokinetics and pharmacodynamics of warfarin: understanding the dose-effect relationship. Clin Pharmacokinet. 1986;11(6):483–504.
Acknowledgments
The authors wish to thank the Pharmacy Department at Dunedin Hospital, Professor Andre van Rij and the staff of the Otago Vascular Diagnostics Unit for assistance with patient recruitment. The authors are grateful to Lionel van den Berg from the University of Queensland and Professor Carl Kirkpatrick from Monash University for invaluable assistance with TCIWorks. We wish to thank Anna Karin Hamberg from the University of Uppsala for generous assistance with the warfarin model and for helpful comments on the manuscript. This study was funded by a research grant from the New Zealand Pharmacy and Education Research Foundation (NZPERF), PO Box 11-640, Manners Street, Wellington, New Zealand. At the time of writing, Dan Wright was the recipient of a University of Otago PhD scholarship.
Conflict of interest
The authors have no conflicts of interest that are directly relevant to the content of this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wright, D.F.B., Duffull, S.B. A Bayesian Dose-Individualization Method for Warfarin. Clin Pharmacokinet 52, 59–68 (2013). https://doi.org/10.1007/s40262-012-0017-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-012-0017-6