Abstract
The pharmacokinetics of morphine in paediatrics have been widely studied using different approaches and modelling techniques. In this review, we explore advantages and disadvantages of the different data analysis techniques that have been applied, with specific focus on the accuracy of morphine clearance predictions by reported paediatric pharmacokinetic models. Twenty paediatric studies reported a wide range in morphine clearance values using traditional, rather descriptive methods. Clearance values were expressed per kilogram bodyweight, while maturation in clearance was described by comparing mean clearance per kilogram bodyweight between age-stratified subgroups. Population modelling allows for the analysis of sparse data, thereby limiting the burden to individual patients. Using this technique, continuous maturation profiles can be obtained on the basis of either fixed allometric scaling or comprehensive covariate analysis. While the models based on fixed allometric scaling resulted in complex maturation functions, all three paediatric population models for morphine yielded quite similar clearance predictions. The largest difference in clearance predictions between these three population models occurred in the first months of life, particularly in preterm neonates. Morphine clearance predictions by a physiologically based pharmacokinetic model were based on many continuous equations describing changes in underlying physiological processes across the full paediatric age range, and resulted in similar clearance predictions as well. However, preterm neonates could not be integrated in this model. In conclusion, the value of paediatric pharmacokinetic models is mostly dependent on clearance predictions and population concentration predictions, rather than on the individual description of data. For most pharmacokinetic models, however, the assessment of model performance was very limited and the accuracy of morphine clearance predictions as well as population concentration predictions was confirmed by formal evaluation and validation procedures for only one model.

Similar content being viewed by others
References
Coffman BL, Rios GR, King CD, Tephly TR. Human UGT2B7 catalyzes morphine glucuronidation. Drug Metab Dispos. 1997;25:1–4.
Court MH, Krishnaswamy S, Hao Q, Duan SX, Patten CJ, Von Moltke LL, et al. Evaluation of 3′-azido-3′-deoxythymidine, morphine, and codeine as probe substrates for UDP-glucuronosyltransferase 2B7 (UGT2B7) in human liver microsomes: specificity and influence of the UGT2B7*2 polymorphism. Drug Metab Dispos. 2003;31:1125–33.
Morrish GA, Foster DJR, Somogyi AA. Differential in vitro inhibition of M3G and M6G formation from morphine by (R)- and (S)-methadone and structurally related opioids. Br J Clin Pharmacol. 2006;61:326–35.
Osborne R, Thompson P, Joel S, Trew D, Patel N, Slevin M. The analgesic activity of morphine-6-glucuronide. Br J Clin Pharmacol. 1992;34:130–8.
Buck ML. Pharmacokinetic changes during extracorporeal membrane oxygenation: implications for drug therapy of neonates. Clin Pharmacokinet. 2003;42:403–17.
Bhatt-Meht V, Annich G. Sedative clearance during extracorporeal membrane oxygenation. Perfusion. 2005;20:309–15.
Roka A, Melinda KT, Vasarhelyi B, Machay T, Azzopardi D, Szabo M. Elevated morphine concentrations in neonates treated with morphine and prolonged hypothermia for hypoxic ischemic encephalopathy. Pediatrics. 2008;121:e844–9.
Lynn AM, Nespeca MK, Bratton SL, Shen DD. Intravenous morphine in postoperative infants: intermittent bolus dosing versus targeted continuous infusions. Pain. 2000;88:89–95.
Scott CS, Riggs KW, Ling EW, Fitzgerald CE, Hill ML, Grunau RV, et al. Morphine pharmacokinetics and pain assessment in premature newborns. J Pediatr. 1999;135:423–9.
Lynn A, Nespeca MK, Bratton SL, Strauss SG, Shen DD. Clearance of morphine in postoperative infants during intravenous infusion: the influence of age and surgery. Anesth Analg. 1998;86:958–63.
Dagan O, Klein J, Bohn D, Barker G, Koren G. Morphine pharmacokinetics in children following cardiac surgery: effects of disease and inotropic support. J Cardiothorac Vasc Anesth. 1993;7:396–8.
Dampier CD, Setty BN, Logan J, Ioli JG, Dean R. Intravenous morphine pharmacokinetics in pediatric patients with sickle cell disease. J Pediatr. 1995;126:461–7.
Tod M, Jullien V, Pons G. Facilitation of drug evaluation in children by population methods and modelling. Clin Pharmacokinet. 2008;47:231–43.
Anderson BJ, Holford NH. Mechanistic basis of using body size and maturation to predict clearance in humans. Drug Metab Pharmacokinet. 2009;24:25–36.
Mahmood I. Theoretical versus empirical allometry: facts behind theories and application to pharmacokinetics. J Pharm Sci. 2010;99:2927–33.
Dodds PS, Rothman DH, Weitz JS. Re-examination of the “3/4-law” of metabolism. J Theor Biol. 2001;209:9–27.
Agutter PS, Wheatley DN. Metabolic scaling: consensus or controversy? Theor Biol Med Model. 2004;1:13.
Bokma F. Evidence against universal metabolic allometry. Funct Ecol. 2004;18:184–7.
Glazier DS. Beyond the ‘3/4-power law’: variation in the intra- and interspecific scaling of metabolic rate in animals. Biol Rev. 2005;80:611–62.
White CR, Cassey P, Blackburn TM. Allometric exponents do not support a universal metabolic allometry. Ecology. 2007;88:315–23.
Kolokotrones T, Van S, Deeds EJ, Fontana W. Curvature in metabolic scaling. Nature. 2010;464:753–6.
Mahmood I. Prediction of drug clearance in children from adults: a comparison of several allometric methods. Br J Clin Pharmacol. 2006;61:545–57.
Mahmood I. Prediction of drug clearance in children: impact of allometric exponents, body weight, and age. Ther Drug Monit. 2007;29:271–8.
De Cock RF, Piana C, Krekels EH, Danhof M, Allegaert K, Knibbe CA. The role of population PK–PD modelling in paediatric clinical research. Eur J Clin Pharmacol. 2011;67:5–16.
Bouwmeester NJ, Anderson BJ, Tibboel D, Holford NH. Developmental pharmacokinetics of morphine and its metabolites in neonates, infants and young children. Br J Anaesth. 2004;92:208–17.
Van Dijk M, Bouwmeester NJ, Duivenvoorden HJ, Koot HM, Tibboel D, Passchier J, et al. Efficacy of continuous versus intermittent morphine administration after major surgery in 0–3-year-old infants; a double-blind randomized controlled trial. Pain. 2002;98:305–13.
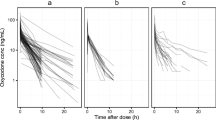
Krekels EH, van Hasselt JG, Tibboel D, Danhof M, Knibbe CA. Systematic evaluation of the descriptive and predictive performance of paediatric morphine population models. Pharm Res. 2011;28:797–811.
Anand KJ, Anderson BJ, Holford NH, Hall RW, Young T, Shephard B, et al. Morphine pharmacokinetics and pharmacodynamics in preterm and term neonates: secondary results from the NEOPAIN trial. Br J Anaesth. 2008;101:680–9.
Mahmood I. Evaluation of a morphine maturation model for the prediction of morphine clearance in children: how accurate is the predictive performance of the model? Br J Clin Pharmacol. 2011;71:88–94.
Knibbe CA, Krekels EH, van den Anker JN, DeJongh J, Santen GW, van Dijk M, et al. Morphine glucuronidation in preterm neonates, infants and children younger than 3 years. Clin Pharmacokinet. 2009;48:371–85.
Simons SH, van Dijk M, Van Lingen RA, Roofthooft D, Duivenvoorden HJ, Jongeneel N, et al. Routine morphine infusion in preterm newborns who received ventilatory support: a randomized controlled trial. JAMA. 2003;290:2419–27.
Krekels EH, DeJongh J, Van Lingen RA, Van der Marel CD, Choonara I, Lynn AM, et al. Predictive performance of a recently developed population pharmacokinetic model for morphine and its metabolites in new datasets of (preterm) neonates, infants and children. Clin Pharmacokinet. 2011;50:51–63.
Johnson TN, Rostami-Hodjegan A, Tucker GT. Prediction of the clearance of eleven drugs and associated variability in neonates, infants and children. Clin Pharmacokinet. 2006;45:931–56.
Edginton AN, Schmitt W, Willmann S. Development and evaluation of a generic physiologically based pharmacokinetic model for children. Clin Pharmacokinet. 2006;45:1013–34.
Fagerholm U. Prediction of human pharmacokinetics: evaluation of methods for prediction of hepatic metabolic clearance. J Pharm Pharmacol. 2007;59:803–28.
Edginton AN, Schmitt W, Voith B, Willmann S. A mechanistic approach for the scaling of clearance in children. Clin Pharmacokinet. 2006;45:683–704.
Krekels EH, Panoilia E, Neely M, Tibboel D, Capparelli E, Danhof M, et al. Maturation of glucuronidation; a system specific property [poster]. PAGE 20th meeting; 2011 Jun 7–10; Athens.
De Cock RFW, Allegaert K, Sherwin CMT, de Hoog M, van den Anker JN, Danhof M, et al. Maturation of GFR in preterm and term neonates reflected by clearance of different antibiotics [abstract no. 2096]. PAGE 20th meeting; 2011 Jun 7–10; Athens.
Knibbe CA, Danhof M. Individualized dosing regimens in children based on population PKPD modelling: are we ready for it? Int J Pharm. 2011;415:9–14.
Alcorn J, McNamara PJ. Ontogeny of hepatic and renal systemic clearance pathways in infants: part I. Clin Pharmacokinet. 2002;41:959–98.
Knibbe CA, Krekels EH, Danhof M. Advances in paediatric pharmacokinetics. Expert Opin Drug Metab Toxicol. 2011;7:1–8.
Hartley R, Green M, Quinn M, Levene MI. Pharmacokinetics of morphine infusion in premature neonates. Arch Dis Child. 1993;69:55–8.
Saarenmaa E, Neuvonen PJ, Rosenberg P, Fellman V. Morphine clearance and effects in newborn infants in relation to gestational age. Clin Pharmacol Ther. 2000;68:160–6.
Barrett DA, Barker DP, Rutter N, Pawula M, Shaw PN. Morphine, morphine-6-glucuronide and morphine-3-glucuronide pharmacokinetics in newborn infants receiving diamorphine infusions. Br J Clin Pharmacol. 1996;41:531–7.
Chay PC, Duffy BJ, Walker JS. Pharmacokinetic-pharmacodynamic relationships of morphine in neonates. Clin Pharmacol Ther. 1992;51:334–42.
Mikkelsen S, Feilberg VL, Christensen CB, Lundstrom KE. Morphine pharmacokinetics in premature and mature newborn infants. Acta Paediatr. 1994;83:1025–8.
Barrett DA, Elias-Jones AC, Rutter N, Shaw PN, Davis SS. Morphine kinetics after diamorphine infusion in premature neonates. Br J Clin Pharmacol. 1991;32:31–7.
Pokela ML, Olkkola KT, Seppala T, Koivisto M. Age-related morphine kinetics in infants. Dev Pharmacol Ther. 1993;20:26–34.
Choonara I, Lawrence A, Michalkiewicz A, Bowhay A, Ratcliffe J. Morphine metabolism in neonates and infants. Br J Clin Pharmacol. 1992;34:434–7.
Haberkern CM, Lynn AM, Geiduschek JM, Nespeca MK, Jacobson LE, Bratton SL, et al. Epidural and intravenous bolus morphine for postoperative analgesia in infants. Can J Anaesth. 1996;43:1203–10.
McRorie TI, Lynn AM, Nespeca MK, Opheim KE, Slattery JT. The maturation of morphine clearance and metabolism. Am J Dis Child. 1992;146:972–6.
Hain RD, Hardcastle A, Pinkerton CR, Aherne GW. Morphine and morphine-6-glucuronide in the plasma and cerebrospinal fluid of children. Br J Clin Pharmacol. 1999;48:37–42.
Mashayekhi SO, Ghandforoush-Sattari M, Routledge PA, Hain RD. Pharmacokinetic and pharmacodynamic study of morphine and morphine 6-glucuronide after oral and intravenous administration of morphine in children with cancer. Biopharm Drug Dispos. 2009;30:99–106.
Kopecky EA, Jacobson S, Joshi P, Koren G. Systemic exposure to morphine and the risk of acute chest syndrome in sickle cell disease. Clin Pharmacol Ther. 2004;75:140–6.
Robieux IC, Kellner JD, Coppes MJ, Shaw D, Brown E, Good C, et al. Analgesia in children with sickle cell crisis: comparison of intermittent opioids vs. continuous intravenous infusion of morphine and placebo-controlled study of oxygen inhalation. Pediatr Hematol Oncol. 1992;9:317–26.
Van Lingen RA. Pain assessment and analgesia in the newborn: an integrated approach [thesis]. Rotterdam: Erasmus University; 2000.
Van der Marel CD, Peters JW, Bouwmeester NJ, Jacqz-Aigrain E, van den Anker JN, Tibboel D. Rectal acetaminophen does not reduce morphine consumption after major surgery in young infants. Br J Anaesth. 2007;98:372–9.
Peters JW, Anderson BJ, Simons SH, Uges DR, Tibboel D. Morphine pharmacokinetics during venoarterial extracorporeal membrane oxygenation in neonates. Intensive Care Med. 2005;31:257–63.
Peters JW, Anderson BJ, Simons SH, Uges DR, Tibboel D. Morphine metabolite pharmacokinetics during venoarterial extra corporeal membrane oxygenation in neonates. Clin Pharmacokinet. 2006;45:705–14.
Hanekamp MN. Short and long term studies in neonates treated with extracorporeal membrane oxygenation (ECMO) [thesis]. Rotterdam: Erasmus University; 2005.
Vandenberghe H, Mac LS, Chinyanga H, Endrenyi L, Soldin S. Pharmacokinetics of intravenous morphine in balanced anesthesia: studies in children. Drug Metab Rev. 1983;14:887–903.
Dahlstrom B, Bolme P, Feychting H, Noack G, Paalzow L. Morphine kinetics in children. Clin Pharmacol Ther. 1979;26:354–65.
Olkkola KT, Maunuksela EL, Korpela R, Rosenberg PH. Kinetics and dynamics of postoperative intravenous morphine in children. Clin Pharmacol Ther. 1988;44:128–36.
Acknowledgments
This study was performed within the framework of Top Institute Pharma project number D2-104. The work of C.A.J. Knibbe is supported by the Innovational Research Incentives Scheme (Veni Grant, July 2006) of the Dutch Organization for Scientific Research NWO.
Conflict of interest
All authors declare no conflicts of interest that are directly relevant to the content of this review.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Krekels, E.H.J., Tibboel, D., Danhof, M. et al. Prediction of Morphine Clearance in the Paediatric Population. Clin Pharmacokinet 51, 695–709 (2012). https://doi.org/10.1007/s40262-012-0006-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-012-0006-9