Abstract
Background and Objective
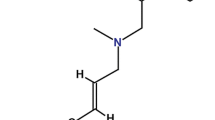
Naftifine, an allylamine, is highly effective against tinea pedis and exhibits relatively greater affinity to skin and nail beds, possibly due to its high lipophilicity. To study the efficacy and safety of naftifine 2% gel in an Indian population, a phase III multicentre double-blind, comparative, parallel-group study was conducted in comparison with miconazole 2% gel in patients with interdigital tinea pedis, with mild to moderate symptoms.
Patients and Methods
Patients presenting with mild to moderate signs and symptoms of interdigital tinea pedis and mycologically confirmed tinea infection were randomised to either naftifine hydrochloride 2% gel (n = 112) or miconazole 2% gel (n = 112) in 1:1 ratio. All patients were treated for 2 weeks with a follow-up of up to 12 weeks. Study evaluations were done at the end of 2, 6, and 12 weeks. The primary efficacy endpoint was the proportion of patients achieving clinical cure at week 6 (± 4 days) and secondary endpoints were the mycological cure at week 6 and week 12 and complete cure at week 12.
Results
At the end of week 6, clinical cure was 54.55% and 50.00% in the naftifine and miconazole groups (p = 0.4960), respectively, and it was increased to 78.18% and 76.36% in the naftifine and miconazole group (p = 0.7455) at the end of week 12. Mycological and clinical cure were similar in the naftifine and miconazole groups at week 6 and week 12. The safety and tolerability profiles of both treatments were similar.
Conclusions
Naftifine 2% gel was efficacious and safe for the treatment of mild to moderate interdigital tinea pedis. Its clinical effectiveness was comparable to that of miconazole 2% gel.
Trial Registration
Clinical Trials Registry of India: CTRI/2021/01/030753.




Similar content being viewed by others
References
Becker BA, Childress MA. Common foot problems: over-the-counter treatments and home care. Am Fam Physician. 2018;98(5):298–303.
Clebak KT, Malone MA. Skin infections. Prim Care. 2018;45(3):433–54.
Rajagopalan M, Inamadar A, Mittal A, Miskeen AK, Srinivas CR, Sardana K, Godse K, Patel K, Rengasamy M, Rudramurthy S, Dogra S. Expert consensus on the management of dermatophytosis in India (ECTODERM India). BMC Dermatol. 2018;18(1):6.
Ilkit M, Durdu M. Tinea pedis: the etiology and global epidemiology of a common fungal infection. Crit Rev Microbiol. 2015;41(3):374–88.
Nigam PK, Saleh D. Tinea Pedis. In: StatPearls. Treasure Island: StatPearls Publishing Copyright © 2021, StatPearls Publishing LLC. 2021.
Kaushik N, Pujalte GG, Reese ST. Superficial fungal infections. Prim Care. 2015;42(4):501–16.
Havlickova B, Czaika VA, Friedrich M. Epidemiological trends in skin mycoses worldwide. Mycoses. 2008;51(Suppl 4):2.
Seebacher C, Bouchara JP, Mignon B. Updates on the epidemiology of dermatophyte infections. Mycopathologia. 2008;166:335.
Ameen M. Epidemiology of superficial fungal infections. Clin Dermatol 2010; 28:197.
Oz Y, Qoraan I, Oz A, Balta I. Prevalence and epidemiology of tinea pedis and toenail onychomycosis and antifungal susceptibility of the causative agents in patients with type 2 diabetes in Turkey. Int J Dermatol. 2017;56(1):68–74.
Georgopoulos A, Petranyi G, Mieth H, et al. In vitro activity of naftifine, a new antifungal agent. Antimicrob Agents Chemother. 1981;19:386–9.
Jay E. Birnbaum, Pharmacology of the allylamines. J Am Acad Dermatol. 1990;23(4):782–5 (2).
NAFTIN®-naftifine hydrochloride gel. https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/019356s008,019599s014,204286s003lbl.pdf. Accessed 24 Nov 2022
Poojary SA. Topical antifungals: A review and their role in current management of dermatophytoses. Clin Dermatol Rev. 2017;1:S24–9.
Gupta AK, Albreski D, Del Rosso JQ, Konnikov N. The use of the new oral antifungal agents, itraconazole, terbinafine, and fluconazole to treat onychomycosis and other dermatomycoses. Curr Problems Dermatol. 2001;13:220–46.
Suchil P, Gei FM, Robles M, et al. Once- weekly oral dose of fluconazole 150 mg in the treatment of tineacorporis/cruris and cutaneous candidiasis. Clin Exp Dermatol. 1992;17:397–401.
Ngo HX, Garneau-Tsodikova S, Green KD. A complex game of hide and seek: the search for new antifungals. Medchemcomm. 2016;7:1285–306.
El Darouti MA, Raubaie SAL, Shandrashekhar CR, Sawaf MHAL, Movahadi GA. Double-blind randomized comparative study of naftifine cream and clotrimazole cream in the treatment of dermatophytosis. Intl J Dermatol. 1989;28(5):345–6.
Nada M, Hanafi S, Al-Omari H, et al. Naftifine versus miconazole/hydrocortisone in inflammatory dermatophyte infections. Int J Dermatol. 1994;33:570–2.
Acknowledgements
The authors would like to thank Hetero naftifine investigator group (Dr. G. Narsimha Rao Netha, Gandhi Hospital, Hyderabad; Dr. Devendra Kumar Omer, Nirmal Hospital, Jhansi; Dr. Bindiya Bansal, Maharaja Agrasen Super Specialty Hospital, Jaipur; Dr. Surendra Kumar, SMS Medical College and Hospital, Jaipur; Dr. Gaurav Patel, Hi Tech Multispecialty Hospital, Gandhinagar; Dr. Neha Sharma, Lotus Multispecialty Hospital, Ahmedabad; Dr. Neetu Sidana, Apex Hospitals, Jaipur and Dr. Rinkesh Dobariya, Global Hospital, Surat) for conducting this study. The authors would also like to thank all the study subjects for their valuable participation in this study, and the dedicated physicians, nurses, scientists and staff at each study site for their dedication and outstanding performance of clinical and laboratory study activities. Additionally, we would also like to thank Sudeshna Roy, Hetero Labs Limited, Hyderabad, for all editorial and submission support of our article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Funding for this study was provided by Hetero Labs Limited, Hyderabad, India.
Conflicts of Interest
Shubhadeep D. Sinha, Mohan Reddy Bandi, Sreenivasa Chary Sriramadasu, Abhilash Sankerneni, Muralidher Panapakam, Venkata Narayana Reddy Vemireddy and Srinivas Reddy Devireddy are the employees of Hetero Labs Limited. Ramya Vattipalli is a former employee of Hetero Labs Limited. All other authors have no conflict of interest to declare.
Availability of data and material
The data supporting the results reported in the article, which are not available in the article, are available on request if appropriate.
Ethics Approval
This study was conducted after approval by the institutional review board/ethics committee at each participating site (Supplementary Material) and in accordance with good clinical practice (GCP) guidelines issued by the Central Drugs Standard Control Organization (CDSCO), New Drugs and Clinical Trials Rules (2019), Indian Council of Medical Research (ICMR) and ethical guidelines for biomedical research on human patients. This trial was performed with the ethical principles that have their origin in the Declaration of Helsinki (2013), that are consistent with GCP in accordance with International Conference on Harmonization guidelines (ICH-GCP E6), the applicable regulatory requirements, and applicable standard operating procedures (SOPs).
Consent to Participate
All patients signed written informed consent prior to the initiation of study-related procedures for screening.
Consent for Publication
Not Applicable.
Code Availability
Not Applicable.
Author Contributions
Conceptualisation: SDS and SCS; Methodology: SCS and AS; Formal analysis and investigation: AR, RKK, S.S, SH, MP, VNRV and MRB; Writing—original draft preparation: SRD; Writing—review and editing: SCS, SRD, SDS; Supervision: SDS, SCS, and MRB.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sinha, S.D., Rajamma, A., Bandi, M.R. et al. Efficacy and Safety of Naftifine Hydrochloride 2% Gel in Interdigital Tinea Pedis: A Phase III Randomised, Double-Blind, Parallel-Group, Active-Controlled Study in Indian Adult Patients. Clin Drug Investig 43, 565–574 (2023). https://doi.org/10.1007/s40261-023-01288-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40261-023-01288-1