Abstract
Introduction
Few studies describe the adverse drug event profiles in patients simultaneously receiving antiretroviral and anti-tubercular medicines in resource-limited countries.
Objectives
To describe and compare the adverse drug reaction profiles in patients on highly active antiretroviral therapy only (HAART), HAART and isoniazid preventive therapy (HHART), and HAART and antitubercular treatment (ATTHAART).
Methods
We analysed individual case safety reports (ICSRs) for patients on antiretroviral therapy and antitubercular treatment submitted to the national pharmacovigilance centre during the targeted spontaneous reporting (TSR) programme from 1 September 2012 through 31 August 2016. All reports considered certain, probable or possible were included in the analysis.
Results
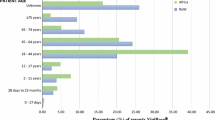
A total of 1076 ICSRs were included in the analysis. Most of the reports were from the HAART only group (n = 882; 82.0%), followed by patients on HHART (n = 132; 12.3%), and ATTHAART (n = 62; 5.7%). The ATTHAART (35.5%) and HHAART (34.1%) had a higher frequency of hepatic disorders than the HAART group (5.0%) (p < 0.0001). A higher frequency of rash was reported in the HHAART (35.6%) and HAART groups (29.4%) than the ATTHAART group (14.5%) (p = 0.011). Peripheral neuropathy occurred more frequently in the ATTHAART group (19.3%) than other groups (p = 0.001) while Stevens-Johnson syndrome (14.7%; p < 0.001), gynaecomastia (18.2%; p < 0.001), and lipodystrophy (4.5%; p = 0.012) occurred more frequently in the HAART group. The HHAART group was associated with a higher frequency of psychosis (4.5%; p = 0.002).
Conclusion
Antiretroviral therapy was associated with a higher frequency of Stevens-Johnson syndrome, gynaecomastia, and lipodystrophy. Co-administration of antiretroviral and antitubercular medicines was associated with a higher frequency of drug-induced liver injury and peripheral neuropathy. Similarly, co-administration of isoniazid preventive therapy and antiretroviral drugs was associated with a higher risk for psychosis. There is a need to carefully manage TB/HIV co-infected patients, due to the higher risk of adverse drug reactions which may lead to poor treatment adherence and outcomes.

Similar content being viewed by others
References
Raviglione M, Sulis G. Tuberculosis 2015: burden, challenges and strategy for control and elimination. Infect Dis Rep. 2016;8:33–7.
WHO. WHO| TB/HIV facts 2012–2013. WHO. World Health Organization; 2015. http://www.who.int/hiv/topics/tb/tbhiv_facts_2013/en/. Accessed 2 Oct 2016.
USAID. HIV and AIDS| U.S. Agency for International Development. http://www.usaid.gov/what-we-do/global-health/hiv-and-aids. Accessed 29 Sept 2016.
Martinson NA, Hoffmann CJ, Chaisson RE. Epidemiology of tuberculosis and HIV: recent advances in understanding and responses. Proc Am Thorac Soc. 2011;8:288–93.
Getahun H, Gunneberg C, Granich R, Nunn P. HIV infection-associated tuberculosis: the epidemiology and the response. Clin Infect Dis. 2010;50(Suppl 3):S201–7.
Kwan C, Ernst JD. HIV and tuberculosis: A deadly human syndemic. Clin Microbiol Rev. 2011;24:351–76.
Girardi E, Antonucci G, Vanacore P, Libanore M, Errante I, Matteelli A, et al. Impact of combination antiretroviral therapy on the risk of tuberculosis among persons with HIV infection. AIDS. 2000;14:1985–91.
Badri M, Wilson D, Wood R. Effect of highly active antiretroviral therapy on incidence of tuberculosis in South Africa: a cohort study. The Lancet. 2002;359:2059–64.
Manosuthi W, Chottanapand S, Thongyen S, Chaovavanich A, Sungkanuparph S. Survival rate and risk factors of mortality among HIV/tuberculosis-coinfected patients with and without antiretroviral therapy. JAIDS J Acquir Immune Defic Syndr. 2006;43:42–6.
McIlleron H, Meintjes G, Burman WJ, Maartens G. Complications of antiretroviral therapy in patients with tuberculosis: drug interactions, toxicity, and immune reconstitution inflammatory syndrome. J Infect Dis [Internet]. 2007;196:S63–75.
Marks DJB, Dheda K, Dawson R, Ainslie G, Miller RF. Adverse events to antituberculosis therapy: influence of HIV and antiretroviral drugs. Int J STD AIDS. 2009;20:339–45.
Subbaraman R, Chaguturu SK, Mayer KH, Flanigan TP, Kumarasamy N. Adverse effects of highly active antiretroviral therapy in developing countries. Clin Infect Dis. 2007;45:1093–101.
Manosuthi W, Wiboonchutikul S, Sungkanuparph S. Integrated therapy for HIV and tuberculosis. AIDS Res Ther. 2016;13:22.
Kadima JN, Mukanyangezi MF, Uwizeye CB. Effectiveness and safety of concurrent use of first-line antiretroviral and antituberculous drugs in Rwanda. J Trop Med. 2014;2014:e904957.
World Health Organization. Guidelines for intensified tuberculosis case-finding and isoniazid preventive therapy for people living with HIV in resource-constrained settings. World Health. 2011;1:142. http://whqlibdoc.who.int/publications/2011/9789241500708_eng.pdf. Accessed 1 Oct 2016.
Denholm JT, McBryde ES, Eisen DP, Penington JS, Chen C, Street AC. Adverse effects of isoniazid preventative therapy for latent tuberculosis infection: a prospective cohort study. Drug Healthc Patient Saf. 2014;6:145–9.
Tedla Z, Nyirenda S, Peeler C, Agizew T, Sibanda T, Motsamai O, et al. Isoniazid-associated hepatitis and antiretroviral drugs during tuberculosis prophylaxis in HIV-infected adults in Botswana. Am J Respir Crit Care Med. 2010;182:278–85.
Decloedt EH, Mwansa-Kambafwile J, Van Der Walt JS, McIlleron H, Denti P, Smith P, et al. The pharmacokinetics of nevirapine when given with isoniazid in South African HIV-infected individuals. Int J Tuberc Lung Dis. 2013;17:333–5.
Sadiq S, Khajuria V, Tandon VR, Mahajan A, Singh JB. Adverse drug reaction profile in patients on anti-tubercular treatment alone and in combination with highly active antiretroviral therapy. J Clin Diagnostic Res. 2015;9:FC01–4.
Ampadu HH, Hoekman J, de Bruin ML, Pal SN, Olsson S, Sartori D, et al. Adverse drug reaction reporting in Africa and a comparison of individual case safety report characteristics between Africa and the rest of the world: analyses of spontaneous reports in VigiBase®. Drug Saf. 2016;39:335–45.
Muula AS, Ngulube TJ, Siziya S, Makupe CM, Umar E, Prozesky HW et al. Gender distribution of adult patients on highly active antiretroviral therapy (HAART) in Southern Africa: a systematic review. BMC Public Health. 2007;7:63. http://bmcpublichealth.biomedcentral.com/articles/10.1186/1471-2458-7-63. Accessed 6 June 2017.
Marques J, Ribeiro-Vaz I, Pereira AC, Polõnia J. A survey of spontaneous reporting of adverse drug reactions in 10 years of activity in a pharmacovigilance centre in Portugal. Int J Pharm Pract. 2014;22:275–82.
Ozcan G, Aykac E, Kasap Y, Nemutlu NT, Sen E, Aydinkarahaliloglu ND. Adverse drug reaction reporting pattern in Turkey: analysis of the national database in the context of the first pharmacovigilance legislation. Drug Real World Outcome. 2016;3:33–43.
Acknowledgements
We gratefully acknowledge the Global Fund, WHO, WHO-Uppsala Monitoring Centre (UMC), UNICEF and MCAZ for providing financial support to strengthen pharmacovigilance for HIV and TB medicines in Zimbabwe and technical support for the VigiBase database. We also acknowledge the following: the Ministry of Health and Child Care ART and TB programmes, Directorate of Pharmacy Services, central hospitals, the district and/or provincial healthcare teams, and the Newlands Clinic, for their participation during the TSR programme and for collection of ADR reports. We also thank WHO, Mr Sten Olsson, Dr Shantil Pal for their contribution in the design and implementation of the TSR programme. We are also grateful to Dr Luther Gwaza and the Director General for MCAZ Gugulethu N Mahlangu, for their contribution in the design of the Targeted Spontaneous Reporting programme and their comments on the draft manuscript. We also acknowledge the contribution made by the Pharmacovigilance and Clinical Trials Committee during causality assessment of all reported ADRs.
Author information
Authors and Affiliations
Contributions
JTM was involved in the study design, collection and analysis of the data, and drafted the manuscript. PC was involved in the study design, collection and analysis of the data. PPN and SK were involved in the study design, analysis of the data, revised and critically reviewed the manuscript. AS critically reviewed and edited the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All the authors declare no conflict of interest.
Funding
The targeted spontaneous reporting programme was funded through the Global Fund, Grant GF-OIG-13-012. Funding was also provided by WHO, UNICEF and MCAZ. The ADR reports used in this study were submitted during the targeted spontaneous reporting programme. However, no direct funding from the Global Fund grant and other donor partners was received in the conduct of this study and during preparation of the manuscript.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study formal consent is not required.
Rights and permissions
About this article
Cite this article
Masuka, J.T., Chipangura, P., Nyambayo, P.P. et al. A Comparison of Adverse Drug Reaction Profiles in Patients on Antiretroviral and Antitubercular Treatment in Zimbabwe. Clin Drug Investig 38, 9–17 (2018). https://doi.org/10.1007/s40261-017-0579-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40261-017-0579-z