Abstract
Introduction
Foveal eversion (FE) is a recently described optical coherence tomography (OCT) finding associated with negative outcome in diabetic macular edema. The main goal of the present study was to investigate the role of the FE metric in the diagnostic workup of retinal vein occlusion (RVO).
Methods
This study was a retrospective, observational case series. We included 168 eyes (168 patients) affected by central RVO (CRVO) and 116 eyes (116 patients) affected by branch (RVO). We collected clinical and imaging data from CRVO and BRVO eyes affected by macular edema with a minimum follow-up of 12 months. On structural OCT, we classified FE as pattern 1a, characterized by thick vertical intraretinal columns, pattern 1b, presenting thin vertical intraretinal lines, and pattern 2, showing no signs of vertical lines in the context of the cystoid macular edema. For statistical purposes, we considered data collected at baseline, after 1 year and at the last follow-up.
Results
The mean follow-up was 40 ± 25 months for CRVO eyes and 36 ± 24 months for BRVO eyes. We found FE in 64 of 168 CRVO eyes (38%) and in 25 of 116 BRVO eyes (22%). Most of the eyes developed FE during the follow-up. For CRVO eyes, we found 6 eyes (9%) with pattern 1a, 17 eyes (26%) with pattern 1b and 41 eyes (65%) with pattern 2. Of those BRVO eyes with FE, we found 8 eyes (32%) with pattern 1a + 1b and 17 eyes (68%) with pattern 2. In both CRVO and BRVO the presence of FE was significantly associated with higher persistence of macular edema and worse outcome, with FE pattern 2 representing the most severe condition. Remarkably, FE patterns 1a and 1b were characterized by BCVA stability over the follow-up, whereas FE pattern 2 showed significant bestcorrected visual acuity (BCVA) worsening at the end of the follow-up.
Conclusions
FE can be considered a negative prognostic biomarker in RVO, associated with higher persistence of macular edema and worse visual outcome. Müller cell impairment might represent the pathogenic mechanism leading to the loss of macular structural support and impairment of fluid homeostasis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Foveal eversion (FE) has been recently described as a structural optical coherence tomography (OCT) parameter associated with high prevalence of macular edema and poor outcome in diabetic retinopathy. |
The main hypothesis of this study is that FE might be applied also to macular edema secondary to central and branch retinal vein occlusion (CRVO and BRVO, respectively). |
What was learned from the study? |
The presence of FE has been associated with worse clinical course and outcome compared with eyes without FE in both CRVO and BRVO eyes. |
We described three different patterns of FE, categorizing three clinically different RVO subgroups. Our findings support the role of FE as a clinically relevant and easily assessable metric to be included in the diagnostic workup of RVO. |
Introduction
Retinal vein occlusion (RVO) represents the second most common cause of retinal vascular diseases after diabetic retinopathy and a major cause of vision deterioration in developed countries [1,2,3]. A common complication of both central RVO (CRVO) and branch RVO (BRVO) is macular edema, leading to reduction of visual acuity. Macular edema is successfully managed by anti-vascular endothelial growth factor (anti-VEGF) injections and corticosteroid implants [4,5,6,7,8,9,10,11], providing fundamental tools for inducing the resolution of edema and preserving visual function [12, 13]. The presence of ischemia (i-RVO) worsens the clinical picture of CRVO and BRVO, and laser treatment may be considered an additional procedure [14,15,16,17]. However, long-term studies showed how heterogeneous the response to treatments and visual outcome may be [18, 19]. Similarly to what happens in diabetic retinopathy, a challenging and unpredictable condition is the presence of persistent macular edema, remarkably affecting the morpho-functional outcome. In a recent paper, we proposed foveal eversion (FE) as a structural optical coherence tomography (OCT) biomarker associated with high prevalence of macular edema and poor outcome in diabetic retinopathy [20]. Furthermore, the identification of more patterns of FE further improves the clinically meaningful categorization of diabetic patients [21], supporting the role of FE as a feasible and useful biomarker to be used in clinical practice.
Our main hypothesis is that FE might also be applied to macular edema secondary to CRVO and BRVO. Hence, the main aim of the present study was to investigate the role of FE in the RVO clinical setting, assessing the relationship to persistent macular edema and visual outcome.
Methods
The study was designed as a retrospective, observational case series. Patients affected by CRVO and BRVO were analyzed at the Department of Ophthalmology, IRCCS San Raffaele Scientific Institute, Milan, Italy. The study was approved by the Ethics Committee of San Raffaele Scientific Institute, Milan, Italy (protocol ID: MIRD), and conducted in compliance with Ethics Guidelines and in accordance with the Declaration of Helsinki. No identifiable data were used, and all patients provided informed consent. The diagnosis of CRVO or BRVO was made by structural OCT and fluorescein angiography examinations.
The inclusion criterion was the diagnosis of CRVO or BRVO complicated by a clinically significant macular edema, treated by anti-VEGF and/or corticosteroids, with a minimum follow-up of 12 months. Exclusion criteria were: high media opacities, other eye diseases potentially affecting the interpretation of the present findings, uncontrolled arterial hypertension or diabetes mellitus, and any ophthalmic surgery in the 6 months before the diagnosis of RVO. Furthermore, we excluded those eyes affected by combined RVO and retinal artery occlusion and eyes characterized by extensive involvement of the posterior pole with severe disruption of retinal structures and baseline visual acuity < + 1.0 LogMAR.
The collected data included LogMAR best corrected visual acuity (BCVA) evaluated by standard ETDRS charts, anterior and posterior segment slit-lamp evaluation and Goldmann applanation tonometry. Structural OCT examination (Spectralis HRA2 + OCT, Heidelberg Engineering, Heidelberg, Germany) was performed at each follow-up visit, with radial, raster and dense scans (ART > 25; enhanced depth imaging).
Structural OCT scans were used to extract central macular thickness (CMT), considering the central ETDRS subfield; fluorescein angiography was revised to assess the presence of peripheral capillary non-perfusion, intended as at least ten-disc areas that lacked fluorescein-filled capillaries.
Moreover, based on structural OCT images, we classified RVO eyes in two subgroups, namely with or without FE. FE was defined as the complete eversion of the foveal profile, as detected on a horizontal, foveal-centered OCT scan. We assessed the presence of FE at baseline or its occurrence during the follow-up. Furthermore, we classified FE eyes in three further subgroups or FE patterns: pattern 1a is defined as the presence of FE with intraretinal vertical columns developed in the context of the hyporeflective cystic space; pattern 1b is defined as the presence of FE with multiple intraretinal fan-like, vertical lines developed in the context of the hyporeflective cystic space; pattern 2 is defined as the presence of FE with only hyporeflective intraretinal cystic signal and no signs of hyperreflective vertical lines. To standardize the differentiation of pattern 1a and pattern 1b, we established FE pattern 1a as the presence of a major central column of at least 100 µm with the possible presence of thinner lines. The other cases were considered FE pattern 1b (Fig. 1). Eyes with FE were categorized accordingly with the first appearance of FE subtype (namely pattern 1a, 1b or 2).
Foveal eversion (FE) patterns in retinal vein occlusion. Starting from the definition of FE as a complete eversion of the foveal profile, FE pattern 1a (A) is characterized by the presence of thick intraretinal vertical columns, with at least one column with a thickness > 100 µm. FE pattern 1b (B) shows thinner intraretinal vertical columns than pattern 1a, whereas FE pattern 2 (C) has no sign of columns in the context of intraretinal macular edema. RVO eyes with macular edema, showing a sign of foveal depression, are classified as no FE eyes (D). RVO retinal vein occlusion
All the eyes were treated using a loading dose of 3-monthly anti-VEGF injections following a treat-and-extend treatment regimen. Criteria for treatment switching to another anti-VEGF molecule of corticosteroid implant included BCVA deterioration > 1 ETDRS line and/or OCT-based evidence of CMT reduction < 25% after treatments, established by ophthalmologist discretion.
Furthermore, persistent macular edema was defined as the persistence of intraretinal fluid for > 6 months, whereas resolved macular edema was defined as complete resolution with recovery of the foveal depression for > 6 months. All the other cases were considered recurrent macular edema.
The main outcome measure was the assessment of the relationship between FE and the clinical course of RVO, considering macular edema persistence, recurrence or resolution, and the visual outcome. The secondary outcome was the assessment of the relationship between each FE pattern (1a, 1b and 2) and both visual outcome and the presence of persistent macular edema. We considered the parameters measured at baseline after 1 year and at the last follow-up visit. Two independent blinded graders performed all the measurements (AA, AR). Interclass correlation coefficient was measured to assess the agreement between the two graders through a two-way random-effects model. For the statistical analyses we included the following fixed variables: age, gender, systemic arterial hypertension, and type and duration of diabetes mellitus. Additional variables were type and number of treatments (anti-VEGF, corticosteroids) and baseline features (BCVA, CMT, i-RVO). All the statistical analyses were performed using the SPSS software package (SPSS, Chicago, IL, USA). In our statistical models, we evaluated the normality distribution of each variable with frequency histograms and quantile-quantile plots. Descriptive statistics of continuous variables were reported as mean ± standard deviation, whereas frequency and proportions were described as categorical variables. Continuous variables were statistically evaluated using the two-tailed t-test. One-way ANOVA analysis assessed the differences between FE eyes and eyes without FE. Tau-Kendall correlation analysis was adopted to assess the relationship between the collected parameters. Statistical significance was set at p < 0.05.
Results
Overall Data
We collected data from 168 CRVO eyes of 168 patients [112 males (67%); mean age 67 ± 15 years] and 116 BRVO eyes of 116 patients [56 males (48%); mean age 71 ± 11 years]. The mean follow-up was 40 ± 25 months for CRVO eyes and 36 ± 24 months for BRVO eyes. Baseline BCVA was similar to the end of follow-up (from 0.6 ± 0.4 LogMAR to 0.6 ± 0.5 LogMAR in CRVO and from 0.4 ± 0.3 LogMAR to 0.4 ± 0.4 LogMAR in BRVO; p > 0.05).
Both CRVO and BRVO underwent significant CMT improvement (from 560 ± 226 to 340 ± 186 µm in CRVO and from 503 ± 170 to 308 ± 116 μm in BRVO; p < 0.01). CRVO eyes received a mean of 9 ± 8 intravitreal treatments, whereas BRVO underwent 6 ± 6 injections over the follow-up. The percentage of FE in CRVO eyes was 64 out of 168 eyes (38%) and 25 out of 116 eyes (22%) in BRVO eyes. Furthermore, 11/64 CRVO eyes (17%) and 2/25 BRVO eyes (8%) showed FE at baseline, whereas the remaining eyes developed FE during the follow-up, with a mean onset of 11 ± 6 months for CRVO and 9 ± 5 months for BRVO (p < 0.05). Our multivariate linear model revealed i-RVO as significantly associated with the onset of FE in both diseases (F = 10.22; p = 0.002 for CRVO and F = 9.45; p = 0.003 for BRVO). However, FE onset was not influenced by age or gender (p > 0.05). Moreover, the presence of FE had no influence on baseline CMT (F = 1.73; p = 0.195 for CRVO and F = 1.12; p = 0.243 for BRVO). In addition, the systemic status of the patients showed no significant effect on RVO course and clinical outcome (p > 0.05).
CRVO
Sixty-four out of 168 CRVO eyes (38%) showed FE. Eyes with and without FE did not differ in terms of age and gender (p > 0.05). The mean follow-up was 48 ± 25 months for FE eyes and 34 ± 23 months for eyes without FE. The mean number of intravitreal injections required was significantly higher for FE eyes (12 ± 8) than for eyes without FE (6 ± 7) (p < 0.01) (Supplementary Material Table 1). The percentage of i-RVO and laser treatment was similar between the two groups (p > 0.05) as was the percentage of eyes that underwent cataract surgery (p > 0.05). The mean baseline LogMAR BCVA was similar to 12-month follow-up (p > 0.05), while the last LogMAR BCVA showed a significant worsening in eyes with FE (p < 0.01). The mean CMT was significantly higher in eyes with FE at baseline, after 12 months and at last follow-up (p < 0.01).
Among those 64 CRVO eyes with FE, we found 6 (9%) eyes with pattern 1a, 17 (26%) eyes with pattern 1b and 41 (65%) with pattern 2. Remarkably, the percentage of i-RVO was higher in eyes with pattern 2 (41%) compared with both pattern 1a and pattern 1b (p < 0.01). Considering pattern 1a + 1b vs. pattern 2, we found significantly worse BCVA in pattern 2 at the last follow-up (0.6 ± 0.5 LogMAR vs. 0.8 ± 0.3 LogMAR; p < 0.01). There were no other significant differences among the three groups (p > 0.05) (Supplementary Material Table 2).
Analyzing the changes of macular edema over the follow-up in eyes with FE (persistence, recurrence or resolution of macular edema), 29 eyes of 64 (45%) showed persistent macular edema, 16 eyes (25%) had recurrent macular edema, and 19 eyes (30%) showed resolved macular edema.
In more detail, FE pattern 1a presented resolved macular edema in 50% of cases (3/9 eyes), recurrent macular edema in 34% of cases (2/9 eyes) and persistent macular edema in 16% of cases (1/9 eye).
FE pattern 1b was characterized by resolved macular edema in 48% of cases (8/17 eyes), recurrent macular edema in 29% of cases (5/17 eyes) and persistent macular edema in 23% of cases (4/17 eyes).
FE pattern 2 showed resolved macular edema in 19% of cases (8/41 eyes), recurrent macular edema in 22% of cases (9/41 eyes) and persistent macular edema in 59% of cases (24/41 eyes). These eyes were also characterized by a significantly higher percentage of i-RVO (41% of cases) compared with both pattern 1a (20% of cases) and pattern 1b (13% of cases) (p < 0.01).
Eyes with persistent macular edema were characterized by significantly worse LogMAR BCVA at baseline, after 12 months and at the last follow-up (all p < 0.01). There was no difference between eyes with persistent macular edema and eyes with a recurrent or resolved macular edema regarding baseline CMT and 12-month CMT (both p > 0.05), while it was significantly higher in the persistent macular edema subgroup at the last follow-up (p > 0.01). Eyes affected by recurrent macular edema underwent more intravitreal injections (15 ± 8) than eyes with persistent or resolved macular edema (overall 10 ± 7) (p < 0.01). In addition, patients characterized by resolved macular edema were significantly younger (64 ± 13 years) than patients with persistent or recurrent macular edema (overall 73 ± 10 years) (p < 0.01). Eyes with resolved macular edema were characterized by better BCVA after 12 months and at last follow-up (both p < 0.01) regarding the other two subgroups and significantly lower CMT at last follow-up (p < 0.01).
Conversely, considering the course of macular edema in eyes without FE (Fig. 2) (persistence, recurrence or resolution of macular edema), 9 of 104 eyes (8%) showed persistent macular edema, 30 (29%) eyes had recurrent macular edema, and 65 eyes (63%) had resolved macular edema (p < 0.01).
A case of CRVO without FE. Baseline structural OCT (A) shows the combined presence of intraretinal and subretinal fluid (LogMAR BCVA 0.5). After the loading dose of anti-VEGF injections, the regression of intraretinal edema is seen, with persistence of subretinal fluid (B). After 6 months of treatment, also subretinal fluid was almost reabsorbed (C). One- and 2-year follow-ups confirm the positive effect of the treat-and-extend regimen in preserving retinal integrity, with final LogMAR BCVA of 0.0 (D, E). CRVO central retinal vein occlusion, FE foveal eversion, OCT optical coherence tomography, BCVA best corrected visual acuity, anti-VEGF anti-vascular endothelial growth factor
The correlation analysis confirmed the relationship of persistent macular edema with worse LogMAR BCVA and CMT (Tau-Kendall coefficient 0.48 and 0.52, respectively; both p < 0.01) and both with the presence of FE and FE pattern 2 (Tau-Kendall coefficient 0.53 and 0.65; both p < 0.01). Moreover, worse LogMAR BCVA after 12 months was correlated with i-RVO (Tau-Kendall coefficient 0.42; p < 0.01).
BRVO
Twenty-five out of 116 BRVO eyes (22%) showed FE. Eyes with and without FE showed no significant difference in terms of age and gender (p > 0.05). The mean number of intravitreal injections required from BRVO eyes with FE was higher (10 ± 9) than in eyes without FE (5 ± 5) (p < 0.01). The percentage of i-RVO and laser treatment was similar between the two subgroups (p > 0.05) as was the percentage of eyes that underwent cataract surgery (p > 0.05). The mean LogMAR BCVA was significantly higher in eyes with FE at baseline and after 12-month follow-up regarding eyes without FE (both p < 0.01). The mean CMT was significantly higher in eyes with FE at baseline, after 12 months and at the last follow-up (all p < 0.01) (Supplementary Material Table 3).
Of those 25 BRVO eyes with FE, we found 8 (32%) eyes with pattern 1a + 1b and most of the eyes (17; 68%) with pattern 2 (Supplementary Material Table 4).
Because of the low number of BRVO eyes with pattern 1a and 1b, we performed the statistical analysis merging both subgroups (pattern 1a + 1b vs. pattern 2). BRVO eyes with FE pattern 1a + 1b showed significantly better LogMAR BCVA at 12 months and at the end of the follow-up compared with FE pattern 2 eyes (p < 0.05). Moreover, BRVO eyes with FE pattern 1a + 1b showed a significantly lower percentage of i-RVO than FE pattern 2 eyes (p < 0.05). No other significant differences characterized the two subgroups of BRVO FE eyes.
FE pattern 1a + 1b (Fig. 3) showed resolved macular edema in 50% of cases (4/8 eyes), recurrent macular edema in 25% of cases (2/8 eyes) and persistent macular edema in 25% of cases (2/8 eyes).
A case of BRVO with FE pattern 1b. Baseline structural OCT (A) shows the presence of a completely everted foveal profile with multiple thin intraretinal vertical columns (LogMAR BCVA 0.8). Macular edema was already reabsorbed after the loading dose of anti-VEGF injections (B), and 6-month, 1-year and 2-year follow-ups confirmed the stability of the clinical picture and the positive outcome with a final LogMAR BCVA of 0.2 (C–E). BRVO branch retinal vein occlusion, FE foveal eversion, OCT optical coherence tomography, BCVA best corrected visual acuity, anti-VEGF anti-vascular endothelial growth factor
FE pattern 2 (Fig. 4) was characterized by resolved macular edema in 23.5% of cases (4/17 eyes), recurrent macular edema in 23.5% of cases (4/17 eyes) and persistent macular edema in 53% of cases (9/17 eyes).
A case of BRVO with FE pattern 2. Baseline structural OCT (A) shows the presence of a completely everted foveal profile without central vertical columns (LogMAR BCVA 0.8). Despite the intensive anti-VEGF treatment regimen and switching to corticosteroid implants during the follow-up, this eye was always characterized by macular edema persistence over the entire follow-up window [after loading dose (B); 6-month follow-up (C); 1-year follow-up (D); 2-year follow-up (E)]. Final LogMAR BCVA was 0.5. BRVO branch retinal vein occlusion, FE foveal eversion, OCT optical coherence tomography, BCVA best corrected visual acuity, anti-VEGF anti-vascular endothelial growth factor
Eyes with recurrent macular edema underwent significantly more intravitreal injections than those in the other two subgroups (19 ± 11 vs. 7 ± 4; p < 0.01). Eyes with persistent macular edema showed the worst LogMAR BCVA and CMT at the last follow-up (both p < 0.01).
However, considering the course of macular edema in eyes without FE, 7 of 91 eyes (8%) showed persistent macular edema, 28 (31%) eyes had recurrent macular edema, and 56 eyes (61%) had resolved macular edema (p < 0.01).
The correlation analysis confirmed the negative relationship between last follow-up LogMAR BCVA and the presence of FE (Tau-Kendall coefficient − 0.55; p < 0.01) as well as persistent macular edema (Tau-Kendall coefficient − 0.48; p < 0.01).
The distribution of persistent, recurrent or resolved macular edema among CRVO and BRVO eyes is given in Supplementary Material Table 5. In addition, Fig. 5 shows the proposed mechanism of formation of FE and its evolution.
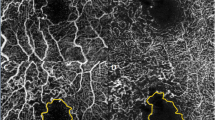
The possible evolution of foveal eversion in RVO. Baseline image shows a BRVO complicated by macular edema with complete eversion of the foveal profile and multiple thin vertical columns, classified as FE pattern 1b (A). After 6 months (B), we can observe a dry retina with the presence of a central vertical hyperreflective line, which can be interpreted as a gliotic reaction of the Müller cells. Nine-month follow-up (C) examination shows the recurrence of macular edema, with a marked thinning of the vertical intraretinal columns and degenerative signs of inner retinal layers, which are further evident at 1-year follow-up (D). Eighteen-month follow-up (E) is characterized by almost complete response to intravitreal treatments, although it is possible to observe the central disruption of retinal layers. Thirty-month follow-up (F) is characterized by recurrent behavior of macular edema. Interestingly, at 40-month follow-up (G), it is possible to observe the presence of a mixed reflectivity material in the context of the intraretinal macular edema, highlighting the passage through FE pattern 2. From this point, macular edema assumes a persistent course, as confirmed by 5-year follow-up examination (H). BRVO branch retinal vein occlusion, FE foveal eversion
Discussion
In the present study we assessed the diagnostic role of FE in the clinical setting of CRVO and BRVO. The presence of FE was associated with worse clinical course and outcome compared with eyes without FE. CRVO and BRVO eyes may disclose three different patterns of FE. The clinical course of FE pattern 1a and FE pattern 1b was overall worse than in eyes without FE, although these patients showed similar BCVA at the end of the follow-up. Conversely, for CRVO and BRVO eyes, FE pattern 2 subgroup was characterized by remarkably high prevalence of persistent macular edema (> 50% of cases) and significantly worse visual outcome than all the other RVO eyes. FE characterized the minority of CRVO and BRVO eyes at baseline, whereas it may occur over the follow-up. In addition, the presence of peripheral capillary non-perfusion was slightly associated with worse clinical outcome and with the onset of FE.
Our data confirmed the fact that the number of intravitreal treatments may be associated with visual function stability, but not a significant improvement [18, 19]. Furthermore, we found no significant results related to laser treatments, further confirming its minor role in the management of RVO.
The most interesting result of the present study regards the perspective of making a new RVO classification based on the presence and type of FE. FE has been previously interpreted as a structural OCT sign of Müller cell impairment [20, 21]. Müller cells are responsible for the entire functional and structural homeostasis of the human retina, playing a major role in the intra-extracellular fluid balance and structural integrity of the foveal region [22, 23]. Although Müller cells are known to play a major role in the pathogenesis of diabetic retinopathy and diabetic macular edema [23,24,25], in this study we hypothesized their potential role also in the pathogenesis and clinical course of macular edema secondary to RVO. Although representing a relatively novel research field, some support for our hypothesis can already be found in the literature. Indeed, a previous study highlighted how the assessment of macular edema features, including the extension and distribution of cysts, is clinically relevant for collecting information about RVO outcome [26]. Mouse models of BRVO highlighted the importance of Müller cells in governing the reabsorption of intraretinal fluid [27]. Müller cells showed a rearrangement of genetic expression after BRVO, with downregulation of key anti-edema factors such as Kir4.1 and aquaporins, osmotic swelling of Müller cells and their damage [28]. A likely mechanism leading to the damage of Müller cells is the hypoxic status induced by vascular stasis and capillary closure characterizing both CRVO and BRVO [29]. As a consequence of Müller cells impairment, it might be possible to observe upregulation of permeability and pro-edema factors and the loss of intraretinal fluid homeostasis [29, 30]. In this scenario, we might assume that the greater the vascular stasis and hypoxia are, the higher the probability to observe Müller cell damage and, as an indirect structural OCT sign, the onset of FE and its patterns. Our pathogenic hypothesis regarding the progression of FE patterns and the central role of Müller cells is shown in Fig. 5, where we used a case of BRVO with 5-year follow-up, showing the early sign of Müller cell gliosis following a progressive worsening of retinal morphology and evolution toward FE pattern 2. This should be considered only a humble attempt to visually represent our pathogenic hypothesis. The timing and all the microstructural considerations should be carefully evaluated since this is not supported by big data. Further studies involving more eyes and providing histological support are warranted to establish the pathogenesis of FE and involvement of Müller cells.
We are aware our study is potentially affected by several limitations, first of all related to the retrospective design of this investigation. This study setting made the assessment of FE progression toward different patterns impossible. Indeed, the retrospective nature of the present investigation carried a tangible risk of losing useful information to assess the evolution of FE over the follow-up. For this reason, further prospective studies are warranted to reliably define the evolution and progression of FE patterns over time. Since our study was mainly focused on the assessment of the intraretinal status in RVO, we did not perform specific assessments of outer retinal status, including the clinical impact of subretinal fluid. We are aware this represents an important biomarker in RVO [26]; however, we may assume a completely different pathogenesis as well as different retinal cytotypes involved regarding intraretinal fluid and FE. However, we believe that the clinical interaction among subretinal fluid, intraretinal fluid and FE should be investigated in the future. Moreover, the real-life setting of the study, with no standardized decisional process regarding the treatment strategy, and the variable follow-up remarkably affected the possibility to explore the effect of treatments, considering both intravitreal molecules and laser, on the onset and course of macular edema and FE. However, a strong point of the present study is the collection of data from a large cohort of eyes affected by CRVO and BRVO. Moreover, although all imaging-based approaches are potentially affected by artifacts [31], in this case their influence is poor because of the dichotomic nature of FE (present/absent) and the high feasibility of this kind of investigation. Furthermore, all our hypotheses represent mere speculations, making the present study a first exploratory investigation. Further prospective studies are warranted to draw definite conclusions regarding the role of FE evaluation in clinical practice.
Conclusions
Our study highlighted how FE, detected on structural OCT, can categorize more subtypes of CRVO and BRVO, characterized by different morphologies and functional outcomes. From the perspective of customized treatment strategies and the adoption of artificial intelligence-based diagnostic approaches, FE might represent a useful metric to be included in the diagnostic workup of RVO.
References
Hayreh SS, Zimmerman MB, Podhajsky P. Incidence of various types of retinal vein occlusion and their recurrence and demographic characteristics. Am J Ophthalmol. 1994;117(4):429–41.
Rogers S, et al. The prevalence of retinal vein occlusion: pooled data from population studies from the United States, Europe, Asia, and Australia. Ophthalmology. 2010;117(2):313-9.e1.
Hayreh SS. Ocular vascular occlusive disorders: natural history of visual outcome. Prog Retin Eye Res. 2014;41:1–25.
Campochiaro PA, et al. Sustained benefits from ranibizumab for macular edema following central retinal vein occlusion: twelve-month outcomes of a phase III study. Ophthalmology. 2011;118(10):2041–9.
Haller JA, et al. Randomized, sham-controlled trial of dexamethasone intravitreal implant in patients with macular edema due to retinal vein occlusion. Ophthalmology. 2010;117(6):1134-1146.e3.
Haller JA, et al. Dexamethasone intravitreal implant in patients with macular edema related to branch or central retinal vein occlusion twelve-month study results. Ophthalmology. 2011;118(12):2453–60.
Heier JS, et al. Ranibizumab for macular edema due to retinal vein occlusions: long-term follow-up in the HORIZON trial. Ophthalmology. 2012;119(4):802–9.
Campochiaro PA, et al. Long-term outcomes in patients with retinal vein occlusion treated with ranibizumab: the RETAIN study. Ophthalmology. 2014;121(1):209–19.
Boyer D, et al. Vascular endothelial growth factor Trap-Eye for macular edema secondary to central retinal vein occlusion: six-month results of the phase 3 COPERNICUS study. Ophthalmology. 2012;119(5):1024–32.
Heier JS, et al. Intravitreal aflibercept injection for macular edema due to central retinal vein occlusion: two-year results from the COPERNICUS study. Ophthalmology. 2014;121(7):1414-1420.e1.
Clark WL, et al. Intravitreal aflibercept for macular edema following branch retinal vein occlusion: 52-week results of the VIBRANT study. Ophthalmology. 2016;123(2):330–6.
Schmidt-Erfurth U, et al. Guidelines for the management of retinal vein occlusion by the European Society of Retina Specialists (EURETINA). Ophthalmologica. 2019;242(3):123–62.
Arrigo A, Bandello F. Retinal vein occlusion: drug targets and therapeutic implications. Expert Opin Ther Targets. 2021;25(10):847–64.
Tadayoni R, et al. Sustained benefits of ranibizumab with or without laser in branch retinal vein occlusion: 24-month results of the BRIGHTER study. Ophthalmology. 2017;124(12):1778–87.
Chatziralli I, Theodossiadis G, Parikakis E, Mitropoulos PG, Theodossiadis P. Long-term anatomical and functional outcomes in patients with ischemic central retinal vein occlusion treated with anti-vascular endothelial growth factor agents. Ophthalmic Res. 2017;58(4):203–8.
Khayat M, Williams M, Lois N. Ischemic retinal vein occlusion: characterizing the more severe spectrum of retinal vein occlusion. Surv Ophthalmol. 2018;63(6):816–50.
Hayreh SS. Photocoagulation for retinal vein occlusion. Prog Retin Eye Res. 2021;85: 100964.
Rezar S, et al. Anti-VEGF treatment in branch retinal vein occlusion: a real-world experience over 4 years. Acta Ophthalmol. 2015;93(8):719–25.
Arrigo A, et al. Real-life management of central and branch retinal vein occlusion: a seven-year follow-up study. Thromb Haemost. 2021;121(10):1361–6.
Arrigo A, et al. Foveal eversion: a possible biomarker of persistent diabetic macular edema. Ophthalmol Ther. 2021;10(1):115–26.
Arrigo A, et al. Foveal eversion patterns in diabetic macular edema. Sci Rep. 2022;12(1):13097.
Distler C, Dreher Z. Glia cells of the monkey retina—II. Müller cells. Vis Res. 1996;36(16):2381–94.
Reichenbach A, Bringmann A. Glia of the human retina. Glia. 2020;68(4):768–96.
Coughlin BA, Feenstra DJ, Mohr S. Müller cells and diabetic retinopathy. Vis Res. 2017;139:93–100.
Chakravarthy U, et al. Clinical evidence of the multifactorial nature of diabetic macular edema. Retina. 2018;38(2):343–51.
Martinet V, et al. Macular edema in central retinal vein occlusion: correlation between optical coherence tomography, angiography and visual acuity. Int Ophthalmol. 2012;32(4):369–77.
Köferl P, et al. Effects of arteriolar constriction on retinal gene expression and Müller cell responses in a rat model of branch retinal vein occlusion. Graefes Arch Clin Exp Ophthalmol. 2014;252(2):257–65.
Rehak M, et al. Retinal gene expression and Müller cell responses after branch retinal vein occlusion in the rat. Investig Ophthalmol Vis Sci. 2009;50(5):2359–67.
Bek T. Capillary closure secondary to retinal vein occlusion. A morphological, histopathological, and immunohistochemical study. Acta Ophthalmol Scand. 1998;76(6):643–8.
Xin X, et al. Hypoxic retinal Muller cells promote vascular permeability by HIF-1-dependent up-regulation of angiopoietin-like 4. Proc Natl Acad Sci USA. 2013;110(36):E3425–34.
Arrigo A, Aragona E, BattagliaParodi M, Bandello F. Quantitative approaches in multimodal fundus imaging: state of the art and future perspectives. Prog Retin Eye Res. 2023;92: 101111.
Acknowledgements
Funding
No funding or sponsorship was received for this study or publication of this article.
Author Contributions
Study design and manuscript drafting (Alessandro Arrigo MD,PhD, Emanuela Aragona MD,PhD); data collection and analysis (Alessio Antropoli MD, Lorenzo Bianco MD, Andrea Rosolia MD, Andrea Saladino MD); critical revision of the manuscript, supervision of the entire study (Francesco Bandello MD,FEBO, Maurizio Battaglia Parodi MD).
Disclosures
Francesco Bandello has consulted for: Alcon (Fort Worth, TX, USA), Alimera Sciences (Alpharetta, GA, USA), Allergan Inc (Irvine, CA, USA), Farmila-Thea (Clermont-Ferrand, France), Bayer Shering-Pharma (Berlin, Germany), Bausch And Lomb (Rochester, NY, USA), Genentech (San Francisco, CA, USA), Hoffmann-La-Roche (Basel, Switzerland), NovagaliPharma (Évry, France), Novartis (Basel, Switzerland), Sanofi-Aventis (Paris, France), Thrombogenics (Heverlee, Belgium), Zeiss (Dublin, USA). Alessandro Arrigo, Emanuela Aragona, Alessio Antropoli, Lorenzo Bianco, Andrea Rosolia, Andrea Saladino and Maurizio Battaglia Parodi have nothing to disclose.
Compliance with Ethics Guidelines
The study was approved by the Ethical Committee of San Raffaele Scientific Institute, Milan, Italy (protocol ID: MIRD) and conducted in compliance with Ethics Guidelines and in accordance with the Declaration of Helsinki. No identifiable data were used, and all patients provided informed consent.
Data Availability
The datasets generated during and/or analyzed during the current study are not publicly available due to internal rules and privacy issues.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Arrigo, A., Aragona, E., Antropoli, A. et al. Foveal Eversion is Associated with High Persistence of Macular Edema and Visual Acuity Deterioration in Retinal Vein Occlusion. Ophthalmol Ther 12, 2157–2169 (2023). https://doi.org/10.1007/s40123-023-00734-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-023-00734-9