Abstract
Introduction
The aim of this work is to evaluate the effect of mesenchymal stem cell transplantation (MSCT) and cultivated limbal epithelial transplantation (CLET) therapies on the limbus of patients suffering from limbal stem cell deficiency (LSCD).
Methods
A sub-analysis of a phase I–II randomized, controlled, and double-masked clinical trial was performed to assess the changes in the anatomical structures of the limbus. In vivo confocal microscopy (IVCM) analysis was carried out in LSCD eyes before and 12 months after allogeneic MSCT or CLET. Epithelial phenotype of the central cornea, as well as the presence of transition zones and palisades of Vogt in the limbus, were assessed using Wilcoxon test.
Results
Twenty-three LSCD (14 MSCT and nine CLET) eyes were included. The epithelial phenotype of the central cornea improved significantly (p < 0.001) from 15 (eight MSCT, seven CLET) and eight (six MSCT, two CLET) LSCD eyes showing conjunctival and mixed phenotypes, respectively, to eight (five MSCT, three CLET), five (two MSCT, three CLET), and ten (seven MSCT, three CLET) eyes showing conjunctival, mixed, and corneal phenotypes, respectively. Transition areas and palisades of Vogt were observed in at least one quadrant in nine (five MSCT, four CLET) and 16 (nine MSCT, seven CLET), and in four (two MSCT, two CLET) and six (three MSCT, three CLET) LSCD eyes before and after surgery, respectively. Changes in the transition zones and palisades were solely significant (p = 0.046) for the nasal and inferior quadrants, respectively.
Conclusions
MSCT and CLET improved the central corneal epithelial phenotype despite only minor changes in the anatomical structures of the limbus, as detected by IVCM technology.
Trial Registration
ClinicalTrials.gov identifier, NCT01562002.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Limbal stem cell deficiency (LSCD) can be managed by cultivated limbal epithelial transplantation (CLET); however, further innovative approaches like mesenchymal stem cell transplantation (MSCT) are being developed. |
A previous clinical trial showed that MSCT can improve the healthiness of the cornea as much as CLET in LSCD eyes. However, the changes occurring in the limbal niche after MSCT have not yet been reported. |
What was learned from the study? |
The changes in the transition zones and palisades of Vogt after transplantation surgery are minor. |
MSCT could provide similar changes as CLET in the anatomical structures of the limbal niche using in vivo confocal microscopy technology. |
Future clinical trials including a higher number of patients should be performed to better characterize the changes occurring in the corneo-scleral limbal niche after cell transplantation. Additionally, techniques to locate transplanted stem cells in the human living eye would provide invaluable information. |
Introduction
The sclerocorneal limbus, the transition area between the corneal and conjunctival epithelium of the ocular surface, is the niche of the limbal epithelial stem cells (LESC). The specific niche site is the basal epithelium of the palisades of Vogt, formed by limbal crypts and ridges. It is responsible for the adequate homeostasis and continuous regeneration of the corneal epithelium. The limbus also acts as a physical barrier that prevents the migration of conjunctival cells and blood vessels onto the cornea [1,2,3].
Damage or dysfunction of LESC or the niche induces limbal stem cell deficiency (LSCD), which prevents the normal regeneration of the corneal epithelium. This clinical alteration can be triggered by different diseases such as congenital aniridia, severe ocular surface inflammation, chemical burns, or multiple surgeries, among others [4, 5]. LSCD causes recurrent epithelial defects, corneal ulcerations, neovascularization, conjunctivalization, and squamous metaplasia [6, 7]. Consequently, the LSCD patient usually suffers from photophobia, decreased vision, inflammation, blepharospasm, and pain [4, 5, 8, 9].
Up to now, many different approaches have been used to treat LSCD [10, 11]. Among them, cultivated limbal epithelial transplantation (CLET) from an autologous or allogeneic small limbal biopsy is the most common stem cell-based treatment. This therapy provides a source of stem cells to regenerate the normal corneal epithelium resulting in clinical improvements [12,13,14]. In this regard, our research group has wide experience improving the techniques for cultivating LESC [15,16,17,18,19], and clinical management of LSCD, including CLET [13, 20].
In the last decades, the use of mesenchymal stem cells (MSC) for regenerative medicine has grown significantly due to their beneficial properties. MSC have immunosuppressive functions by inhibiting proliferation, differentiation, and chemotaxis of B cells in inflamed tissues, where MSC can migrate [21, 22]. MSC also have non-immunogenic characteristics allowing them to perform allogeneic transplantation without immunosuppression [23]. Therefore, the benefits of MSC for the treatment of ocular surface alterations have been extensively studied in experimental models [24,25,26,27]. Moreover, our research group performed the first clinical trial in human eyes as a proof-of-concept demonstrating that MSC transplantation (MSCT) can be as safe and effective as CLET for LSCD management [28].
In vivo confocal microscopy (IVCM) is a non-invasive technique that allows high-resolution imaging of the cornea; thus, it has become an appropriate tool for studying corneal anomalies [29]. The first report of this clinical trial showed that eyes undergoing MSCT obtained similar improvement in the epithelial phenotype of the central cornea than CLET ones [28]. However, no previous study has reported if MSCT can also have a positive effect on limbal niche structures in LSCD eyes. Consequently, the objective of this sub-analysis from a phase I–II clinical trial was to assess the effect of MSCT and CLET on the limbal anatomical structures of LSCD eyes as measured with IVCM technique.
Methods
The protocol of the clinical trial was approved by the University Hospital Ethics Committee and the Spanish Agency for Medicine and Medical Devices (AEMPS). This study followed the principles of the Declaration of Helsinki, the Good Manufacturing and Clinical Practice guidelines, and the European Union Tissues and Cells Directive. All patients signed the written informed consent after the nature of the study was explained.
The present study is a sub-analysis of a proof-of-concept phase I–II randomized, controlled, and double-masked clinical trial (EudraCT 2010-023535-42; ClinicalTrials.gov Identifier: NCT01562002). This sub-analysis was performed because changes in the limbal structures of LSCD eyes after CLET or MSCT were not included as a primary or secondary outcome measure of the clinical trial. The specific details pertaining to the clinical trial design, patient characteristics, randomization and masking, procedures and primary evaluation endpoints have been already widely detailed [28]. Briefly, recruited patients had unilateral or bilateral, severe and/or total corneal epithelial failure due to LSCD, with blindness or low vision due to central corneal opacification. Allogeneic bone marrow-derived MSC and limbal epithelial cells isolated from a cadaveric limbal biopsy were cultured on amniotic membrane and later transplanted to the ocular surface. The cell dose in MSCT was around 250,000 cells per graft. All scheduled transplants were randomly allocated to CLET or MSCT.
In Vivo Confocal Microscopy of the Limbal Niche
The Heidelberg Retinal Tomograph version 3 (HRT3) with a Rostock cornea module (RCM) (RCM-HRT3) (Heidelberg GmbH, Heidelberg, Germany) was used to analyze the corneal and limbal areas before and after transplantation. Disposable and sterile contact caps (TomoCap® Heidelberg GmbH) were used to allow contact between the cornea and the objective lens of the IVCM. A lubricating gel (Viscotears® 0.2% with Carbomero 980; Novartis, Basel, Switzerland) was used to cover and fill the corneal contact caps. Also, topical anesthesia (tetracaine 0.1% and oxybuprocaine 0.4%; Alcon Cusí, Barcelona, Spain) was used prior to IVCM image acquisition. High-contrast digital images with a field of view of 400 × 400 μm (0.16 mm2) were acquired. The transverse resolution and thickness of the optical sections were 2 and 4 μm, respectively. Sequential scans of the central cornea and superior, inferior, temporal, and nasal limbus (12, 3, 6, 9 o’clock positions) using the manual frame acquisition technique were obtained following methods previously described [13, 20]. A minimum of 40 z-scan images were visualized at each examination point from the epithelium to the stroma in the central cornea, or to the palisades of Vogt in the limbus. To increase the likelihood of assessing the same location, external fixation targets were presented to the contralateral eye—one distance target for the central cornea and four eccentric ones for each quadrant of the limbus. Central cornea scans were performed to assess the phenotype of the central epithelium. Cell morphology was classified as corneal, conjunctival, or mixed-type depending on the IVCM findings [30, 31]. When classifying the central phenotype, corneal epithelium was considered as a multi-layered anatomical structure having polygonal and flat cells with hyperreflective nuclei in the superficial layer, progressively decreasing in size in the intermediate layers, and small cells without detectable nuclei with reflective borders in the basal layer [32]; and the conjunctival epithelium as a stratified anatomical structure of cuboidal or polygonal cells having hyporeflective cytoplasm with or without detectable nuclei, and barely defined borders [30, 33]. Limbal scans were performed to assess the presence or absence of palisades of Vogt and the morphologic transition of epithelial cells from corneal to conjunctival phenotype. The palisades of Vogt were defined as radial hyperreflective stromal ridges that follow a branching or interconnecting pattern alternated with columns of limbal basal epithelium (rete pegs) [30, 34, 35].
Central cornea epithelial phenotype and limbal IVCM images were acquired before and 12 months after MSCT and CLET therapies. The IVCM images were obtained and later analyzed, always by the same experienced researcher (I.P.S.) using the Heidelberg Eye Explorer software (V. 1.5.10.0. 2006; Heidelberg GmbH) to avoid interobserver variability. The main outcomes of the IVCM analysis were the epithelial phenotype of the central cornea (corneal, conjunctival, or mixed), and the presence or absence of transition zones and palisades of Vogt in the four quadrants of the limbus.
Statistical Analysis
Statistical analysis was performed using R statistical package version 4.0.0. Quantitative characteristics were expressed as mean ± standard deviation (SD), and qualitative variables were described as numbers and percentages. McNemar's test was used to assess changes in the dichotomous variables before and 12 months after transplantation surgery, while Wilcoxon test was used for ordinal variables. To assess if there were any relationships between the changes in the epithelial phenotype of the central cornea after surgery and the changes in the palisades of Vogt and transition zones of the limbus, Mann–Whitney test was used.
Results
Clinical Trial Sample
Twenty-three transplants reached 12-month follow-up in the original clinical trial; thus, they were included in this study. However, in two LSCD eyes (both from the MSCT group) it was not possible to obtain high-quality IVCM images in any limbal quadrant. Considering the whole sample (n = 23), nine transplants belonged to the CLET group and 14 to the MSCT group. There were 12 females and 11 males with a mean age of 46.1 ± 11.5 years. The etiology of the LSCD in the 23 eyes was 13 chemical injuries, four Stevens–Johnson syndromes, two congenital aniridias, one graft-versus-host disease, one atopic keratoconjunctivitis, one sequela from multiple surgeries, and one from infectious keratitis.
Central Corneal In Vivo Confocal Microscopy Analysis
Before surgery, 15 (eight MSCT and seven CLET) and eight (six MSCT and two CLET) LSCD eyes showed conjunctival and mixed epithelial phenotype for the central cornea, respectively. Twelve months after surgery, a conjunctival, mixed, and corneal epithelial phenotype was observed in eight (five MSCT and three CLET), five (two MSCT and three CLET), and ten (seven MSCT and three CLET) LSCD eyes, respectively. The improvement of the central corneal epithelial phenotype was significant not only for the whole sample (p < 0.001), but also for both the MSCT (p = 0.015) and the CLET (p = 0.026) groups.
Limbal In Vivo Confocal Microscopy Analysis
Transition areas between corneal and conjunctival epithelium in any of the four quadrants of the limbus were found in nine (five MSCT and four CLET) LSCD eyes before surgery and in 16 (nine MSCT and seven CLET) LSCD eyes 12 months after cell transplantation. This change was only statistically significant (p = 0.046) for the nasal quadrant considering the total sample (Fig. 1), however, both MSCT (p = 0.31) and CLET (p = 0.08) groups independently did not show significant changes. Besides, there was not a significant association between the improvement in the epithelial phenotype of the central cornea and the higher number of transition zones observed (p ≥ 0.43).
Number (and percentage) of eyes suffering from limbal stem cell deficiency that showed transition zones in each quadrant of the limbus before and 1 year after mesenchymal stem cell transplantation (MSCT) and cultivated limbal epithelial transplantation (CLET). *Statistically significant (p = 0.046) differences before (baseline) and after transplantation surgery
Regarding the palisades of Vogt, they were found in any of the limbal quadrants in four (two MSCT and two CLET) LSCD eyes before surgery, and it increased to six (three MSCT and three CLET) LSCD eyes 12 months after surgery. This minor change was only significant in the inferior quadrant (p = 0.046) for the whole sample (Fig. 2). However, changes in the MSCT and CLET group were not significant (p = 0.08 and p = 0.31, respectively). There was not a significant (p ≥ 0.15) relationship between the improvement in the epithelial phenotype of the central cornea and the changes in the detection of palisades of Vogt. Representative cases of successful MSCT and CLET cases are shown in Figs. 3 and 4. Unsuccessful representative cases, in terms of absence of improvement in the limbus, are also shown in Fig. 1S and 2S (Supplementary material).
Number (and percentage) of limbal stem cell deficiency (LSCD) eyes that showed palisades of Vogt in each quadrant of the limbus before and 1 year after mesenchymal stem cell transplantation (MSCT) and cultivated limbal epithelial transplantation (CLET). *Statistically significant (p = 0.046) differences before (baseline) and after transplantation surgery
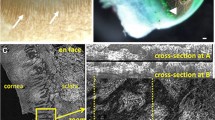
A representative example of a successful mesenchymal stem cell transplantation (MSCT) case. Slit-lamp biomicroscopy images before treatment and 12 months after MSCT are shown (left panel). In vivo confocal microscopy (IVCM) images of the central cornea show an improvement from a conjunctival-like to a mixed epithelial phenotype before and 12 months after surgery, respectively. IVCM images of the limbus show an absence of transition zones (nasal quadrant) and palisades of Vogt (inferior quadrant) before transplantation (baseline). In contrast, 12 months after MSCT surgery, a transition zone and limbal palisade ridges were detected in the same quadrants (nasal and inferior, respectively)
A representative example of a successful cultivated limbal epithelial transplantation (CLET) case. Left panels show slit-lamp biomicroscopy images before and 12 months after CLET. In vivo confocal microscopy (IVCM) images of the central cornea show improvement from a conjunctival-like to a mixed epithelial phenotype 12 months after CLET. Limbal IVCM images obtained 12 months after CLET show the presence of an abrupt transition zone in the nasal quadrant, and oval-shaped focal stromal projections typically observed in the palisades of Vogt (inferior quadrant)
Discussion
Our research group performed a pilot clinical trial to assess if MSCT therapy was as safe and efficient as CLET to treat LSCD eyes. A healthier corneal epithelium was achieved in 85.7 and 77.8% of MSCT and CLET cases, respectively [28]. However, histological and anatomical changes in the limbus were not considered as primary or secondary endpoints of the study, thus they were not reported. IVCM technique allows us to obtain minimally invasive in vivo images of the corneal epithelium and the limbal area, which can be evaluated in situ to better evaluate the success or failure of the treatments [33, 36, 37]. There are several publications analyzing the limbal niche by IVCM after surgical techniques, including CLET [20, 33, 36, 38], however, no report exists addressing the limbal changes after MSCT. Therefore, the present sub-analysis from a phase I–II clinical trial was carried out to assess if limbal areas in LSCD eyes could also show some histological regeneration after MSCT therapy.
The IVCM images of the central cornea obtained in the present clinical trial showed an improvement in the central corneal epithelial phenotype 12 months after both stem cell type transplantations. These results are like the ones reported by Pedrotti et al. [33], who observed that 46.1% of 13 LSCD eyes exhibited corneal phenotype and 30.8% had a mixed phenotype 1 year after autologous CLET surgery. Likewise, in the study of Mastropascua et al. [36], including six LSCD eyes after 12 months of autologous CLET, a corneal phenotype was observed in 50% of eyes and a mixed phenotype in 33.3% of the cases.
In the limbus of the healthy human cornea, a progressive transition of epithelial cells from corneal to conjunctival epithelial phenotype can be observed by IVCM [34]. However, this regular epithelial transition is usually altered in LSCD eyes [30]. Consequently, in the present sub-analysis of the clinical trial, we assessed if the detection of the transition zone was higher after transplantation because it can be considered suggestive of restoration of limbal function. Twelve months after surgery, the improvement in the transition zones was solely significant for the nasal quadrant considering the total sample. Although the sample size of the present clinical trial is higher than other studies assessing transplantation in LSCD eyes [33, 36], when we analyzed the two different transplantation groups, the statistical power was reduced for each group, and it might have played a role in the absence of statistically significant changes after surgery for each group. Pedrotti et al. [33] have also observed similar findings to ours. They reported a higher number of transition zones in LSCD eyes (n = 13) after CLET. Specifically, in 46.1% of the cases, the transition zone was fully present and in 30.8% cases, it was partially present 1 year after surgery. Mastropasqua et al. [36] have also assessed changes in the superficial morphology of the limbus after CLET, reporting that all six of their cases showed an abrupt transition from corneal to conjunctival epithelial phenotype.
The detection of palisades of Vogt in LSCD eyes is important not only because it is an indicator of a healthy histology but also because they play an essential role in maintaining the normal state and function of LESC [3]. In the present clinical trial, after surgery, only two more LSCD eyes showed palisades of Vogt in at least one quadrant. This minor change was only significant for the inferior quadrant considering the whole sample. Previous authors have also assessed the presence of palisades of Vogt after transplantation surgery. Both Pedrotti et al. [33] and Mastropasqua et al. [36] have reported the absence of recovery of palisades of Vogt after CLET.
The outcomes of the present clinical trial and those previously reported [33, 36, 38] showed slight histological changes in the limbus after transplantation surgery when assessing the transition from conjunctival to corneal epithelial phenotype. However, major histological improvements in the limbus, like the appearance of palisades of Vogt after surgery, might be much more difficult to observe. In the present study, a healthier epithelial phenotype in the central cornea, in addition to a higher number of transition zones in the limbus, was observed. However, the relationship between both improvements was not significant. Previous authors [33] have shown that it is possible to observe improvements in the epithelial phenotype of the central cornea without detecting palisades of Vogt in the limbus after transplantation. Thus, improvements in the corneal epithelial phenotype can be detected in the absence of a normal limbal stem cell niche. In fact, it has been previously hypothesized that if stem cells are located after surgery in different positions within the cornea (e.g., basal layers of corneal epithelium), they might be able to sustain the corneal surface cell mass [33].
The differences in the recovery of the limbal architecture after transplantation among different studies could be related to several factors, including the etiology and severity of the LSCD eyes included in each study, or the number of the transplanted cells (250,000 in the present clinical trial) and even the administration route. Most of the eyes included in the present clinical trial and other studies suffered from LSCD due to chemical burns. However, the severity of the ocular injury usually depends on the contact surface area and the degree of penetration of the alkaline or acid. Thus, outcomes after transplantation are very likely to vary depending on the LSCD severity before surgery. Besides, once the safety and efficacy of MSCT have been already demonstrated by our research group [28], further clinical trials must be conducted using alternative routes for cell administration, such as subconjunctival injections, which can increase the number of cells administered [26].
In this sub-analysis study, some changes were observed in the limbus 1 year after transplantation. However, the secretion of different paracrine factors by the transplanted cells could also be implicated in the regeneration of the central corneal epithelium. Corneal wound healing depends on the presence of growth factor, such us epidermal growth factor (EGF), whose topical administration has been demonstrated to improve the corneal epithelial wound closure, keratinocyte growth factor, hepatocyte growth factor, and transforming growth factor (TGF), among others [39]. In this regard, both LESC and MSC secrete paracrine growth factors, which might have contributed to the corneal epithelium regeneration. In addition, limbal epithelial cells secrete different factors like the mediator of immunological system regulation TGF-α and β, tumor necrosis factor (TNF), fibroblast growth factor (FGF), and leukemia inhibitory factor [40]. Besides, several significant factors are also secreted by MSC, such as EGF, pigment epithelium-derived factor (PEDF), TGF-β, and the tumor necrosis factor-inducible gene 6 protein, which are implicated in neuropathic pain inhibition, present anti-inflammatory properties, stimulate limbal stem cell colony-forming efficiency, and prevent neovascularization [41, 42].
The present sub-analysis from a phase I–II clinical trial has some limitations. First, although the assessment of the limbus in LSCD eyes using IVCM technique is very useful to image the cornea and limbus, it is still a semi-automatic diagnostic technique that relies on the ability and experience of the clinician to obtain high-quality images, and the assessment is still subjective and very difficult in advanced LSCD eyes due to light scattering [33]. Moreover, the technique requires contact, which can cause discomfort to the patient, and increases the difficulty of image acquisition. In fact, in the present clinical trial, it was not possible to obtain IVCM images in any of the four limbal quadrants in two LSCD eyes, despite successful central corneal assessment. In addition, in some LSCD eyes, it was not possible to obtain high-quality images in all limbal quadrants. Thus, although we observed a minor change in the detection of palisades of Vogt in the inferior quadrant after transplantation, detection of palisades in any quadrant might be missed during baseline assessment, because adequate detection is much more difficult in LSCD eyes than in normal ones or healthier corneas (i.e., after transplantation surgery). Second, the sample size of this study can be considered adequate in comparison with previous studies assessing the outcomes of transplantation surgeries in LSCD. However, when the MSCT and CLET groups were independently analyzed, the statistical power was reduced, and the change previously observed in the limbal structures lost its statistical significance. Fortunately, it was possible to recruit enough LSCD eyes to show that MSCT provided similar histological changes in the central cornea and limbus as eyes undergoing CLET.
Conclusions
The present sub-analysis from a phase I–II clinical trial showed that MSCT provides similar changes in the histological structures of the limbal niche as CLET technique, using IVCM technology 1 year after transplantation surgery. Regardless of the transplantation technique, healthier transition zones from corneal to conjunctival-like epithelium in the limbus can be observed. However, detection of a higher number of palisades of Vogt after surgery might not be achieved, although an improvement of the epithelial phenotype of the central cornea is very likely to be observed. Future studies should be carried out to further assess the ability of MSCT and CLET techniques to provide a healthier limbus in larger sample sizes, including other LSCD etiologies.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Tseng SC. Concept and application of limbal stem cells. Eye Lond Engl. 1989;3:141–57.
Cotsarelis G, Cheng SZ, Dong G, Sun TT, Lavker RM. Existence of slow-cycling limbal epithelial basal cells that can be preferentially stimulated to proliferate: implications on epithelial stem cells. Cell. 1989;57:201–9.
Li W, Hayashida Y, Chen YT, Tseng SC. Niche regulation of corneal epithelial stem cells at the limbus. Cell Res. 2007;17:26–36.
Dua HS, Saini JS, Azuara-Blanco A, Gupta P. Limbal stem cell deficiency: concept, aetiology, clinical presentation, diagnosis and management. Indian J Ophthalmol. 2000;48:83–92.
Sejpal K, Bakhtiari P, Deng SX. Presentation, diagnosis and management of limbal stem cell deficiency. Middle East Afr J Ophthalmol. 2013;20:5–10.
Ahmad S, Osei-Bempong C, Dana R, Jurkunas U. The culture and transplantation of human limbal stem cells. J Cell Physiol. 2010;225:15–9.
Shortt AJ, Tuft SJ, Daniels JT. Corneal stem cells in the eye clinic. Br Med Bull. 2011;100:209–25.
Chan EH, Chen L, Yu F, Deng SX. Epithelial thinning in limbal stem cell deficiency. Am J Ophthalmol. 2015;160:669–77.
Deng SX, Borderie V, Chan CC, et al. Global consensus on definition, classification, diagnosis, and staging of limbal stem cell deficiency. Cornea. 2019;38:364–75.
Figueiredo FC, Glanville JM, Arber M, et al. A systematic review of cellular therapies for the treatment of limbal stem cell deficiency affecting one or both eyes. Ocul Surf. 2021;20:48–61.
Calonge M, Nieto-Miguel T, de la Mata A, et al. Goals and challenges of stem cell-based therapy for corneal blindness due to limbal deficiency. Pharmaceutics. 2021;16(13):1483.
Atallah MR, Palioura S, Perez VL, Amescua G. Limbal stem cell transplantation: current perspectives. Clin Ophthalmol. 2016;10:593–602.
Ramirez BE, Sanchez A, Herreras JM, et al. Stem cell therapy for corneal epithelium regeneration following good manufacturing and clinical procedures. BioMed Res Int. 2015;2015: 408495.
Rama P, Matuska S, Paganoni G, Spinelli A, De Luca M, Pellegrini G. Limbal stem-cell therapy and long-term corneal regeneration. N Engl J Med. 2010;363:147–55.
López-Paniagua M, Nieto-Miguel T, de la Mata A, et al. Comparison of functional limbal epithelial stem cell isolation methods. Exp Eye Res. 2016;146:83–94.
López-Paniagua M, Nieto-Miguel T, de la Mata A, et al. Consecutive expansion of limbal epithelial stem cells from a single limbal biopsy. Curr Eye Res. 2013;38:537–49.
López-Paniagua M, Nieto-Miguel T, de la Mata A, et al. Successful consecutive expansion of limbal explants using a biosafe culture medium under feeder layer-free conditions. Curr Eye Res. 2017;42:685–95.
De la Mata A, Nieto T, Paniagua M, Galindo S, et al. Chitosan-gelatin biopolymers as carrier substrata for limbal epithelial stem cells. J Mater Sci Mater Med. 2013;24:2819–29.
De la Mata A, Mateos-Timoneda MA, Nieto-Miguel T, et al. Poly-l/dl-lactic acid films functionalized with collagen IV as carrier substrata for corneal epithelial stem cells. Colloids Surf B Biointerfaces. 2019;177:121–9.
Ramírez BE, Victoria DA, Murillo GM, Herreras JM, Calonge M. In vivo confocal microscopy assessment of the corneoscleral limbal stem cell niche before and after biopsy for cultivated limbal epithelial transplantation to restore corneal epithelium. Histol Histopathol. 2015;30:183–92.
Chamberlain G, Fox J, Ashton B, Middleton J. Concise review: mesenchymal stem cells: their phenotype, differentiation capacity, immunological features, and potential for homing. Stem Cells. 2007;25:2739–49.
Nauta AJ, Fibbe WE. Immunomodulatory properties of mesenchymal stromal cells. Blood. 2007;110:3499–506.
Krampera M, Pasini A, Pizzolo G, Cosmi L, Romagnani S, Annunziato F. Regenerative and immunomodulatory potential of mesenchymal stem cells. Curr Opin Pharmacol. 2006;6:435–41.
Galindo S, Herreras JM, López-Paniagua M, et al. Therapeutic effect of human adipose tissue-derived mesenchymal stem cells in experimental corneal failure due to limbal stem cell niche damage. Stem Cells. 2017;35:2160–74.
Nieto-Miguel T, Galindo S, López-Paniagua M, Pérez I, Herreras JM, Calonge M. Cell therapy using extraocular mesenchymal stem cells. In: Alió N, Alió Barrio J, Arnalich-Montiel F, editors. Corneal Regen. Essent ophthalmol. Cham: Springer; 2019.
Galindo S, de la Mata A, López-Paniagua MJ. Subconjunctival injection of mesenchymal stem cells for corneal failure due to limbal stem cell deficiency: state of the art. Stem Cell Res Ther. 2021;12:60.
Al-Jaibaji O, Swioklo S, Connon CJ. Mesenchymal stromal cells for ocular surface repair. Expert Opin Biol Ther. 2019;19:643–53.
Calonge M, Pérez I, Galindo S, et al. A proof-of-concept clinical trial using mesenchymal stem cells for the treatment of corneal epithelial stem cell deficiency. Transl Res. 2019;206:18–40.
Le Q, Xu J, Deng SX. The diagnosis of limbal stem cell deficiency. Ocul Surf. 2018;16:58–69.
Nubile M, Lanzini M, Miri A, et al. In vivo confocal microscopy in diagnosis of limbal stem cell deficiency. Am J Ophthalmol. 2013;155:220–32.
Chidambaranathan GP, Mathews S, Panigrahi AK, Mascarenhas J, Prajna NV, Muthukkaruppan V. In vivo confocal microscopic analysis of limbal stroma in patients with limbal stem cell deficiency. Cornea. 2015;34:1478–86.
Eckard A, Stave J, Guthoff RF. In vivo investigations of the corneal epithelium with the confocal Rostock laser scanning microscope (RLSM). Cornea. 2006;25:127–31.
Pedrotti E, Passilongo M, Fasolo A, et al. In vivo confocal microscopy 1 year after autologous cultured limbal stem cell grafts. Ophthalmology. 2015;122:1660–8.
Patel DV, Sherwin T, McGhee CNJ. Laser scanning in vivo confocal microscopy of the normal human corneoscleral limbus. Invest Ophthalmol Vis Sci. 2006;47:2823–7.
Miri A, Al-Aqaba M, Otri AM, et al. In vivo confocal microscopic features of normal limbus. Br J Ophthalmol. 2012;96:530–6.
Mastropasqua L, Calienno R, Lanzini M, et al. In vivo confocal microscopy of the sclerocorneal limbus after limbal stem cell transplantation: looking for limbal architecture modifications and cytological phenotype correlations. Mol Vis. 2016;22:748–60.
Chan EH, Chen L, Rao JY, Yu F, Deng SX. Limbal basal cell density decreases in limbal stem cell deficiency. Am J Ophthalmol. 2015;160:678–84.
Hong J, Zheng T, Xu J, et al. Assessment of limbus and central cornea in patients with keratolimbal allograft transplantation using in vivo laser scanning confocal microscopy: an observational study. Graefes Arch Clin Exp Ophthalmol A. 2011;249:701–8.
Yu F-SX, Yin J, Xu K, Huang J. Growth factors and corneal epithelial wound healing. Brain Res Bull. 2010;81:229–35.
Loureiro RR, Gomes JÁP. Biological modulation of corneal epithelial wound healing. Arq Bras Oftalmol. 2019;82:78–84.
Dabrowski FA, Burdzinska A, Kulesza A, et al. Comparison of the paracrine activity of mesenchymal stem cells derived from human umbilical cord, amniotic membrane and adipose tissue. J Obstet Gynaecol Res. 2017;43:1758–68.
Oh JY, Roddy GW, Choi H, et al. Anti-inflammatory protein TSG-6 reduces inflammatory damage to the cornea following chemical and mechanical injury. Proc Natl Acad Sci USA. 2010;107:16875–80.
Funding
This work was supported by Proyectos de Generación de Conocimiento Program (Grant PID2021-125142OA-I00 MCIN/AEI/10.13039/501100011033/FEDER, UE) and Retos Investigación (Grant PID2019-105525RB-100/AEI/10.13039/501100011033, MICINN/FEDER, EU) Programs, Ministry of Science and Innovation, Spain; the Advanced Therapies Program (Grant SAS/2377/2010 EC10-256), Ministry of Health, Spain; Institute of Health Carlos III, CIBER-BBN (CB06/01/003 MICINN/FEDER, EU), Spain; and the Regional Center for Regenerative Medicine and Cell Therapy, Castilla y León, Spain. The funding organizations had no role in the design or conduct of this research. The journal’s fee for this article was waived.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Inmaculada Pérez, Sara Galindo, Alberto López-Miguel, Teresa Nieto-Miguel, Ana de la Mata, Marina López-Paniagua, Mercedes Alberca, José M. Herreras, and Margarita Calonge. The first draft of the manuscript was written by Inmaculada Pérez, Sara Galindo, Teresa Nieto-Miguel, Marina López-Paniagua and Ana de la Mata, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
Inmaculada Pérez, Sara Galindo, Alberto López-Miguel, Teresa Nieto-Miguel, Ana de la Mata, Marina López-Paniagua, Mercedes Alberca, José M. Herreras, and Margarita Calonge declare that they have no competing interests.
Ethical Approval
The Ethics Committee of the Valladolid University Hospital prospectively approved this clinical trial (Ref: HCUV-CASVE-11-108). This study followed the principles of the Declaration of Helsinki of 1964 and its later amendments. All patients signed the written informed consent after the nature of the study was explained.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Pérez, I., Galindo, S., López-Miguel, A. et al. In Vivo Confocal Microscopy in Limbal Stem Cell Deficiency After Mesenchymal Stem Cell Transplantation: A Sub-analysis from a Phase I–II Clinical Trial. Ophthalmol Ther 12, 3251–3262 (2023). https://doi.org/10.1007/s40123-023-00809-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-023-00809-7