Abstract
Background and Objectives
Novel immunotherapy-based combination treatments have drastically improved clinical outcomes for previously untreated patients with advanced/metastatic renal cell carcinoma (aRCC). This study aimed to assess the temporal trends in grade 3/4 adverse event (AE) rates and associated costs of nivolumab plus cabozantinib combination therapy versus sunitinib monotherapy in previously untreated patients with aRCC.
Methods
Individual patient data from the CheckMate 9ER trial (nivolumab plus cabozantinib: N = 320; sunitinib: N = 320) were used to calculate the proportion of patients experiencing grade 3/4 AEs. AE unit costs were obtained from the United States (US) 2017 Healthcare Cost and Utilization Project (HCUP) and inflated to 2020 US dollars. Per-patient-per-month (PPPM) all-cause and treatment-related grade 3/4 AE costs over 18-months, temporal trends, and top drivers of AE costs were evaluated in both treatment arms.
Results
Overall, the proportion of patients experiencing grade 3/4 AEs decreased over time, with the highest rates observed in the first 3 months for the nivolumab plus cabozantinib and sunitinib arms. Compared with sunitinib, nivolumab plus cabozantinib was associated with consistently lower average all-cause AE costs PPPM [month 3: $2021 vs. $3097 (p < 0.05); month 6: $1653 vs. $2418 (p < 0.05); month 12: $1450 vs. $1935 (p > 0.05); month 18: $1337 vs. $1755 (p > 0.05)]. Over 18 months, metabolism and nutrition disorders ($244), laboratory abnormalities ($182), and general disorders and administration site conditions ($122) were the costliest all-cause PPPM AE categories in the nivolumab plus cabozantinib arm, and laboratory abnormalities ($443), blood and lymphatic system disorders ($254), and metabolism and nutrition disorders ($177) were the costliest in the sunitinib arm. Trends of treatment-related AE costs were consistent with all-cause AE costs.
Conclusions
Nivolumab plus cabozantinib was associated with lower costs of grade 3/4 AE management PPPM than sunitinib, which accumulated over the 18-month study period.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
This study assessed the temporal trends of grade 3/4 adverse event (AE) rates and the associated costs of nivolumab plus cabozantinib combination therapy versus sunitinib monotherapy using individual patient-level data from the pivotal CheckMate 9ER trial. |
Nivolumab plus cabozantinib was associated with lower all-cause and treatment-related grade 3/4 AE costs compared with sunitinib, despite the higher rate of AEs observed among patients treated with nivolumab plus cabozantinib in the CheckMate 9ER trial. |
Cost savings appeared to be most prominent within the first month of treatment initiation. |
1 Introduction
In the United States (US), renal cell carcinoma (RCC) accounts for 4.2% of all cancer diagnoses [1], and 30% of patients are estimated to have advanced or metastatic RCC (aRCC) at the time of diagnosis [2]. This advanced stage is associated with a 5-year survival rate of 13% [3]. Since their approval by the US Food and Drug Administration (FDA) in 2006, targeted therapies, such as the tyrosine kinase inhibitor (TKI) sunitinib, became the standard of care in patients with previously untreated aRCC [4, 5]. Inhibition of the proangiogenic vascular endothelial growth factor (VEGF) pathway by the TKI is thought to normalize tumor vasculature, facilitate lymphocyte trafficking, and ultimately promote lymphocyte infiltration of tumors [6]. However, nearly half of patients with aRCC eventually stop treatment with TKI monotherapy and experience progression around 1 year after receiving treatment [7,8,9].
Recently, the FDA approved several immuno-oncology (IO)-based combinations for the management of treatment-naïve patients with aRCC, including nivolumab plus ipilimumab, avelumab plus axitinib, pembrolizumab plus axitinib, nivolumab plus cabozantinib, and pembrolizumab plus lenvatinib [10,11,12,13,14]. Immune checkpoint inhibition by anti–programmed cell death 1 (anti-PD-1) works by promoting T cell priming, activation, and finally T cell-mediated tumor cell death [6]. The combination of nivolumab (an anti-PD-1 checkpoint inhibitor) plus cabozantinib, a TKI, was approved by the FDA for treatment-naïve patients with aRCC across risk groups in 2021 based on the results of the CheckMate 9ER trial (NCT03141177) [13]. This randomized, open-label, phase III clinical trial demonstrated that patients treated with nivolumab plus cabozantinib showed a statistically significant improvement compared with those who received sunitinib monotherapy in terms of progression-free survival, probability of overall survival, and objective response rate [15]. Among patients in the as-treated population—patients who received at least one dose of trial treatments—all-cause grade 3 or higher adverse events (AEs) occurred in 75.3% of patients in the nivolumab plus cabozantinib arm and in 70.6% of patients in the sunitinib arm. Grade 3/4 treatment-related AEs occurred in 60.6% and 50.9% of patients treated with nivolumab plus cabozantinib and sunitinib, respectively [15, 16].
The approval of immune checkpoint inhibitors over the last decade has transformed the landscape of care for patients with aRCC. Huo et al. previously estimated the total costs for nivolumab plus cabozantinib versus sunitinib over 12 months, including drug administration and treatment-related AE costs, where differences were primarily driven by the use of dual agents over single agent in the first-line setting [17]. However, the financial impact on toxicity management has not been previously well characterized. Despite their superior efficacy, combination therapies with IO are associated with AEs that starkly differ from those related to previous standards of care [17,18,19]. Understanding the AE profile, temporal trends, and associated costs for new immune checkpoint inhibitors approved for aRCC can better help characterize the associated economic burden and ensure optimal adherence and inform decision-making for patients, payers, and healthcare providers. As such, this study utilized the CheckMate 9ER trial data to assess the temporal trends in grade 3/4 AE rates and the associated costs of nivolumab plus cabozantinib combination therapy and sunitinib monotherapy in patients with previously untreated aRCC.
2 Methods
2.1 Data Sources
Individual patient-level data (IPD) from the CheckMate 9ER trial (data cutoff date: March 30, 2020; median follow-up: 18.1 months) were used to estimate all-cause and treatment-related grade 3/4 AE rates associated with nivolumab plus cabozantinib and sunitinib [15]. In the trial, patients with previously untreated aRCC were stratified according to the International Metastatic Renal Cell Carcinoma Database Consortium score, geographic region, and tumor expression of programmed death-ligand 1 (PD-L1). Patients were randomly assigned 1:1 to receive either nivolumab 240 mg every 2 weeks in combination with cabozantinib 40 mg daily or sunitinib 50 mg daily for the first 4 weeks in repeating 6-week cycles [15]. The analysis assessed patients from the as-treated population (i.e., patients who received at least one dose of trial treatments), which included 320 patients treated with nivolumab plus cabozantinib and 320 patients treated with sunitinib. Grade 3/4 AEs occurring on treatment and within the 30 days after the last dose of each treatment were included in the analysis. Each AE was defined based on the AE type, body system organ class, toxicity grade, and date of onset.
The US 2017 Healthcare Cost and Utilization Project (HCUP) National Inpatient Database was used to obtain the unit cost of each grade 3/4 AE. Developed through a Federal-State-Industry partnership and sponsored by the Agency for Healthcare Research and Quality (AHRQ), the HCUP database is a family of healthcare databases with a national information resource of encounter-level healthcare data (HCUP Partners) [20,21,22]. Since the Common Terminology Criteria for Adverse Events (CTCAE) version 4.0 defines patients with grade 3 AEs as those potentially requiring hospitalization or prolonged hospitalization and patients with grade 4 AEs as those requiring urgent intervention, this study used inpatient costs at the national level from the HCUP database to estimate the unit costs associated with each grade 3/4 AE. The unit cost of each grade 3/4 AE or laboratory abnormality was obtained based on the corresponding International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM) diagnosis code. For infrequent AEs (i.e., AEs with a rate < 1.5%) and AEs for which the unit costs were unavailable, unit costs were assumed to be the same as the unit costs of similar AEs under the same CTCAE category, the average of that type of disorder, or the average of all listed unit costs. All costs were inflated from 2017 US dollars (USD) to 2020 USD using an inflation factor of 1.0793 based on the Consumer Price Index for all urban consumers in medical care [23].
2.2 Study Outcomes and Statistical Analyses
Outcomes evaluated for the nivolumab plus cabozantinib and sunitinib monotherapy arms included temporal trends in grade 3/4 AE rates, per-patient grade 3/4 AE costs, temporal trends of grade 3/4 AE costs, and top drivers of grade 3/4 AE costs. For this study, all analyses were focused on the first 18 months to match the median follow-up of 18.1 months for overall survival and to ensure sufficient sample sizes (for example, the sample size is less than 50 patients for the sunitinib arm for time points beyond 18 months in the current data cut). All-cause and treatment-related grade 3/4 AE costs were assessed separately. All analyses were performed using SAS V.9.4 (SAS Institute).
2.2.1 Temporal Trends of Grade 3/4 AE Rates for Nivolumab plus Cabozantinib and Sunitinib
The proportion of patients with all-cause or treatment-related grade 3/4 AEs each month was calculated over 18 months among the as-treated population. This was calculated as the number of patients experiencing a new AE divided by the number of patients at risk during each month.
2.2.2 Temporal Trends of Grade 3/4 AE Costs for Nivolumab plus Cabozantinib and Sunitinib
The temporal trends of all-cause and treatment-related grade 3/4 AE costs associated with nivolumab plus cabozantinib and sunitinib were assessed over 18 months. The cost for a given AE was calculated by multiplying its unit cost by its frequency. The per-patient-per-month (PPPM) all-cause grade 3/4 AE costs per patient were calculated as total grade 3/4 all-cause AE costs during each month divided by the sum of patient-months at risk during the month. The temporal trend of PPPM all-cause grade 3/4 AE costs of nivolumab plus cabozantinib and sunitinib were assessed using 4-order polynomial trendlines. The same methods were used to assess temporal trends of treatment-related grade 3/4 AE costs.
Total all-cause and treatment-related grade 3/4 AE costs associated with each treatment arm were calculated for grade 3/4 AEs occurring within 3, 6, 12, and 18 months of the first dose of the randomized regimens by summing PPPM grade 3/4 AE costs for the relevant arm during the designated study period (i.e., 3, 6, 12, and 18 months). Statistical comparisons of PPPM AE costs between the nivolumab plus cabozantinib and sunitinib arms were conducted using Wilcoxon rank-sum tests, and statistical significance was assessed at the 5% level.
Lastly, cumulative all-cause grade 3/4 AE costs were calculated by summing the PPPM all-cause grade 3/4 AE costs incrementally each month over the 18-month period.
2.2.3 Top Drivers of Grade 3/4 AE Costs for Nivolumab plus Cabozantinib and Sunitinib
Top drivers of AE costs associated with nivolumab plus cabozantinib and sunitinib were evaluated based on the PPPM all-cause and treatment-related grade 3/4 AE costs per AE category (e.g., blood and lymphatic system disorders, gastrointestinal disorders), which were defined by the CTCAE, version 4.0 [24]. PPPM all-cause and treatment-related AE costs per AE category were calculated by dividing the sum of grade 3/4 AE costs within each AE category by the number of patient-months in each treatment arm over 18 months.
3 Results
3.1 Temporal Trends of Grade 3/4 AE Rates for Nivolumab plus Cabozantinib and Sunitinib
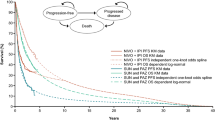
Over the 18 months, the proportion of patients experiencing all-cause grade 3/4 AEs was similar between patients treated with nivolumab plus cabozantinib versus those treated with sunitinib. The highest proportion of patients who experienced all-cause grade 3/4 AEs was observed in the first month for both treatment arms at rates of 20% and 33% for nivolumab plus cabozantinib and sunitinib, respectively. After 1 year on treatment, the proportion of patients who experienced all-cause grade 3/4 AEs decreased from 20 to 11% (Δ = 45%) for the nivolumab plus cabozantinib arm and from 33 to 11% (Δ = 67%) in the sunitinib arm. The proportion ranged from 5 to 10% for the remaining months in the assessed 18-month period for both arms (Fig. 1).
Proportion of patients experiencing all-cause and treatment-related grade 3/4 AEs each month in CheckMate 9ER, as-treated population. Analyses were conducted among patients in the as-treated population who received at least 1 dose of the study drug in CheckMate 9ER. Percentages were calculated as the number of patients with any all-cause/treatment-related grade 3/4 AEs divided by the number of patients at risk during the given month. Patients at risk were defined as patients who were still on treatment during each month. Four-order polynomial trendlines fitted by a multiple regression were added to the figure to present the smoothed temporal trend of monthly AE costs by treatment arm. AE adverse event, N+C nivolumab plus cabozantinib, SUN sunitinib
The same trend persisted among patients who experienced treatment-related grade 3/4 AEs. The highest proportion of patients was observed in the first month among those treated with each regimen: (nivolumab plus cabozantinib: 16%; sunitinib: 26%). After 1 year on treatment, the proportion of patients who experienced treatment-related grade 3/4 AEs decreased from 16 to 7% (Δ = 57%) for those treated with nivolumab plus cabozantinib. The proportion of patients who experienced treatment-related grade 3/4 AEs in the sunitinib arm decreased from 26 to 10% (Δ = 62%) at 1 year following treatment initiation (Fig. 1). For the remaining months in the study period, the proportion ranged from 2 to 5% for patients treated with nivolumab plus cabozantinib and below 10% for those treated with sunitinib.
3.2 Temporal Trends of Grade 3/4 AE Costs for Nivolumab plus Cabozantinib and Sunitinib
3.2.1 Average Monthly Grade 3/4 AE Costs over the 18-Month Period
The monthly temporal trends of all-cause grade 3/4 AE costs per patient are provided in Fig. 2. Both treatment arms experienced an overall decreasing trend in costs throughout the study period, although the monthly costs varied. Compared to sunitinib, treatment with nivolumab plus cabozantinib was generally associated with lower PPPM all-cause grade 3/4 AE costs each month over the first 6 months of treatment; costs remained similar between the two arms thereafter. Specifically, the highest PPPM cost associated with nivolumab plus cabozantinib occurred in the second month ($2356) and decreased 20% by the third month. The PPPM all-cause grade 3/4 AE costs further decreased to $1264 (Δ = 46%) 1 year following treatment initiation. For the remaining 6 months in the study period, PPPM all-cause AE costs ranged from $683 to $1422. In the sunitinib monotherapy arm, the highest PPPM cost was $4481 in the first month, which was more than double the cost observed in the first month of treatment with nivolumab plus cabozantinib ($1827) and higher than the PPPM costs observed in patients treated with nivolumab plus cabozantinib at any point in time. The all-cause grade 3/4 AE cost for sunitinib decreased by 53% to $2084 in the second month, and ranged from $430 to $2614 for the remainder of the study period (i.e., months 3–18). In 10 out of 18 months, patients treated with nivolumab plus cabozantinib had lower PPPM all-cause grade 3/4 AE costs compared to those treated with sunitinib.
PPPM all-cause and treatment-related grade 3/4 AE costs for patients in CheckMate 9ER, as-treated population. Analyses were conducted among patients in the as-treated population who received at least 1 dose of the study drug in CheckMate 9ER. Monthly AE costs were calculated as total all-cause/treatment-related grade costs during each month divided by the sum of all patients’ medication exposure time occurring during each month. Four-order polynomial trendlines fitted by a multiple regression were added to the figure to present the smoothed temporal trend of monthly AE costs by treatment arm. AE adverse event, N+C nivolumab plus cabozantinib, PPPM per-patient-per-month, SUN sunitinib, USD United States dollars
The monthly temporal trends of treatment-related grade 3/4 AE costs per patient were similar to those observed with respect to all-cause grade 3/4 AEs (Fig. 2). Specifically, the highest PPPM cost for nivolumab plus cabozantinib treatment occurred in the second month ($1885 per patient) and decreased by 22% by the third month. After 1 year on treatment, the PPPM treatment-related grade 3/4 AE cost decreased by 63% to $689. For the remaining months of the study period, PPPM treatment-related grade 3/4 AE costs remained relatively constant, ranging from $277 to $593. In the sunitinib arm, the highest PPPM cost was $3165 in the first month, which was more than twice as high as costs observed in the first month of treatment with nivolumab plus cabozantinib ($1338). The treatment-related grade 3/4 AE cost decreased by 76% to $767 in the second month and ranged from $303 to $1881 for the remainder of the study period. In 13 out of 18 months, patients treated with nivolumab plus cabozantinib had lower PPPM treatment-related grade 3/4 AE costs compared to those treated with sunitinib.
3.2.2 Grade 3/4 AE Costs over Time for Nivolumab plus Cabozantinib and Sunitinib
The PPPM all-cause and treatment-related grade 3/4 AE costs in the nivolumab plus cabozantinib and sunitinib arms among all patients with aRCC included in the study are provided in Table 1. Patients who received nivolumab plus cabozantinib incurred lower PPPM all-cause grade 3/4 AE costs compared to patients treated with sunitinib during all assessment periods (month 3: $2021 vs. $3097; month 6: $1653 vs. $2418; month 12: $1450 vs. $1935; month 18: $1337 vs. $1755). The difference between the two arms was statistically significant (p < 0.05) at month 3 and at month 6. Patients who received nivolumab plus cabozantinib also incurred lower PPPM treatment-related grade 3/4 AE costs compared to patients treated with sunitinib during all assessment periods (month 3: $1503 vs. $1963; month 6: $1212 vs. $1584; month 12: $979 vs. $1253; month 18: $860 vs. $1153), although these results were not statistically significant.
3.2.3 Cumulative Average Grade 3/4 AE Costs over the 18-Month Period
The monthly temporal trends of cumulative all-cause and treatment-related grade 3/4 AE costs per patient are provided in Fig. 3, respectively. Treatment with nivolumab plus cabozantinib was consistently associated with lower cumulative average all-cause and treatment-related grade 3/4 AE costs compared with sunitinib at each month in the 18-month study period. The cumulative average all-cause grade 3/4 AE costs over 6, 12, and 18 months for patients treated with nivolumab plus cabozantinib versus sunitinib were $9819 versus $13,682, $17,032 versus $20,670, and $22,342 versus $25,770, respectively. The absolute cost differences of cumulative average all-cause and treatment-related grade 3/4 AE costs between the nivolumab plus cabozantinib and sunitinib arms consistently ranged from $2382 to $4182 and $709 to $3526, respectively, throughout the 18-month period. The cumulative average treatment-related grade 3/4 AE costs over the entire 18-month study period were 20% lower for patients treated with nivolumab plus cabozantinib versus sunitinib: $13,812 versus $17,336.
Cumulative per-patient all-cause and treatment-related grade 3/4 AE costs for patients in CheckMate 9ER, as-treated population. Analyses were conducted among patients in the as-treated population who received at least 1 dose of the study drug in CheckMate 9ER. Cumulative all-cause grade 3/4 AE costs at each month were calculated by summing the PPPM all-cause grade 3/4 AE costs per patient in all previous months. The same method was followed for cumulative treatment-related grade 3/4 AE costs. Four-order polynomial trendlines fitted by a multiple regression were added to the figure to present the smoothed temporal trend of monthly AE costs by treatment arm. AE adverse event; N+C nivolumab plus cabozantinib, PPPM per-patient-per-month, SUN sunitinib, USD United States dollars
3.3 Top Drivers of Grade 3/4 AE Costs for Nivolumab plus Cabozantinib and Sunitinib
All-cause grade 3/4 AE costs by AE category PPPM over 18 months are presented in Fig. 4. The top three AE categories contributing to the negative cost differences between the nivolumab plus cabozantinib versus sunitinib arms were laboratory abnormalities ($182 vs. $443, Δ = − $261), blood and lymphatic system disorders ($41 vs. $254, Δ = − $213), and general disorders and administration site conditions ($122 vs. $157, Δ = − $35). Metabolism and nutrition disorders ($244), laboratory abnormalities ($182), and general disorders and administration site conditions ($122) were the top three AE categories contributing to total all-cause grade 3/4 AE costs for patients in the nivolumab plus cabozantinib arm. For patients in the sunitinib arm, laboratory abnormalities ($443), blood and lymphatic system disorders ($254), and metabolism and nutrition disorders ($177) were the top three AE categories contributing to the total all-cause grade 3/4 AE costs.
PPPM all-cause and treatment-related grade 3/4 AE costs by AE category over 18 months for patients in CheckMate 9ER, as-treated population. Analyses were conducted among patients in the as-treated population who received at least 1 dose of the study drug in CheckMate 9ER. PPPM grade 3/4 AE costs for each AE category over 18 months were calculated by summing grade 3/4 AE costs within each AE category over 18 months. AEs were graded according to the CTCAE, version 4.0 [24]. Legends for all-cause and treatment-related AEs with PPPM AE costs ≤ $100 for the 18-month period are not shown. This includes ear and labyrinth disorders, eye disorders, immune system disorders, psychiatric disorders, reproductive system and breast disorders, and surgical and medical procedures. AE adverse event, CTCAE Common Terminology Criteria for Adverse Events, N+C nivolumab plus cabozantinib, PPPM per-patient-per-month, SUN sunitinib, USD United States dollars
Treatment-related grade 3/4 AE costs by AE category PPPM over 18 months are also presented in Fig. 4. The top three categories driving the negative difference in AE costs for treatment-related grade 3/4 AEs among patients receiving nivolumab plus cabozantinib versus sunitinib differed from the drivers of all-cause grade 3/4 AE costs, and included laboratory abnormalities ($144 vs. $393, Δ = − $249), blood and lymphatic system disorders ($32 vs. $225, Δ = − $193), and vascular disorders ($77 vs. $112, Δ = − $35). Metabolism and nutrition disorders ($166), laboratory abnormalities ($144), and general disorders and administration site conditions ($83) were the top three AE categories contributing to total treatment-related grade 3/4 AE costs for patients in the nivolumab plus cabozantinib arm. For patients in the sunitinib arm, laboratory abnormalities ($393), blood and lymphatic system disorders ($225), and vascular disorders ($112) were the top three AE categories contributing to total treatment-related grade 3/4 AE costs.
4 Discussion
Using IPD from the CheckMate 9ER clinical trial, this study assessed the grade 3/4 AE rates and costs associated with nivolumab plus cabozantinib combination therapy versus sunitinib monotherapy from a US payer’s perspective. The combination of nivolumab plus cabozantinib is associated with a unique safety profile involving immune-related AEs, which necessitate the development and implementation of AE-specific management plans [25]. This study fills an important gap in the literature by accurately capturing the temporal trends of AEs experienced by patients while on treatment with nivolumab plus cabozantinib combination therapy versus sunitinib monotherapy, as well as the associated costs, which were assessed at multiple time points during the trial.
The present analysis found that nivolumab plus cabozantinib was associated with lower all-cause and treatment-related grade 3/4 AE costs compared with sunitinib, with the all-cause AE cost difference between the two treatment arms being $1076, $765, $485, and $418 PPPM at months 3, 6, 12, and 18, respectively. By observing monthly trends, the AE cost savings associated with nivolumab plus cabozantinib compared to sunitinib appeared to be the most prominent within the first month of treatment initiation, such that all-cause and treatment-related grade 3/4 AE costs for sunitinib were more than twice as high as the respective costs for nivolumab plus cabozantinib at month 1. This may be partially explained by the lower starting dose of cabozantinib when used in combination (40 mg vs. the full dose of 60 mg when used as monotherapy) versus the full starting dose of sunitinib (50 mg), as most of the AEs at early time points are related to TKIs. At month 2, all-cause and treatment-related grade 3/4 AE costs for nivolumab plus cabozantinib were higher than the corresponding costs for sunitinib. However, cumulatively, total all-cause and treatment-related grade 3/4 AE costs were consistently higher for sunitinib than nivolumab plus cabozantinib at each month over the entire 18-month period, suggesting an accumulation of cost savings over time. Over 18 months, the cumulative all-cause and treatment-related grade 3/4 AE costs were $3428 and $3524 less per patient, respectively, for those treated with nivolumab plus cabozantinib compared to sunitinib. In addition, a similar analysis found that patients who received nivolumab plus ipilimumab also had lower average per-patient all-cause grade at 12 months ($15,170 vs. $20,342) compared to sunitinib [26]. Together, these results highlight the value of nivolumab-based combination therapies for the first-line treatment of aRCC compared to the current standard of care in the US.
Both treatment arms experienced an overall decreasing trend in monthly grade 3/4 AE rates and costs per patient throughout the 18-month study period. The decreasing trend in AE rates was more moderate in the nivolumab plus cabozantinib arm than the sunitinib arm, possibly due to the different mechanisms of action between the two treatments and potential for a delayed immune-related AE [6]. The highest AE costs occurred at month 2 for the nivolumab plus cabozantinib arm and at month 1 for the sunitinib arm. Similarly, in CheckMate 214, the highest AE costs occurred at month 3 for nivolumab plus ipilimumab and at month 1 for sunitinib [26]. Similar onset times of AEs were also reported for other targeted aRCC therapies, such as sorafenib, and other studies of sunitinib, in which most treatment-related AEs developed shortly within the first treatment cycle (6 weeks) and decreased with each subsequent cycle [27, 28]. One trial conjectured that patients with aRCC who did not experience common treatment-related AEs earlier during the course of treatment of sorafenib may be unlikely to develop them later [27]. However, it is unclear whether the onset and course of each type of AEs associated with IO-based combinations differ from targeted therapies. Future studies with comparative data are needed to address this question and determine whether these characteristics have an impact on the associated costs.
The study also contributes to our understanding of the cost drivers of the AEs associated with these two treatments. Investigations related to abnormalities in laboratory results (such as decreased platelet count, decreased neutrophil count, and increased lipase) were some of the most important drivers of all-cause and treatment-related grade 3/4 AE costs in the nivolumab plus cabozantinib arm, and contributed the highest all-cause and treatment-related grade 3/4 AE costs in the sunitinib arm [26]. Managing laboratory abnormalities can be resource-intensive and is associated with high costs. For example, previous cost-effectiveness analyses in treatment-naïve aRCC patients showed that the costs of managing grade 3/4 thrombocytopenia (i.e., decreased platelet count), amounted to more than $4000 per event [29]. In addition, the different mechanism of actions of nivolumab plus cabozantinib and sunitinib might contribute to the different cost drivers observed in this study [30,31,32,33,34,35]. While there are many contributing factors to treatment-decision making, the safety profile of aRCC treatments and associated cost is one integral component of that process. Further studies are warranted to assess how cost drivers in treatment-naïve aRCC patients may impact treatment decision-making in clinical practice.
It is worth noting that while the overall grade 3/4 AE rates were slightly higher for patients treated with nivolumab plus cabozantinib (all-cause: 75.3%; treatment-related: 60.6%) compared with sunitinib (all-cause: 70.6%; treatment-related: 50.9%) [15], the estimated PPPM costs associated with nivolumab plus cabozantinib treatment and incidence AE rates adjusting for exposure time were lower, due to the longer exposure to nivolumab plus cabozantinib than sunitinib in the trial. The median treatment duration for patients treated with nivolumab plus cabozantinib and sunitinib was 14.3 months and 9.2 months, respectively. At the time of database lock, the proportion of patients who discontinued treatment was 44.4% in the nivolumab plus cabozantinib arm versus 71.3% in the sunitinib arm, with disease progression being the primary reason for discontinuation in both arms [15]. The longer exposure time may also be associated with the superior overall survival of nivolumab plus cabozantinib. Thus, it is important to consider treatment exposure in the interpretation of the AE incidence rates and costs. As illustrated by this analysis, slightly higher overall grade 3/4 AE rates associated with nivolumab plus cabozantinib treatment can indeed be mainly attributed to the longer treatment duration. This may in turn reflect superior efficacy outcomes versus sunitinib, and ultimately do not translate to higher PPPM AE costs. The results of this study serve to further emphasize the benefit of nivolumab plus cabozantinib over sunitinib, where nivolumab plus cabozantinib is associated with lower costs related to AE management in addition to the superior efficacy outcomes.
The study was subject to a number of limitations. First, as grade 1 or 2 AEs are expected to be of low-cost impact, the current analysis focused on costs associated with grade 3/4 AEs and may have consequently underestimated the total AE costs in both treatment arms. Second, each grade 3/4 AE was assumed to incur the cost of a hospitalization, which was obtained from the HCUP. Thus, the unit costs may not reflect the true costs incurred during the trial and may be subject to measurement error. In addition, some grade 3/4 AEs might not require a hospitalization and the unit cost may overestimate the true cost for such AEs. Third, the study focused on the rate of new AEs that occurred during each time period and did not consider the duration of a grade 3/4 AE; further studies are warranted to assess the cost impact attributed to the chronic nature of certain AEs. Finally, patients with previously untreated aRCC in a real-world setting may have different clinical profiles than those included in the CheckMate 9ER trial, which could influence the observed AE toxicity profile associated with these therapies.
5 Conclusions
The result of this cost analysis suggests that the IO + TKI combination of nivolumab plus cabozantinib is associated with lower long-term management costs related to AEs compared with sunitinib monotherapy among patients with aRCC. The AE cost savings associated with nivolumab plus cabozantinib were the most prominent within the first month of initiating treatment and continued to accumulate over the assessed trial period. The rates of all-cause and treatment-related grade 3/4 AEs and their associated costs declined in both nivolumab plus cabozantinib and sunitinib arms over the 18-month follow-up period, with a more moderate rate of decline for nivolumab plus cabozantinib. In addition to the superior clinical efficacy observed in the CheckMate 9ER trial, the results from this analysis indicate that nivolumab plus cabozantinib is associated with lower costs of AE management compared with sunitinib despite the higher rate of AEs observed among patients treated with nivolumab plus cabozantinib in the CheckMate 9ER trial.
References
Padala SA, Barsouk A, Thandra KC, Saginala K, Mohammed A, Vakiti A, et al. Epidemiology of renal cell carcinoma. World J Oncol. 2020;11(3):79–87. https://doi.org/10.14740/wjon1279.
Levitin M, Ofori J, Shin WJ, Huang J, Daly M, Cao D, et al. Radiation and checkpoint inhibitor immunotherapy lead to long term disease control in a metastatic RCC patient with brain metastases. Front Oncol. 2020. https://doi.org/10.3389/fonc.2020.566070.
National Cancer Institute, Surveillance, Epidemiology, and End Results Program (SEER): Cancer Stat Facts: Kidney and Renal Pelvis Cancer. 2020. https://seer.cancer.gov/statfacts/html/kidrp.html. Accessed 13 Jan 2021.
Motzer RJ, Tannir NM, McDermott DF, Aren Frontera O, Melichar B, Choueiri TK, et al. Nivolumab plus Ipilimumab versus Sunitinib in advanced renal-cell carcinoma. N Engl J Med. 2018;378(14):1277–90. https://doi.org/10.1056/NEJMoa1712126.
Motzer RJ, Hutson TE, Tomczak P, Michaelson MD, Bukowski RM, Rixe O, et al. Sunitinib versus interferon alfa in metastatic renal-cell carcinoma. N Engl J Med. 2007;356(2):115–24. https://doi.org/10.1056/NEJMoa065044.
George S, Rini BI, Hammers HJ. Emerging role of combination immunotherapy in the first-line treatment of advanced renal cell carcinoma: a review. JAMA Oncol. 2019;5(3):411–21. https://doi.org/10.1001/jamaoncol.2018.4604.
Motzer RJ, Hutson TE, Cella D, Reeves J, Hawkins R, Guo J, et al. Pazopanib versus sunitinib in metastatic renal-cell carcinoma. N Engl J Med. 2013;369(8):722–31. https://doi.org/10.1056/NEJMoa1303989.
Rini BI, Hutson TE, Figlin RA, Lechuga MJ, Valota O, Serfass L, et al. Sunitinib in patients with metastatic renal cell carcinoma: clinical outcome according to international metastatic renal cell carcinoma database consortium risk group. Clin Genitourin Cancer. 2018;16(4):298–304. https://doi.org/10.1016/j.clgc.2018.04.005.
Maroun R, Mitrofan L, Benjamin L, Nachbaur G, Maunoury F, Le Jeunne P, et al. Real life patterns of care and progression free survival in metastatic renal cell carcinoma patients: retrospective analysis of cross-sectional data. BMC Cancer. 2018;18(1):214. https://doi.org/10.1186/s12885-018-4117-z.
US Food & Drug Administration: FDA approves nivolumab plus ipilimumab combination for intermediate or poor-risk advanced renal cell carcinoma. 2018. https://www.fda.gov/Drugs/InformationOnDrugs/ApprovedDrugs/ucm604685.htm. Accessed 5 Apr 2020.
US Food & Drug Administration: FDA approves avelumab plus axitinib for renal cell carcinoma. 2019. https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-avelumab-plus-axitinib-renal-cell-carcinoma. Accessed 14 Mar 2021.
US Food & Drug Administration: FDA approves pembrolizumab plus axitinib for advanced renal cell carcinoma. 2019. https://www.fda.gov/drugs/drug-approvals-and-databases/fda-approves-pembrolizumab-plus-axitinib-advanced-renal-cell-carcinoma. Accessed 26 May 2021.
US Food & Drug Administration: FDA approves nivolumab plus cabozantinib for advanced renal cell carcinoma. 2021. https://www.fda.gov/drugs/drug-approvals-and-databases/fda-approves-nivolumab-plus-cabozantinib-advanced-renal-cell-carcinoma. Accessed 14 Mar 2021.
US Food & Drug Administration: FDA approves lenvatinib plus pembrolizumab for advanced renal cell carcinoma. 2021. https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-lenvatinib-plus-pembrolizumab-advanced-renal-cell-carcinoma. Accessed 14 Aug 2021.
Choueiri TK, Powles T, Burotto M, Escudier B, Bourlon MT, Zurawski B, et al. Nivolumab plus cabozantinib versus sunitinib for advanced renal-cell carcinoma. N Engl J Med. 2021;384(9):829–41. https://doi.org/10.1056/NEJMoa2026982.
Choueiri TK: ESMO Virtual Congress: nivolumab + cabozantinib vs sunitinib in first-line treatment for advanced renal cell carcinoma: first results from the randomized phase 3 CheckMate 9ER trial. 2020. https://www.urotoday.com/conference-highlights/esmo-2020/kidney-cancer/124546-esmo-virtual-congress-2020-invited-discussant-first-results-from-the-randomized-phase-3-checkmate-9er-trial.html. Accessed 26 Jan 2021.
Huo S, Del Tejo V, Du EX, Wu A, Chen Y, Betts KA. Number needed to treat and cost per progression-free survivor of nivolumab plus cabozantinib vs. pembrolizumab plus axitinib for previously untreated advanced renal cell carcinoma. Academy of Managed Care Pharmacy (AMCP). Chicago, IL; 2022.
Martins F, Sofiya L, Sykiotis GP, Lamine F, Maillard M, Fraga M, et al. Adverse effects of immune-checkpoint inhibitors: epidemiology, management and surveillance. Nat Rev Clin Oncol. 2019;16(9):563–80. https://doi.org/10.1038/s41571-019-0218-0.
Li S, Li J, Peng L, Li Y, Wan X. Cost-effectiveness of nivolumab plus cabozantinib versus sunitinib as a first-line treatment for advanced renal cell carcinoma in the United States. Front Pharmacol. 2021. https://doi.org/10.3389/fphar.2021.736860.
Agency for Healthcare Research and Quality: HCUP Cost-to-Charge Ratio Files (CCR). (2006–2009). www.hcup-us.ahrq.gov/db/state/costtocharge.jsp. Accessed 5 Apr 2020.
Agency for Healthcare Research and Quality: HCUP National Inpatient Sample (NIS). 2012. www.hcup-us.ahrq.gov/nisoverview.jsp. Accessed 5 Apr 2020.
Agency for Healthcare Research and Quality: HCUPnet, Healthcare Cost and Utilization Project. 2020. https://hcupnet.ahrq.gov/. Accessed 5 Apr 2020.
US Medical Care Services: Consumer Price Index—All Urban Consumers. http://data.bls.gov/cgi-bin/surveymost?cu Accessed 5 Apr 2020.
National Cancer I. Common terminology criteria for adverse events (CTCAE). [Bethesda, Md.]: U.S. Dept. of Health and Human Services, National Institutes of Health, National Cancer Institute; 2010.
Brahmer JR, Lacchetti C, Schneider BJ, Atkins MB, Brassil KJ, Caterino JM, et al. Management of immune-related adverse events in patients treated with immune checkpoint inhibitor therapy: American Society of Clinical Oncology Clinical Practice Guideline. J Clin Oncol. 2018;36(17):1714–68. https://doi.org/10.1200/JCO.2017.77.6385.
Geynisman DM, Du EX, Yang X, Sendhil SR, Tejo VD, Betts KA, et al. Temporal trends of adverse events and costs of nivolumab plus ipilimumab versus sunitinib in advanced renal cell carcinoma. Future Oncol. 2022;18(10):1219–34. https://doi.org/10.2217/fon-2021-1109.
Hutson TE, Bellmunt J, Porta C, Szczylik C, Staehler M, Nadel A, et al. Long-term safety of sorafenib in advanced renal cell carcinoma: follow-up of patients from phase III TARGET. Eur J Cancer. 2010;46(13):2432–40. https://doi.org/10.1016/j.ejca.2010.06.121.
Porta C, Gore ME, Rini BI, Escudier B, Hariharan S, Charles LP, et al. Long-term safety of sunitinib in metastatic renal cell carcinoma. Eur Urol. 2016;69(2):345–51. https://doi.org/10.1016/j.eururo.2015.07.006.
Su Y, Fu J, Du J, Wu B. First-line treatments for advanced renal-cell carcinoma with immune checkpoint inhibitors: systematic review, network meta-analysis and cost-effectiveness analysis. Ther Adv Med Oncol. 2020;12:1758835920950199. https://doi.org/10.1177/1758835920950199.
Kadowaki H, Ishida J, Akazawa H, Yagi H, Saga-Kamo A, Umei M, et al. Axitinib induces and aggravates hypertension regardless of prior treatment with tyrosine kinase inhibitors. Circ Rep. 2021;3(4):234–40. https://doi.org/10.1253/circrep.CR-21-0008.
Schmidinger M, Danesi R. Management of adverse events associated with cabozantinib therapy in renal cell carcinoma. Oncologist. 2018;23(3):306–15. https://doi.org/10.1634/theoncologist.2017-0335.
Cabanillas ME, Takahashi S. Managing the adverse events associated with lenvatinib therapy in radioiodine-refractory differentiated thyroid cancer. Semin Oncol. 2019;46(1):57–64. https://doi.org/10.1053/j.seminoncol.2018.11.004.
Postow M. Toxicities associated with checkpoint inhibitor immunotherapy. 2021. https://www.uptodate.com/contents/toxicities-associated-with-checkpoint-inhibitor-immunotherapy. Accessed 2021.
Suzman DL, Pelosof L, Rosenberg A, Avigan MI. Hepatotoxicity of immune checkpoint inhibitors: an evolving picture of risk associated with a vital class of immunotherapy agents. Liver Int. 2018;38(6):976–87. https://doi.org/10.1111/liv.13746.
Abdel-Rahman O, ElHalawani H, Fouad M. Risk of elevated transaminases in cancer patients treated with immune checkpoint inhibitors: a meta-analysis. Expert Opin Drug Saf. 2015;14(10):1507–18. https://doi.org/10.1517/14740338.2015.1085969.
Acknowledgements
Analytical support was provided by Selvam R. Sendhil, BA, BS, and medical writing support was provided by Loraine Georgy, Ph.D., employees of Analysis Group, Inc.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Financial support for this research was provided by Bristol Myers Squibb. The study sponsor was involved in several aspects of the research, including the study design, the interpretation of data, the writing of the manuscript, and the decision to submit the manuscript for publication.
Conflict of interest
Stephen Huo and Viviana Del Tejo are employees of Bristol Myers Squibb, which funded the development and conduct of this study and manuscript. Ella X. Du, Xiaoran Yang, and Keith A. Betts are employees of Analysis Group, Inc., a consulting company that has provided paid consulting services to Bristol Myers Squibb. Daniel M. Geynisman received consulting fees from Pfizer, Exelixis, AstraZeneca, Seattle Genetics/Astellas, Eisai, Merck, Myovant Sciences, and 2nd.MD, as well as research funding from Genentech, Merck, Calithera Biosciences, Astellas Pharma, and Harpoon therapeutics. Mauricio Burotto received consulting fees from Roche/Genentech, Bristol Myers Squibb, MSD Oncology, Novartis, and AstraZeneca, as well as honoraria from Roche/Genentech, MSD Oncology, Bristol Myers Squibb, and AstraZeneca. Camillo Porta received consulting fees from Angelini Pharma, AstraZeneca, Bristol Myers Squibb, Eisai, EUSA Pharma, Ipsen, Merck Serono, and MSD, as well as honoraria from Bristol Myers Squibb, EUSA Pharma, General Electric, Ipsen, and MSD, payment for expert testimony from EUSA Pharma and Pfizer, and fees for attending meetings/travel from Roche. Cristina Suarez received research funding from AB Science, Aragon Pharmaceuticals, Astellas Pharma, AstraZeneca, Bayer, Blueprint Medicines, Boehringer Ingelheim España, Bristol Myers Squibb, Clovis Oncology, Exelixis, Genentech, GlaxoSmithKline, Hoffmann-La Roche, Novartis, Pfizer, and Sanofi-Aventis, as well as honoraria from Astellas Pharma, Bristol Myers Squibb, Hoffmann-La Roche, Ipsen, and Pfizer, and scientific advisory fees from Astellas Pharma, Bayer, Bristol Myers Squibb, EUSA Pharma, Hoffmann-La Roche, Ipsen, MSD, Novartis, Pfizer, and Sanofi-Aventis. Maria T. Bourlon received consulting fees from Bristol Myers Squibb, Asofarma, Eisai, MSD Oncology, Janssen Oncology, Novartis, Bayer, Ferring, as well as honoraria from Asofarma, MSD Oncology, Bristol Myers Squibb, Bayer, Eisai, Janssen Oncology, Ipsen, Pfizer, Merck, Ferring, Tecnofarma, Medicamenta, AstraZeneca, and Astellas Pharma, payment for expert testimony from Asofarma, support for attending meetings/travel from Asofarma, Janssen-Cilag, MSD Oncology, Bristol Myers Squibb Mexico, Pfizer, Ipsen, and Sanofi, and steering committee honoraria from Bristol Myers Squibb. Toni K. Choueiri participated in Data Safety Monitoring/Advisory Boards and received grants/contracts and consulting fees from AstraZeneca, Aravive, Aveo, Bayer, Bristol Myers Squibb, Calithera, Circle Pharma, Eisai, EMD Serono, Exelixis, GlaxoSmithKline, IQVIA, Infinity, Ipsen, Janssen, Kanaph, Lilly, Merck, Nikang, Nuscan, Novartis, Pfizer, Roche, Sanofi/Aventis, Surface Oncology, Takeda, Tempest, and UpToDate, and declares a leadership or fiduciary role in NCCN, GU Steering Committee, and ASCO/ESMO, owning stock or stock options in Pionyr, Tempest, Osel, and NuscanDx, institutional patents filed on molecular mutations and immunotherapy response, and ctDNA, medical writing and editorial assistance support which may have been funded in part by Communications companies, mentoring several non-US citizens on research projects with potential funding (in part) from non-US sources/Foreign Components, and receiving independent funding of drug companies or/and royalties potentially involved in research around the subject matter. Bradley McGregor received consulting fees from Exelixis, Bristol Myers Squibb, Pfizer, Seattle Genetics, Calithera, EMD Serono, Eisai, Asetellas, Dendreon, Nektar, and Bayer, as well as research funding from Exelixis, Bristol Myers Squibb, Pfizer, Seattle Genetics, and Calithera.
Ethics approval
CheckMate 9ER was approved by the institutional review board or ethics committee at each site and conducted in accordance with Good Clinical Practice guidelines per the International Conference on Harmonisation. All patients provided written informed consent based on Declaration of Helsinki principles.
Consent to participate
Not applicable. This a post-hoc analysis of previously collected, de-identified data.
Consent for publication
Not applicable.
Code availability
Code is not available for sharing.
Data availability statement
Data are available upon reasonable request. Bristol Myers Squibb’s policy on data sharing may be found at https://www.bms.com/researchers-and-partners/independent-research/data-sharingrequest-process.html. De-identified and anonymized datasets of clinical trial information, including patient-level data, will be shared with external researchers for proposals that are complete, for which the scientific request is valid and the data are available, consistent with safeguarding patient privacy and informed consent.
Authors’ contributions
All authors were involved in the conception and design, and/or analysis and interpretation of the data; the drafting of the paper and revising it critically for intellectual content; and the final approval of the version to be published. All authors agree to be accountable for all aspects of the work.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Geynisman, D.M., Burotto, M., Porta, C. et al. Temporal Trends in Grade 3/4 Adverse Events and Associated Costs of Nivolumab Plus Cabozantinib Versus Sunitinib for Previously Untreated Advanced Renal Cell Carcinoma. Clin Drug Investig 42, 611–622 (2022). https://doi.org/10.1007/s40261-022-01170-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40261-022-01170-6