Summary
Purpose
Disturbances of sleep have frequently been reported in individuals with migraine. On top of this, an elderly patient with migraine also suffers from sleep disturbances due to changes in physiologic and mental health associated with aging. This study aimed to compare several sleep factors, namely sleep quality, chronotype, and obstructive sleep apnea (OSA) risk, between elderly people with and without migraine.
Methods
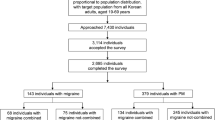
This was a multicenter cross-sectional study conducted in 10 neurologic clinics located in Tehran, Iran, over 2 years. The sample size was calculated as 189, including 63 migraine and 126 non-migraine patients.
Results
A significant difference was observed in the mean score of the global Pittsburgh Sleep Quality Index (PSQI) between migraine and non-migraine groups (p-value = 0.002), and in the individual components of the PSQI. However, there were no significant differences in the frequency of different types of chronotype (p-value = 0.125, T = 1.541) or OSA risk between the two groups (p-value = 0.568, T = −0.573). The binary logistic regression model showed that the relationship between global PSQI and migraine was significant (p = 0.002).
Conclusion
Sleep quality is a problem for elderly migraine sufferers. Meanwhile, certain factors such as chronotype and OSA have no significant relationship with migraine among community-dwelling seniors. Further studies are required to enhance our understanding of this observation.
Zusammenfassung
Ziel der Arbeit
Schlafstörungen werden häufig von Personen mit Migräne angegeben. Außerdem leidet ein älterer Patient mit Migräne auch an Schlafstörungen aufgrund von altersbedingten Veränderungen der physiologischen Abläufe und der psychischen Gesundheit. Ziel der vorliegenden Studie war es, verschiedene Schlaffaktoren, insbesondere die Schlafqualität, den Chronotyp und das Risiko für obstruktive Schlafapnoe (OSA), zwischen älteren Menschen mit und ohne Migräne zu vergleichen.
Methoden
Es handelt sich um eine Multizenter-Querschnitt-Studie, die 2 Jahre lang an 10 neurologischen Kliniken in Teheran, Iran, durchgeführt wurde. Als Stichprobengröße wurden 189 Probanden ermittelt, 63 Patienten mit Migräne und 126 ohne Migräne.
Ergebnisse
Ein signifikanter Unterschied zwischen der Gruppe mit und der Gruppe ohne Migräne wurde beim mittleren Wert für den globalen Pittsburgh Sleep Quality Index (PSQI) festgestellt (p = 0,002) sowie für die einzelnen Komponenten des PSQI. Jedoch bestanden keine signifikanten Unterschiede zwischen den beiden Gruppen bei der Häufigkeit der verschiedenen Typen des Chronotyps (p = 0,125; T = 1,541) oder beim OSA-Risiko (p = 0,568; T = −0,573). Das binäre logistische Regressionsmodell zeigte, dass der Zusammenhang zwischen dem globalen PSQI und Migräne signifikant war (p = 0,002).
Schlussfolgerung
Die Schlafqualität stellt ein Problem für ältere Migränepatienten dar. Allerdings weisen bestimmte Faktoren wie der Chronotyp und OSA keinen signifikanten Zusammenhang mit Migräne bei Senioren auf, die noch selbstständig in der Gesellschaft leben. Weitere Studien sind erforderlich, um das Verständnis dieser Beobachtung zu vertiefen.
Similar content being viewed by others
Abbreviations
- ICHD3:
-
International Classification of Headache Disorders third edition
- MEQ:
-
Morningness–Eveningness Questionnaire
- OSA:
-
Obstructive sleep apnea
- PSQI:
-
Pittsburgh Sleep Quality Index
- STOP-BANG:
-
Snoring, tiredness, observed apnea, blood pressure, body mass index, age, neck circumference, gender questionnaire
References
Steiner TJ, Stovner LJ, Birbeck GL. Migraine: the seventh disabler. Headache. 2013;53(2):227–9.
Olesen J, Bes A, Kunkel R, Lance JW, Nappi G, Pfaffenrath V, et al. The international classification of headache disorders, 3rd edition (beta version). Cephalalgia. 2013;33(9):629–808.
Woldeamanuel YW, Cowan RP. Migraine affects 1 in 10 people worldwide featuring recent rise: a systematic review and meta-analysis of community-based studies involving 6 million participants. J Neurol Sci. 2017;372:307–15.
Farhadi Z, Alidoost S, Behzadifar M, Mohammadibakhsh R, Khodadadi N, Sepehrian R, et al. The prevalence of migraine in Iran: a systematic review and meta-analysis. Iran Red Crescent Med J. 2016;18(10):e40061.
Kaniecki RG, Levin AD. Headache in the elderly. 1st ed. Handbook of clinical neurology, Vol. 167. Elsevier; 2019. pp. 511–28.
Andrés-Jensen L, Larsen HB, Johansen C, Frandsen TL, Schmiegelow K, Wahlberg A. Everyday life challenges among adolescent and young adult survivors of childhood acute lymphoblastic leukemia: an in-depth qualitative study. Psychooncology. 2020;29(10):1630–7.
Bathory E, Tomopoulos S. Sleep regulation, physiology and development, sleep duration and patterns, and sleep hygiene in infants, toddlers, and preschool-age children. Curr Probl Pediatr Adolesc Health Care. 2017;47(2):29–42.
Myllyntausta S, Salo P, Kronholm E, Pentti J, Kivimäki M, Vahtera J, et al. Changes in sleep difficulties during the transition to statutory retirement. Sleep. 2018;41(1):1–14. https://doi.org/10.1093/sleep/zsx182.
Vgontzas A, Pavlović JM. Sleep disorders and migraine: review of literature and potential pathophysiology mechanisms. Headache. 2018;58(7):1030–9.
Buse DC, Greisman JD, Baigi K, Lipton RB. Migraine progression: a systematic review. Headache. 2019;59(3):306–38.
Jalilian R, Ghajarzadeh M, Fateh R, Togha M, Sahraian MA, Azimi A. Comparison of sleep quality in women with migraine moreover, multiple sclerosis. Acta Med Iran. 2014;52(9):690–3.
Kim SJ, Han KT, Jang SY, Yoo KB, Kim SJ. The association between migraine and types of sleep disorder. Int J Environ Res Public Health. 2018;15(12):2648.
Schramm S, Tenhagen I, Schmidt B, Holle-Lee D, Naegel S, Katsarava Z, et al. Prevalence and risk factors of migraine and non-migraine headache in older people—results of the Heinz Nixdorf recall study. Cephalalgia. 2021;41:649–64.
Ferini-Strambi L, Galbiati A, Combi R. Sleep disorder-related headaches. Neurol Sci. 2019;40:107–13.
Burish MJ, Chen Z, Yoo SH. Emerging relevance of circadian rhythms in headaches and neuropathic pain. Acta Physiol. 2019;225:0–2.
Gariépy G, Doré I, Whitehead RD, Elgar FJ. More than just sleeping in: a late timing of sleep is associated with health problems and unhealthy behaviours in adolescents. Sleep Med. 2019;56:66–72.
van Oosterhout WPJ, van Someren EJW, Schoonman GG, Louter MA, Lammers GJ, Ferrari MD, et al. Chronotypes and circadian timing in migraine. Cephalalgia. 2018;38:617–25.
Viticchi G, Falsetti L, Paolucci M, Altamura C, Buratti L, Salvemini S, et al. Influence of chronotype on migraine characteristics. Neurol Sci. 2019;40:1841–8. https://doi.org/10.1007/s10072-019-03886-4.
Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol. 2013;177:1006–14.
Senaratna CV, Perret JL, Lodge CJ, Lowe AJ, Campbell BE, Matheson MC, et al. Prevalence of obstructive sleep apnea in the general population: a systematic review. Sleep Med Rev. 2017;34:70–81.
Yin J, Chen S, Lin C, Sung Y, Chou C, Chung C, et al. Increased risk of sleep apnoea among primary headache disorders : a nationwide population-based longitudinal study. 2019. pp. 1–6.
Kristiansen HA, Kværner KJ, Akre H, Øverland B, Russell MB. Migraine and sleep apnea in the general population. J Headache Pain. 2011;12:55–61.
Yin JH, Chen SY, Lin CC, Sung YF, Chou CH, Chung CH, et al. Increased risk of sleep apnoea among primary headache disorders: a nationwide population-based longitudinal study. Postgrad Med J. 2019;95:72–7.
Headache Classification Committee of the International Headache Society (IHS). The international classification of headache disorders, (beta version). Cephalalgia. 2013;33(9):629–808.
Buysse DJ, Reynolds CF III, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213.
Farrahi Moghaddam J, Nakhaee N, Sheibani V, Garrusi B, Amirkafi A. Reliability and validity of the Persian version of the Pittsburgh sleep quality index (PSQI-P). Sleep Breath. 2012;16:79–82.
Park BK. The Pittsburg sleep quality index (PSQI) and associated factors in middle-school students: a cross-sectional study. Child Health Nurs Res. 2020;26(1):55.
Horne JA, Ostberg O. A self assessment questionnaire to determine moningness eveningness in human circadian rhythms. Int J Chronobiol. 1976;4:97–110.
Chung F, Yegneswaran B, Liao P, Chung SA, Vairavanathan S, Islam S, Khajehdehi A, Shapiro CM. STOP questionnaire: a tool to screen patients for obstructive sleep apnea. Anesthesiology. 2008;108(5):812–21.
Sadeghniiat-Haghighi K, Montazeri A, Khajeh-Mehrizi A, Ghajarzadeh M, Alemohammad ZB, Aminian O, Sedaghat M. The STOP-BANG questionnaire: reliability and validity of the Persian version in sleep clinic population. Qual Life Res. 2015;24:2025–30.
Stanyer EC, Creeney H, Nesbitt AD, Holland PR, Hoffmann J. Subjective sleep quality and sleep architecture in patients with migraine: a meta-analysis. Neurology. 2021;97(16):e1620–31.
Song TJ, Yun CH, Cho SJ, Kim WJ, Yang KI, Chu MK. Short sleep duration and poor sleep quality among migraineurs: a population-based study. Cephalalgia. 2018;38(5):855–64.
Lin YK, Lin GY, Lee JT, Lee MS, Tsai CK, Hsu YW, et al. Associations between sleep quality and migraine frequency. Medicine. 2016;95:1–7.
Lampl C, Thomas H, Stovner LJ, Tassorelli C, Katsarava Z, Laínez JM, et al. Interictal burden attributable to episodic headache: findings from the Eurolight project. J Headache Pain. 2016;17:1–10.
Stanyer EC, Creeney H, Nesbitt AD, Holland PR, Hoffmann J. Subjective sleep quality and sleep architecture in patients with migraine: a meta-analysis. Neurology. 2021;97:E1620–E31.
Wang Y, Xie J, Yang F, Wu S, Wang H, Zhang X, et al. Comorbidity of poor sleep and primary headaches among nursing staff in north China. J Headache Pain. 2015;16:88.
Sadeghniiat K, Rajabzadeh A, Ghajarzadeh M, Ghafarpour M. Sleep quality and depression among patients with migraine. Acta Med Iran. 2013;51:784–8.
Song TJ, Cho SJ, Kim WJ, Yang KI, Yun CH, Chu MK. Poor sleep quality in migraine and probable migraine: a population study. J Headache Pain. 2018;19(1):58. https://doi.org/10.1186/s10194-018-0887-6.
Parashar R, Bhalla P, Rai NK, Pakhare A, Babbar R. Migraine: is it related to hormonal disturbances or stress? Int J Womens Health. 2014;6:921–5.
Putra EK, Machfoed MH. Correlation of sleep quality and anxiety with pain intensity in primary headache patients. Medico-Legal Update. 2020;20:843–7.
Cevoli S, Nicodemo M, Grimaldi D, Leonardi L, Montagna P, Cortelli P, Pierangeli G. Chronotypes in menstrual migraine: a case–control study. Neurol Sci. 2010;31:163–4.
Rafique N, Al-Asoom LI, Latif R, Alsunni AA, Salem AM, Alkhalifa ZH, et al. Prevalence of migraine and its relationship with psychological stress and sleep quality in female university students in Saudi Arabia. J Pain Res. 2020;13:2423–30.
Fox AW, Davis RL. Migraine chronobiology. Headache. 1998;38:436–41.
Sullivan DP, Martin PR. Sleep and headaches: relationships between migraine and non-migraine headaches and sleep duration, sleep quality, chronotype, and obstructive sleep apnoea risk. Aust J Psychol. 2017;69(3):210–7.
Gori S, Morelli N, Maestri M, Fabbrini M, Bonanni E, Murri L. Sleep quality, chronotypes and preferential timing of attacks in migraine without aura. J Headache Pain. 2005;6:258–60.
Im H‑J, et al. Time preference of headache attack and chronotype in migraine and tension-type headache. Chronobiol Int. 2019;36:1528–36.
Harnod T, Wang YC, Kao CH. Association of migraine and sleep-related breathing disorder: a population-based cohort study. Medicine. 2015;94:1–6.
Buse DC, Rains JC, Pavlovic JM, Fanning KM, Reed ML, Manack Adams A, Lipton RB. Sleep disorders among people with migraine: results from the chronic migraine epidemiology and outcomes (CaMEO) study. Headache. 2019;59(1):32–45.
Grazzi L, Toppo C, D’amico D, Leonardi M, Martelletti P, Raggi A, et al. Non-pharmacological approaches to headaches: non-invasive neuromodulation, nutraceuticals, and behavioral approaches. Int J Environ Res Public Health. 2021;18:1–17.
Acknowledgements
We would like to thank Ms. Nur Athirah Inche Mat for the English revision of the manuscript.
Funding
This work is supported by Putra Grant (GP-IPM/2017/9544800) from University Putra Malaysia, Malaysia.
Author information
Authors and Affiliations
Contributions
AKF, MR, and HMD analyzed and interpreted the patient data. WAWS, HB, MHM, VR, and LNIM drafted the study protocol and were major contributors in writing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
A. Kouhi Fayegh, H. Mat Din, W.A. Wan Sulaiman, M. Ravanipour, H. Basri, M.H. Bin Mohamed, V. Ramachandran, and L.N. Inche Mat declare that they have no competing interests.
Ethical standards
This study was performed in accordance with the Declaration of Helsinki. It has been approved by the Ethics Committee of University Putra Malaysia (JKEUPM), reference number JKEUPM-2019-314, and Bushehr province University of Medical Sciences Research Ethics Committee, reference number IR.BPUMS.REC.1398.125. Informed consent to participate in this study was obtained from all subjects and/or their guardian(s).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Availability of data and material
The datasets generated and/or analyzed during the study are not publicly available to protect patient privacy but are available from the corresponding author upon reasonable request.
Rights and permissions
About this article
Cite this article
Kouhi Fayegh, A., Mat Din, H., Wan Sulaiman, W.A. et al. Relationship of sleep quality, chronotype, and obstructive sleep apnea with migraine in the elderly population. Neuropsychiatr (2023). https://doi.org/10.1007/s40211-023-00467-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40211-023-00467-y