Abstract
Purpose of Review
We aimed to describe bleeding events associated with extracorporeal cardiopulmonary resuscitation (eCPR) using two institutional heparin protocols. In addition, we discuss current barriers to optimal anticoagulation in this critical population.
Recent Findings
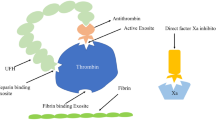
Patients initiated on venoarterial membrane oxygenation (VA-ECMO) are at risk of bleeding and thrombosis; both conditions can lead to severe morbidity or mortality. Intravenous heparin is the preferred form of anticoagulation for VA-ECMO. Prior studies have found elevated activated partial thromboplastin time (aPTT) may be an independent risk factor for bleeding; however, many studies lack standardization of bleeding scores and optimal anticoagulation targets.
Summary
All six patients initiated on VA-ECMO experienced at least one bleeding event. Of 71 aPTT levels collected, 44% were within therapeutic range, 18% were subtherapeutic, and 38% were supratherapeutic. There were no obvious correlation between aPTT levels and bleeding. Future studies are needed to evaluate anticoagulation strategies in this population.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Dalle Ave AL, Shaw DM, Gardiner D. Extracorporeal membrane oxygenation (ECMO) assisted cardiopulmonary resuscitation or uncontrolled donation after the circulatory determination of death following out-of-hospital refractory cardiac arrest-an ethical analysis of an unresolved clinical dilemma. Resuscitation. 2016;108:87–94.
Lee JJ, Han SJ, Kim HS, Hong KS, Choi HH, Park KT, et al. Out-of-hospital cardiac arrest patients treated with cardiopulmonary resuscitation using extracorporeal membrane oxygenation: focus on survival rate and neurologic outcome. Scand J Trauma Resusc Emerg Med. 2016;24:74.
Choi DH, Kim YJ, Ryoo SM, Sohn CH, Ahn S, Seo DW, et al. Extracorporeal cardiopulmonary resuscitation among patients with out-of-hospital cardiac arrest. Clin Exp Emerg Med. 2016;3(3):132–8.
• Tonna JE, Johnson NJ, Greenwood J, Gaieski DF, Shinar Z, Bellezo JM, et al. Practice characteristics of emergency department extracorporeal cardiopulmonary resuscitation (eCPR) programs in the United States: the current state of the art of emergency department extracorporeal membrane oxygenation (ED ECMO). Resuscitation. 2016;107:38–46. This article is important because it describes the culture and lack of inclusion and exclusion for patients who received VA-ECMO in an emergency department.
Hunziker S, Semmer NK, Tschan F, Schuetz P, Mueller B, Marsch S. Dynamics and association of different acute stress markers with performance during a simulated resuscitation. Resuscitation. 2012;83(5):572–8.
Shin TG, Jo IJ, Sim MS, Song YB, Yang JH, Hahn JY, et al. Two-year survival and neurological outcome of in-hospital cardiac arrest patients rescued by extracorporeal cardiopulmonary resuscitation. Int J Cardiol. 2013;168(4):3424–30.
• Iwashita Y, Yukimitsu M, Matsuduki M, Yamamoto A, Ishikura K, Imai H. Use of a fixed, body weight-unadjusted loading dose of unfractionated heparin for extracorporeal cardiopulmonary resuscitation. J Intensive Care. 2015;3(1):33. This article is important because it describes fixed heparin bolus doses used in ECMO and resulted in fatal bleeding events.
Murphy DA, Hockings LE, Andrews RK, Aubron C, Gardiner EE, Pellegrino VA, et al. Extracorporeal membrane oxygenation-hemostatic complications. Transfus Med Rev. 2015;29(2):90–101.
• Oliver WC. Anticoagulation and coagulation management for ECMO. Semin Cardiothorac Vasc Anesth. 2009;13(3):154–75. This article is important because it provides a review of methods used to monitor anticoagulation in patients with ECMO.
Factora FN, et al. Intracranial hemorrhage surgery on patients on mechanical circulatory support: a case series. J Neurosurg Anesthesiol. 2011;23(1):30–4.
•• Sy E, Sklar MC, Lequier L, Fan E, Kanji HD. Anticoagulation practices and the prevalence of major bleeding, thromboembolic events, and mortality in venoarterial extracorporeal membrane oxygenation: a systematic review and meta-analysis. J Crit Care. 2017;39:87–96. This systematic review is important because it demonstrated optimal targets and strategies for anticoagulation monitoring in VA-ECMO are unclear.
Mehran R, Rao SV, Bhatt DL, Gibson CM, Caixeta A, Eikelboom J, et al. Standardized bleeding definitions for cardiovascular clinical trials: a consensus report from the Bleeding Academic Research Consortium. Circulation. 2011;123(23):2736–47.
•• Vranckx P, White HD, Huang Z, Mahaffey KW, Armstrong PW, van de Werf F, et al. Validation of BARC bleeding criteria in patients with acute coronary syndromes: the TRACER trial. J Am Coll Cardiol. 2016;67(18):2135–44. This article is significant because it validates the use of BARC bleeding scales for ACS related trials due to its association with death after a cardiac event with higher BARC scores.
Lim JY, Kim JB, Choo SJ, Chung CH, Lee JW, Jung SH. Anticoagulation during extracorporeal membrane oxygenation; nafamostat mesilate versus heparin. Ann Thorac Surg. 2016;102(2):534–9.
• Lamarche Y, Chow B, Bédard A, Johal N, Kaan A, Humphries KH, et al. Thromboembolic events in patients on extracorporeal membrane oxygenation without anticoagulation. Innovations (Phila). 2010;5(6):424–9. This article is significant because the researchers used no anticoagulation in VA-ECMO without increased thromboembolic events.
Da Q, et al. Free hemoglobin increases von Willebrand factor-mediated platelet adhesion in vitro: implications for circulatory devices. Blood. 2015;126(20):2338–41.
Otani T, Sawano H, Natsukawa T, Matsuoka R, Nakashima T, Takahagi M, et al. D-dimer predicts bleeding complication in out-of-hospital cardiac arrest resuscitated with ECMO. Am J Emerg Med. 2018;36(6):1003–8.
Prakash S, et al. Discordance between ROTEM(R) clotting time and conventional tests during unfractionated heparin-based anticoagulation in intensive care patients on extracorporeal membrane oxygenation. Anaesth Intensive Care. 2016;44(1):85–92.
Park HSKaS. Blood transfusion strategies in patients undergoing extracorporeal membrane oxygenation. Koran J Crit Care Med. 2017;21(1):22–8.
Malfertheiner MV, et al. Acquired von Willebrand syndrome in respiratory extracorporeal life support: a systematic review of the literature. Critical Care And Resuscitation: Journal Of The Australasian Academy Of Crit Care Resusc. 2017;19(Suppl 1):45–52.
Omar HR, et al. Plasma free hemoglobin is an independent predictor of mortality among patients on extracorporeal membrane oxygenation support. PLoS One. 2015;10(4):e0124034.
Tekindur S, Yetim M, Kilickaya O. Risk of transfusion-related acute lung injury after blood products transfusions. Am J Emerg Med. 2016;34(8):1674–5.
Zalpuri S, et al. Intensive red blood cell transfusions and risk of alloimmunization. Transfusion. 2014;54(2):278–84.
•• Aubron C, DePuydt J, Belon F, Bailey M, Schmidt M, Sheldrake J, et al. Predictive factors of bleeding events in adults undergoing extracorporeal membrane oxygenation. Ann Intensive Care. 2016;6(1):97. This article is important because it concluded elevated aPTT levels were associated with more bleeding events.
Aubron C, Cheng AC, Pilcher D, Leong T, Magrin G, Cooper DJ, et al. Factors associated with outcomes of patients on extracorporeal membrane oxygenation support: a 5-year cohort study. Crit Care. 2013;17(2):R73.
Bakhtiary F, Keller H, Dogan S, Dzemali O, Oezaslan F, Meininger D, et al. Venoarterial extracorporeal membrane oxygenation for treatment of cardiogenic shock: clinical experiences in 45 adult patients. J Thorac Cardiovasc Surg. 2008;135(2):382–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Pharmacology Care
Rights and permissions
About this article
Cite this article
Terry, K., Lonardo, N. & Tonna, J. Anticoagulation Levels and Bleeding After Emergency Department Extracorporeal Cardiopulmonary Resuscitation. Curr Emerg Hosp Med Rep 7, 1–5 (2019). https://doi.org/10.1007/s40138-019-00176-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40138-019-00176-3