Abstract
Purpose of Review
(1) To discuss the relevance of the 2018 International Society of Nephrology/Renal Pathology Society (ISN/RPS) classification system for nephritis in childhood-onset systemic lupus erythematosus (SLE). (2) To highlight current practices not addressed in the 2013 Childhood Arthritis and Rheumatology Research Alliance (CARRA) consensus treatment plan (CTP) for pediatric lupus nephritis (LN).
Recent Findings
In addition to class of glomerular involvement, multiple features on kidney biopsy can be assessed for prognosis and therapeutic decision-making. There is pediatric evidence and expertise for optimization of LN classification. Yet, treatment is based primarily on whether nephritis is proliferative or membranous. Moreover, alternative strategies for induction therapy are more commonly prescribed for children.
Summary
There is a need for pediatric data to evaluate/validate LN classification systems. Updates are needed to CTPs for LN induction therapy. Pediatric nephrologists should be enrolling LN patients into existing prospective registries to build the evidence base for treatment decisions.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Sule S, Fivush B, Neu A, Furth S. Increased risk of death in pediatric and adult patients with ESRD secondary to lupus. Pediatr Nephrol (Berlin, Germany). 2011;26(1):93–8. https://doi.org/10.1007/s00467-010-1640-9.
Mina R, Brunner HI. Update on differences between childhood-onset and adult-onset systemic lupus erythematosus. Arthritis research & therapy. 2013;15(4):218. https://doi.org/10.1186/ar4256.
Son MBF, Johnson VM, Hersh AO, Lo MS, Costenbader KH. Outcomes in hospitalized pediatric patients with systemic lupus erythematosus. Pediatrics. 2014;133(1):e106–e13. https://doi.org/10.1542/peds.2013-1640.
Goilav B, Putterman C, Rubinstein TB. Biomarkers for kidney involvement in pediatric lupus. Biomark Med. 2015;9(6):529–43. https://doi.org/10.2217/bmm.15.25.
Wenderfer SE, Ruth NM, Brunner HI. Advances in the care of children with lupus nephritis. Pediatr Res. 2017;81(3):406–14. https://doi.org/10.1038/pr.2016.247.
Mina R, von Scheven E, Ardoin SP, Eberhard BA, Punaro M, Ilowite N, et al. Consensus treatment plans for induction therapy of newly diagnosed proliferative lupus nephritis in juvenile systemic lupus erythematosus. Arthritis Care Res. 2012;64(3):375–83. https://doi.org/10.1002/acr.21558.
Wenderfer SE, Lane JC, Shatat IF, von Scheven E, Ruth NM. Practice patterns and approach to kidney biopsy in lupus: a collaboration of the Midwest Pediatric Nephrology Consortium and the Childhood Arthritis and Rheumatology Research Alliance. Pediatr Rheumatol. 2015;13:26. https://doi.org/10.1186/s12969-015-0024-x.
Boneparth A, Radhakrishna SM, Greenbaum LA, Yen E, Okamura DM, Cooper JC, et al. Approach to membranous lupus nephritis: a survey of pediatric nephrologists and pediatric rheumatologists. J Rheumatol. 2017;44(11):1619–23. https://doi.org/10.3899/jrheum.170502.
•• Bajema IM, Wilhelmus S, Alpers CE, Bruijn JA, Colvin RB, Cook HT, et al. Revision of the International Society of Nephrology/Renal Pathology Society classification for lupus nephritis: clarification of definitions, and modified National Institutes of Health activity and chronicity indices. Kidney Int. 2018;93(4):789–96. https://doi.org/10.1016/j.kint.2017.11.023Consensus report to clarify definitions of pathologic lesions in kidney biopsies from patients with lupus nephritis, including new definitions for mesangial and endocapillary hypercellularity and for cellular, fibrocellular, and fibrous crescents. Furthermore, the report details phase 1 recommendations based on existing evidence and phase 2 recommendations for driving future research.
Weening JJ, D’Agati VD, Schwartz MM, Seshan SV, Alpers CE, Appel GB, et al. The classification of glomerulonephritis in systemic lupus erythematosus revisited. J Am Soc Nephrol. 2004;15(2):241–50. https://doi.org/10.1097/01.asn.0000108969.21691.5d.
Zappitelli M, Duffy C, Bernard C, Scuccimarri R, Watanabe Duffy K, Kagan R, et al. Clinicopathological study of the WHO classification in childhood lupus nephritis. Pediatr Nephrol (Berlin, Germany). 2004;19(5):503–10. https://doi.org/10.1007/s00467-004-1419-y.
Boneparth A, Ilowite N. Comparison of renal response parameters for juvenile membranous plus proliferative lupus nephritis versus isolated proliferative lupus nephritis: a cross-sectional analysis of the CARRA Registry. Lupus. 2014;23(9):898–904. https://doi.org/10.1177/0961203314531841.
Boneparth A, Wenderfer SE, Moorthy LN, Radhakrishna SM, Sagcal-Gironella AC, von Scheven E. Clinical characteristics of children with membranous lupus nephritis: the Childhood Arthritis and Rheumatology Research Alliance Legacy Registry. Lupus. 2016;26(3):299–306. https://doi.org/10.1177/0961203316662720.
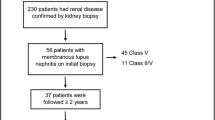
• Oni L, Beresford MW, Witte D, Chatzitolios A, Sebire N, Abulaban K, et al. Inter-observer variability of the histological classification of lupus glomerulonephritis in children. Lupus. 2017;26(11):1205–11. https://doi.org/10.1177/0961203317706558Pediatric biopsy study of 55 children with lupus nephritis, demonstrating utility of whole slide imaging and digital pathology to study inter-observer reproducibility of histopathologic features of lupus nephritis.
Parikh SV, Alvarado A, Malvar A, Rovin BH. The kidney biopsy in lupus nephritis: past, present, and future. Semin Nephrol. 2015;35(5):465–77. https://doi.org/10.1016/j.semnephrol.2015.08.008.
Moroni G, Depetri F, Ponticelli C. Lupus nephritis: when and how often to biopsy and what does it mean? J Autoimmun. 2016;74:27–40. https://doi.org/10.1016/j.jaut.2016.06.006.
Austin HA 3rd, Muenz LR, Joyce KM, Antonovych TT, Balow JE. Diffuse proliferative lupus nephritis: identification of specific pathologic features affecting renal outcome. Kidney Int. 1984;25(4):689–95. https://doi.org/10.1038/ki.1984.75.
Zappitelli M, Duffy CM, Bernard C, Gupta IR. Evaluation of activity, chronicity and tubulointerstitial indices for childhood lupus nephritis. Pediatr Nephrol (Berlin, Germany). 2008;23(1):83–91. https://doi.org/10.1007/s00467-007-0619-7.
Wilhelmus S, Alpers CE, Cook HT, Ferrario F, Fogo AB, Haas M, et al. The revisited classification of GN in SLE at 10 years: time to re-evaluate histopathologic lesions. J Am Soc Nephrol. 2015;26(12):2938–46. https://doi.org/10.1681/asn.2015040384.
• Rijnink EC, Teng YKO, Wilhelmus S, Almekinders M, Wolterbeek R, Cransberg K, et al. Clinical and histopathologic characteristics associated with renal outcomes in lupus nephritis. Clin J Am Soc Nephrol. 2017;12(5):734–43. https://doi.org/10.2215/CJN.10601016Biopsy study of 105 adults with lupus nephritis, demonstrating the utility of assessing fibrinoid necrosis, fibrous crescents, tubular atrophy, and interstitial fibrosis as baseline risk factors for predicting renal outcomes, and reporting a possible correlation between fibrinoid necrosis and future real flare.
• Londoño Jimenez A, Mowrey WB, Putterman C, Buyon J, Goilav B, Broder A. Tubulointerstitial damage in lupus nephritis: a comparison of the factors associated with tubulointerstitial inflammation and renal scarring. Arthritis & Rheumatol. 2018;70(11):1801–6. https://doi.org/10.1002/art.40575Pediatric biopsy study of 203 children with lupus nephritis, demonstrating the utility of assessing tubulointerstitial inflammation (TII) as a baseline risk factor for predicting renal outcomes, and reporting a possible inverse correlation with hydroxychloroquine use.
Chang A, Henderson SG, Brandt D, Liu N, Guttikonda R, Hsieh C, et al. In situ B cell-mediated immune responses and tubulointerstitial inflammation in human lupus nephritis. J Immunol. 2011 Feb 1;186(3):1849–60. https://doi.org/10.4049/jimmunol.1001983.
Leatherwood C, Speyer CB, Feldman CH, D’Silva K, Gómez-Puerta JA, Hoover PJ, et al. Clinical characteristics and renal prognosis associated with interstitial fibrosis and tubular atrophy (IFTA) and vascular injury in lupus nephritis biopsies. Seminars in Arthritis and Rheumatism. 2019. https://doi.org/10.1016/j.semarthrit.2019.06.002.
Coppo R, Peruzzi L, Amore A, Martino S, Vergano L, Lastauka I, et al. Dramatic effects of eculizumab in a child with diffuse proliferative lupus nephritis resistant to conventional therapy. Pediatr Nephrol. 2015;30(1):167–72. https://doi.org/10.1007/s00467-014-2944-y.
El-Husseini A, Hannan S, Awad A, Jennings S, Cornea V, Sawaya BP. Thrombotic microangiopathy in systemic lupus erythematosus: efficacy of eculizumab. American Journal of Kidney Diseases. 2015;65(1):127–30. https://doi.org/10.1053/j.ajkd.2014.07.031.
Zickuhr L, Herlitz LC, Chatterjee S. A 22-year-old woman with systemic lupus erythematosus presents with two damaged kidneys, one seizure, no platelets, and many possible diagnoses. Arthritis Care Res (Hoboken). 2018 Nov;70(11):1686–93. https://doi.org/10.1002/acr.23561.
Garcia D, Erkan D. Diagnosis and management of the antiphospholipid syndrome. N Engl J Med. 2018 May 24;378(21):2010–21. https://doi.org/10.1056/NEJMra1705454.
Bomback AS, Markowitz GS. Lupus Podocytopathy: a distinct entity. Clin J Am Soc Nephrol. 2016 Apr 7;11(4):547–8. https://doi.org/10.2215/CJN.01880216 [pii].
Almaani S, Prokopec SD, Zhang J, Yu L, Avila-Casado C, Wither J, et al. Rethinking lupus nephritis classification on a molecular level. J Clin Med. 2019;8(10):1524. https://doi.org/10.3390/jcm8101524.
Hahn BH, McMahon MA, Wilkinson A, Wallace WD, Daikh DI, Fitzgerald JD, et al. American College of Rheumatology guidelines for screening, treatment, and management of lupus nephritis. Arthritis Care Res. 2012 Jun;64(6):797–808. https://doi.org/10.1002/acr.21664.
Schwartz GJ, Munoz A, Schneider MF, Mak RH, Kaskel F, Warady BA, et al. New equations to estimate GFR in children with CKD. J Am Soc Nephrol. 2009 Mar;20(3):629–37. https://doi.org/10.1681/ASN.2008030287.
Illei GG, Austin HA, Crane M, Collins L, Gourley MF, Yarboro CH, et al. Combination therapy with pulse cyclophosphamide plus pulse methylprednisolone improves long-term renal outcome without adding toxicity in patients with lupus nephritis. Annals of internal medicine. 2001;135(4):248–57.
Moroni G, Quaglini S, Maccario M, Banfi G, Ponticelli C. “Nephritic flares” are predictors of bad long-term renal outcome in lupus nephritis. Kidney Int. 1996;50(6):2047–53.
Gordon C, Jayne D, Pusey C, Adu D, Amoura Z, Aringer M, et al. European consensus statement on the terminology used in the management of lupus glomerulonephritis. Lupus. 2009 Mar;18(3):257–63. https://doi.org/10.1177/0961203308100481.
Lee BS, Cho HY, Kim EJ, Kang HG, Ha IS, Cheong HI, et al. Clinical outcomes of childhood lupus nephritis: a single center’s experience. Pediatric nephrology (Berlin, Germany). 2007;22(2):222–31. https://doi.org/10.1007/s00467-006-0286-0.
Brunner HI, Higgins GC, Klein-Gitelman MS, Lapidus SK, Olson JC, Onel K, et al. Minimal clinically important differences of disease activity indices in childhood-onset systemic lupus erythematosus. Arthritis Care Res. 2010;62(7):950–9. https://doi.org/10.1002/acr.20154.
Brunner HI, Mina R, Pilkington C, Beresford MW, Reiff A, Levy DM, et al. Preliminary criteria for global flares in childhood-onset systemic lupus erythematosus. Arthritis Care Res. 2011;63(9):1213–23. https://doi.org/10.1002/acr.20507.
• Brunner HI, Holland M, Beresford MW, Ardoin SP, Appenzeller S, Silva CA, et al. American College of Rheumatology Provisional criteria for global flares in childhood-onset systemic lupus erythematosus. Arthritis Care Res (Hoboken). 2018;70(6):813–22. https://doi.org/10.1002/acr.23557With provisional endorsement, consensus criteria for measuring global flares in children with lupus are presented that be used as an outcome in future, interventional trials of lupus nephritis. In addition to renal outcome measures, this global flare definition can be used to monitor extra-renal manifestations of lupus.
Brunner HI, Feldman BM, Bombardier C, Silverman ED. Sensitivity of the Systemic Lupus Erythematosus Disease Activity Index, British Isles Lupus Assessment Group Index, and Systemic Lupus Activity Measure in the evaluation of clinical change in childhood-onset systemic lupus erythematosus. Arthritis Rheum. 1999 Jul;42(7):1354–60. https://doi.org/10.1002/1529-0131(199907)42:7<1354::AID-ANR8>3.0.CO;2-4.
Kidney Disease: Improving Global Outcomes (KDIGO) Glomerulonephritis Work Group t. KDIGO Clinical Practice Guideline for Glomerulonephritis: Lupus Nephritis. Kidney Inter Suppl. 2012;2:90–101. https://doi.org/10.1038/kisup.2012.25.
Groot N, Graeff N, Avcin T, Bader-Meunier B, Brogan P, Dolezalova P, et al. European evidence-based recommendations for diagnosis and treatment of childhood-onset systemic lupus erythematosus: the SHARE initiative. Ann Rheum Dis. 2017;76(11):1788–96. https://doi.org/10.1136/annrheumdis-2016-210960.
Gourley MF, Austin HA 3rd, Scott D, Yarboro CH, Vaughan EM, Muir J, et al. Methylprednisolone and cyclophosphamide, alone or in combination, in patients with lupus nephritis. A randomized, controlled trial. Ann Intern Med. 1996;125(7):549–57. https://doi.org/10.7326/0003-4819-125-7-199610010-00003.
• Cooper JC, Rouster-Stevens K, Wright TB, Hsu JJ, Klein-Gitelman MS, Ardoin SP, et al. Pilot study comparing the childhood arthritis and rheumatology research alliance consensus treatment plans for induction therapy of juvenile proliferative lupus nephritis. Pediatr Rheumatol Online J. 2018;16(1):65. https://doi.org/10.1186/s12969-018-0279-0The first study to assess adherence to the six CTPs for lupus nephritis classes III and IV in 41 adolescents across 10 pediatric rheumatology sites, demonstrating feasibility and efficacy of both cyclophosphamide and mycophenolic acid as induction immunosuppression. The report also highlights the challenge of consensus-building around dosing of corticosteroids in lupus studies.
Dooley MA, Hogan S, Jennette C, Falk R. Cyclophosphamide therapy for lupus nephritis: poor renal survival in black Americans. Glomerular Disease Collaborative Network Kidney Int. 1997;51(4):1188–95. https://doi.org/10.1038/ki.1997.162.
Isenberg D, Appel GB, Contreras G, Dooley MA, Ginzler EM, Jayne D, et al. Influence of race/ethnicity on response to lupus nephritis treatment: the ALMS study. Rheumatology (Oxford, England). 2010;49(1):128–40. https://doi.org/10.1093/rheumatology/kep346.
Houssiau FA, Vasconcelos C, D’Cruz D, Sebastiani GD, de Ramon GE, Danieli MG, et al. The 10-year follow-up data of the Euro-Lupus Nephritis Trial comparing low-dose and high-dose intravenous cyclophosphamide. Ann Rheum Dis. 2010;69(1):61–4. https://doi.org/10.1136/ard.2008.102533.
Access Trial Group T. Treatment of lupus nephritis with abatacept: the Abatacept and Cyclophosphamide Combination Efficacy and Safety Study. Arthritis Rheumatol. 2014;66(11):3096–104. https://doi.org/10.1002/art.38790.
Appel GB, Contreras G, Dooley MA, Ginzler EM, Isenberg D, Jayne D, et al. Mycophenolate mofetil versus cyclophosphamide for induction treatment of lupus nephritis. J Am Soc Nephrol. 2009;20(5):1103–12. https://doi.org/10.1681/ASN.2008101028.
Rovin BH, Furie R, Latinis K, Looney RJ, Fervenza FC, Sanchez-Guerrero J, et al. Efficacy and safety of rituximab in patients with active proliferative lupus nephritis: the lupus nephritis assessment with rituximab (LUNAR) study. Arthritis Rheum. 2012;64(4):1215–26. https://doi.org/10.1002/art.34359.
Pepper R, Griffith M, Kirwan C, Levy J, Taube D, Pusey C, et al. Rituximab is an effective treatment for lupus nephritis and allows a reduction in maintenance steroids. Nephrol Dial Transplant. 2009;24(12):3717–23. https://doi.org/10.1093/ndt/gfp336.
Roccatello D, Sciascia S, Baldovino S, Rossi D, Alpa M, Naretto C, et al. A 4-year observation in lupus nephritis patients treated with an intensified B-lymphocyte depletion without immunosuppressive maintenance treatment—clinical response compared to literature and immunological re-assessment. Autoimmun Rev. 2015;14(12):1123–30. https://doi.org/10.1016/j.autrev.2015.07.017.
Peterknecht E, Keasey MP, Beresford MW. The effectiveness and safety of biological therapeutics in juvenile-onset systemic lupus erythematosus (JSLE): a systematic review. Lupus. 2018;27(13):2135–45. https://doi.org/10.1177/0961203318804879.
• Zhang H, Liu Z, Zhou M, Liu Z, Chen J, Xing C, et al. Multitarget therapy for maintenance treatment of lupus nephritis. J Am Soc Nephrol. 2017;28(12):3671–8. https://doi.org/10.1681/asn.2017030263An open-label extension of large clinical trial, including 205 adult patients from China with lupus nephritis, demonstrating that the calcineurin inhibitor tacrolimus may increase sustained remission rates when used in combination with mycophenolic acid.
• Rovin BH, Solomons N, Pendergraft WF 3rd, Dooley MA, Tumlin J, Romero-Diaz J, et al. A randomized, controlled double-blind study comparing the efficacy and safety of dose-ranging voclosporin with placebo in achieving remission in patients with active lupus nephritis. Kidney Int. 2019;95(1):219–31. https://doi.org/10.1016/j.kint.2018.08.025Large clinical trial of 177 adult patients with lupus nephritis, demonstrating that the calcineurin inhibitor voclosporin may increase complete remission rates when used in combination with mycophenolic acid.
Willems M, Haddad E, Niaudet P, Kone-Paut I, Bensman A, Cochat P, et al. Rituximab therapy for childhood-onset systemic lupus erythematosus. J Pediatr. 2006;148(5):623–7. https://doi.org/10.1016/j.jpeds.2006.01.041.
Pereira T, Abitbol CL, Seeherunvong W, Katsoufis C, Chandar J, Freundlich M, et al. Three decades of progress in treating childhood-onset lupus nephritis. Clin J Am Soc Nephrol. 2011;6(9):2192–9. https://doi.org/10.2215/CJN.00910111.
Lehman TJ, Singh C, Ramanathan A, Alperin R, Adams A, Barinstein L, et al. Prolonged improvement of childhood onset systemic lupus erythematosus following systematic administration of rituximab and cyclophosphamide. Pediatr Rheumatol. 2014;12:3. https://doi.org/10.1186/1546-0096-12-3.
Watson L, Beresford MW, Maynes C, Pilkington C, Marks SD, Glackin Y, et al. The indications, efficacy and adverse events of rituximab in a large cohort of patients with juvenile-onset SLE. Lupus. 2015;24(1):10–7. https://doi.org/10.1177/0961203314547793.
Tambralli A, Beukelman T, Cron RQ, Stoll ML. Safety and efficacy of rituximab in childhood-onset systemic lupus erythematosus and other rheumatic diseases. J Rheumatol. 2015;42(3):541–6. https://doi.org/10.3899/jrheum.140863.
Jackson SW, Davidson A. BAFF inhibition in SLE—is tolerance restored? Immunol Rev. 2019;292:1–18. https://doi.org/10.1111/imr.12810.
Ruperto N, Abud-Mendoza C, Viola DO, Calvo I, Levy DM, Gallegos JC, et al. FRI0181 the PLUTO study: intravenous belimumab in children with systemic lupus erythematosus. Ann Rheum Dis. 2019;78(Suppl 2):764–5. https://doi.org/10.1136/annrheumdis-2019-eular.4884.
Aragon E, Resontoc LP, Chan YH, Lau YW, Tan PH, Loh HL, et al. Long-term outcomes with multi-targeted immunosuppressive protocol in children with severe proliferative lupus nephritis. Lupus. 2016;25(4):399–406. https://doi.org/10.1177/0961203315615220.
Chen W, Tang X, Liu Q, Fu P, Liu F, Liao Y, et al. Short-term outcomes of induction therapy with tacrolimus versus cyclophosphamide for active lupus nephritis: a multicenter randomized clinical trial. Am J Kidney Dis. 2011;57(2):235–44. https://doi.org/10.1053/j.ajkd.2010.08.036.
Fu LW, Yang LY, Chen WP, Lin CY. Clinical efficacy of cyclosporin a neoral in the treatment of paediatric lupus nephritis with heavy proteinuria. Br J Rheumatol. 1998;37(2):217–21. https://doi.org/10.1093/rheumatology/37.2.217.
Bao H, Liu ZH, Xie HL, Hu WX, Zhang HT, Li LS. Successful treatment of class V+IV lupus nephritis with multitarget therapy. J Am Soc Nephrol. 2008;19(10):2001–10. https://doi.org/10.1681/ASN.2007121272.
. Rovin BH, Caster DJ, Cattran DC, Gibson KL, Hogan JJ, Moeller MJ, et al. Management and treatment of glomerular diseases (part 2): conclusions from a Kidney Disease: Improving Global Outcomes (KDIGO) Controversies Conference. Kidney Int. 2019;95(2):281–95. https://doi.org/10.1016/j.kint.2018.11.008Consensus report that identifies controversies for the management of lupus nephritis in both adults and children, including an examination of data on disease pathogenesis, biomarkers, and treatments to identify areas of consensus.
Ardoin SP, Daly RP, Merzoug L, Tse K, Ardalan K, Arkin L, et al. Research priorities in childhood-onset lupus: results of a multidisciplinary prioritization exercise. Pediatr Rheumatol. 2019;17(1):32. https://doi.org/10.1186/s12969-019-0327-4.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Wenderfer serves as a co-chair for the Nephritis Working Group for the SLE Committee at the Childhood Arthritis and Rheumatology Research Alliance (CARRA).
Drs. Hicks and Chang declare no conflict of interest.
Human and Animal Rights and Informed Consent
All reported studies/experiments with human or animal subjects performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsinki declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Renal
Rights and permissions
About this article
Cite this article
Wenderfer, S.E., Chang, J. & Hicks, M.J. Approach to Classification and Management of Childhood-Onset Lupus Nephritis. Curr Pediatr Rep 8, 26–35 (2020). https://doi.org/10.1007/s40124-020-00207-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40124-020-00207-8