Abstract
Increasing evidence indicates that improving ocular blood flow (OBF) can be a therapeutic direction for glaucoma therapy. Tafluprost, a prostaglandin analogue which lowers the intraocular pressure (IOP), has been shown to improve OBF in animals and humans. Several animal experiments showed that topical tafluprost significantly increased optic nerve head and retinal blood flow. Clinical trials also showed a beneficial effect of tafluprost on optic nerve head and macula blood flow, and a good ocular pulse amplitude-lowering effect. But, there are still a few conflicting results. Overall, tafluprost seems to have a beneficial effect on OBF, and the positive effect is probably independent from its IOP-lowering effect, which also is expected to improve OBF. Moreover, reducing the intracellular free Ca2+ concentration may be a possible mechanism of tafluprost’s effect on OBF. More well-designed studies are required to reveal the truth.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
An increasing amount of evidence indicates that improving ocular blood flow can be a therapeutic direction for glaucoma therapy. |
Tafluprost seems to have a beneficial effect on ocular blood flow, and the positive effect is probably independent from its intraocular pressure-lowering effect, which also is expected to improve ocular blood flow. |
Reducing the intracellular free Ca2+ concentration may be a possible mechanism of tafluprost’s effect on eye blood flow. |
Introduction
Glaucoma is characterized by optic nerve damage and progressive visual field defect [1]. It is estimated that 112 million people worldwide will suffer from glaucoma by 2040 [2]. Furthermore, glaucoma is the main cause of irreversible blindness [3], and elevated intraocular pressure (IOP) is considered to be the most important risk factor for glaucoma. Thus, reducing IOP is recognized as the main treatment for glaucoma [4]. Currently, IOP-lowering efficacy is the main index for evaluating the clinical efficacy of antiglaucoma medications. However, some patients with satisfactory IOP control with IOP-lowering medications continue to have worsening visual field defect. Moreover, although IOP-reduction therapy cannot reduce IOP significantly in patients with normal-tension glaucoma (NTG), it can still delay the progression of glaucomatous optic neuropathy [5, 6]. As can be seen, the mechanism of action of antiglaucoma medications is complex, and the therapeutic focus needs to be shifted beyond the IOP-lowering effect.
Studies have shown that parameters including blood flow density, blood flow index, and vessel density (VD) in the optic nerve head (ONH), peripapillary vascular layer, and macula decrease significantly in patients with glaucoma [7,8,9,10,11,12,13,14]. Furthermore, the decreased ocular blood flow (OBF) is closely related to the occurrence and development of glaucomatous optic neuropathy. A lower baseline of VD in the macula and the peripapillary area was associated with a faster rate of progressive retinal nerve fiber layer (RNFL) loss in patients with mild-to-moderate primary open-angle glaucoma (POAG) [15]. Kwon et al. [16] reported faster thinning of RNFL in eyes with more deep-layer microvasculature dropout than in those without the dropout. Jia et al. [17] found that the ONH blood flow decreased significantly in patients with glaucoma, whereas the abnormal blood flow index was highly correlated with visual field defect. Yarmohammadi et al. [13] reported that changes in the macular area’s superficial plexus blood flow density were related to the visual field defect. Additionally, a significant correlation was observed between decreased vascular density and the severity of visual field defect. Furthermore, several other studies have reported different degrees of atrophy and blood flow reduction of the capillary network in the peripapillary areas of patients with glaucoma compared with healthy subjects. The location of abnormal changes and the degree of blood flow reduction in the capillary network correlated with the location and degree of visual field defect in glaucoma [12, 17, 18]. Some scholars have also proposed that vascular density parameters were reliable in diagnosing early glaucoma [14]. This collective evidence indicates that the abnormal OBF is an important pathological change in glaucoma. Therefore, improving OBF can be one of the targeted therapeutic avenues for glaucoma. Moreover, the effect of IOP-lowering medications on OBF requires much-needed attention.
Prostaglandin analogues (PGAs) are the first-line therapy for glaucoma treatment. Several studies have shown that local administration of PGAs produces vasodilatation effects in improving OBF, similar to endogenous prostaglandins [19]. Currently, PGAs, including latanoprost, travoprost, tafluprost [20], etc., are widely used in the clinic. Tafluprost topical ophthalmic solution was launched onto the market in Japan in 2008. The key structural feature of tafluprost is the presence of two fluorine atoms in place of a hydrogen atom and hydroxyl group at carbon-15 of the traditional prostaglandin core. This modification in structure led to significantly improved affinity (12 times better than latanoprost [21,22,23]) for prostaglandin F2α receptor (also known as FP receptor). In addition, the minimum effective concentration and incidence of local complications were significantly reduced [24,25,26,27]. The 0.0015% tafluprost has a favorable IOP-lowering effect compared to 0.005% latanoprost and 0.004% travoprost [28]. Moreover, it demonstrates an advantage in improving OBF compared with several other PGAs.
This study reviewed the effect of tafluprost on OBF and explored its possible mechanism. This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors. Three databases, namely PubMed, Embase, and Elsevier, were systematically searched to obtain comprehensive, relevant literature from inception to February 21, 2022. We used a broad, inclusive search strategy to avoid missing a seminal contribution. We used the MeSH term “tafluprost”. Additionally, we manually searched the reference lists for potentially relevant studies, and five additional Japanese articles were included to avoid missing important clinical data. Endnote software was used to filter out duplicate articles manually. Figure 1 shows the literature search and filtering process.
Animal Studies
Non-Primates
Anesthetized State (Cats)
Using a laser Doppler velocity system, Izumi et al. [29] first demonstrated that topical tafluprost significantly increased retinal blood flow (RBF) and blood velocity in normal anesthetized cats. They further pointed out that the main reason for the increase of RBF caused by the single topical administration of tafluprost was the increase of blood flow velocity at the measurement site. However, little change in blood vessel diameter was observed. Therefore, the increased blood flow velocity in the study might reflect the expansion of downstream vessels. In conclusion, the researchers speculated that retinal microvessels located more peripherally than measured points might be dilated. Nevertheless, the study had its shortcomings. Although the structure and circulation of cats’ retinas are similar to those of humans, PGF2 has a stronger effect on cat microvasculature than the primates [30]. In addition, as a result of the difference in the ocular volume, the vascular reaction between cats and humans does not seem to be similar after the instillation of the same amount of drug. Thus, RBF changes in humans may be different or attenuated compared to cats.
Conscious State (Rabbits)
OBF is affected by the depth of anesthesia; thus, its accurate measurement under anesthesia is difficult [31, 32]. Therefore, the researchers chose to assess the OBF in the conscious animal. Akaishi et al. [33] reported significantly increased ONH blood flow through laser speckle flowgraphy (LSFG) in conscious rabbits after continuous use of 0.0015% tafluprost, 0.005% latanoprost, and 0.004% travoprost for 28 days. Still, at all measurement points, the rate of increase in the tafluprost group was significantly higher than in the latanoprost and travoprost groups. This study showed that the repeated administration of tafluprost results in a long-term rather than short-term increase in ONH blood flow in conscious rabbits. Moreover, its potency was greater than the other two PGAs.
To explore the mechanism of PGAs in improving the ONH blood flow, Kurashima et al. [34] studied the effect of four PGAs (tafluprost; 15-OH tafluprost; latanoprost; travoprost) on endothelin-1 (ET-1)-induced ONH blood flow disorders through LSFG in male rabbits. The results showed that the local administration of PGAs inhibited the decrease of ONH blood flow in conscious rabbits induced by ET-1. Furthermore, tafluprost could almost completely inhibit the effect of ET-1. Additionally, the effect was more sustainable than other PGAs, indicating tafluprost was superior to other PGAs in resisting the effects of ET-1.
Giannico et al. [35] divided the conscious, healthy rabbits into six groups. The left eyes were topically treated for 4 weeks with the preservative benzalkonium chloride (BAK) only or different kinds of PGAs (tafluprost BAK-free, bimatoprost BAK, travoprost BAK, travoprost POLYQUAD, and latanoprost BAK), while the fellow eye served as a control. Before and after treatment, color Doppler imaging was used to evaluate the ophthalmic artery (OA). The results showed that tafluprost BAK-free and travoprost with BAK significantly reduced the resistive index of the OA in rabbits, indicating improved OA blood flow. Moreover, preservative-free tafluprost has greater advantages in clinical application owing to the nullification of the adverse effects of preservatives on the ocular surface [36].
Primates
Although cats and rabbits can be used in research studies to explore the effect of tafluprost on OBF, monkeys have a more similar ONH anatomical structure and vascular system to human eyes. The advantages of using primates for research are clear. Additionally, previous studies have evaluated the effect of tafluprost on OBF in normal eyes but not on a glaucomatous eye. Mayama et al. [37] established a monocular glaucoma model in rhesus monkeys. The laser speckle technique detected the ONH blood flow of rhesus monkeys under anesthesia. Single and continuous administrations of 0.0015% tafluprost for 7 days increased the ONH blood flow in the glaucoma model and control eyes. These results suggested that tafluprost could increase the blood flow in subjects with or without glaucoma. The study of the unilateral glaucoma model and contralateral normal eyes in the same subjects excluded the effects of circulation parameters, including blood pressure, pulse rate, autonomic tension, and plasma levels of various vascular active substances between the two eyes. Moreover, this model provides an ideal platform for studying the pharmacological properties of ONH vessels in experimental glaucoma.
Clinical Research
Experimental results in animal models may not be directly extrapolated to humans and thus require further clinical studies. Here we summarize the relevant clinical studies for the following aspects.
ONH Area
LSFG
Several studies used the LSFG method, including normal subjects and patients with NTG, POAG, and myopic disc types. A study of healthy male eyes showed that the microcirculation of the upper and temporal sides of the ONH was significantly increased after continuous administration of 0.0015% tafluprost every night for 7 days [38]. A prospective intervention study of patients with NTG showed similar results [39]. Latanoprost was switched to tafluprost during the treatment of patients with NTG. One month later, LSFG was used to assess changes in ONH blood flow. The results were consistent with the previous study in healthy men, showing significantly increased blood flow of the upper and temporal sides of the ONH without any change in the IOP-lowering effect. In another study, 24 patients with POAG were randomly divided into tafluprost and latanoprost groups [40]. LSFG was used to detect the ONH blood flow after 6 months. The blood flow of the upper, lower, and temporal sides of the ONH in the tafluprost group increased significantly. In contrast, no obvious blood flow changes were detected in the latanoprost group. There was no difference in IOP-lowering effect between the two groups. The results suggest that the positive effect of tafluprost on ONH blood flow is probably independent from its IOP-lowering effect, which also is expected to improve OBF. Notably, these patients were followed up for a longer period. The microcirculation of ONH was stable for up to 3 years in patients treated with tafluprost but decreased in the latanoprost group [41]. Previous studies have shown that myopia is one of the risk factors for POAG [42, 43]. The decreased blood circulation in the ONH might be related to myopia and glaucoma [44]. Researchers began to pay attention to the potential benefit of topical tafluprost on ONH blood flow in people with myopia. In a prospective intervention study conducted on 48 eyes of 24 participants with myopic optic disc morphologic changes (28 were diagnosed as NTG, and 20 were normal subjects) by Tsuda et al. [44], one eye was treated with topical tafluprost, and the fellow eye served as the control. The study design excluded any influence from systemic circulation parameters. LSFG-NAVI (a newer version of LSFG) evaluated the ONH blood flow after 60, 90, and 120 min. The ONH blood supply was significantly increased in all the treated eyes and reached a peak at 120 min. These studies indicated that the treatment of tafluprost had a beneficial effect on OBF in normal subjects, patients with NTG, patients with POAG, and people with a myopic disc. However, no significant changes were observed in LSFG measurements after tafluprost therapy in patients with POAG [45], which was inconsistent with the abovementioned report. Of note, only 11 patients with POAG were included in this study, which may make the results less reliable.
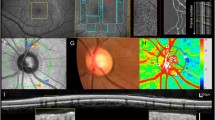
Optical Coherence Tomography Angiography (OCT-A)
Weindler et al. [46] used OCT-A (Topcon DRI OCT Triton) to compare the effect of topical tafluprost or surgical treatment on ONH blood flow density in patients with POAG. The flow density of patients with POAG who underwent IOP-lowering surgery (deep sclerectomy, trabeculotomy, and trabeculectomy) because of poor compliance or intolerance to multiple eye drops was used for comparison. The assessment was made when IOP values reached 10–21 mmHg. Any possibility of interference of flow density reduction caused by decreased IOP was excluded. There was a significantly higher peripapillary flow density in all sectors in tafluprost-treated eyes when compared to post-surgery eyes. Again, the results indicate that the OBF-improving effect of tafluprost is probably independent from its IOP-lowering effect.
A prospective observational study included 36 eyes from 36 patients newly diagnosed with the initial stage of POAG. The patients were treated with tafluprost, tafluprost/timolol combination, or no topical treatment [47]. OCT-A (AngioVue) was performed 1 week after the treatment. The tafluprost and tafluprost/timolol fixed combination decreased VD in the ONH without changing the VD of the peripapillary retina. On the first assessment, the findings were unexpected and inconsistent with previous research. However, the end-diastolic rate of the short posterior ciliary artery in early glaucoma was negatively correlated with VD in the ONH and retinal peripapillary area. In other words, the more blood entering the retina and ONH in early glaucoma, the lower the OCT-A value was. This observation was interpreted as an automatic regulatory mechanism that preserves retinal blood flow in the early stages of the disease [48]. Since the study included patients with early POAG, the autoregulation of OBF might be preserved at the initial stages of glaucoma. Therefore, tafluprost or tafluprost/timolol can be beneficial for OBF in patients with early POAG. However, the regulatory effect may not apply to advanced patients. Moreover, validation of this hypothesis requires long-term follow-up studies at different stages of POAG.
Macular Area
A prospective observational study by Iida et al. [45] included patients with POAG and healthy subjects. The subjects were evaluated using multiple methods (adaptive optics scanning laser ophthalmoscopy (AOSLO), LSFG, and OCT). The study evaluated the effects of topical tafluprost treatment on ocular circulation at baseline and 1, 4, and 12 weeks after initiating treatment in patients with POAG. The mean parafoveal blood flow velocity (pBFV) baseline in POAG eyes was significantly lower than in healthy eyes. Whereas pBFV was significantly increased during all follow-up periods after initiation of tafluprost treatment. Weindler et al. [46] used OCT-A to compare the effect of topical tafluprost or surgical treatment on macular region flow density in patients with POAG. The blood flow density of the lower segment of the superficial plexus in the macular area of the eyes treated with tafluprost was significantly higher than in the postoperative eyes. In a prospective observational study, Ishigaki et al. used [49] laser Doppler flowmetry (LDF) to measure the choroidal blood flow in the macular region of patients with POAG before and after tafluprost instillation. The flow (blood flow) and volume (moving red blood cells in tissues) of the choroidal capillaries were significantly increased after tafluprost administration for 4 or 8 weeks, while velocity (mean blood flow velocity) did not change significantly. It is suggested that the administration of tafluprost could improve the choroidal microcirculation in the macular region of patients with POAG. It is speculated that tafluprost increased the blood flow by dilating the choroidal microcirculation blood vessels without affecting the blood flow velocity. However, these studies examined the effects of tafluprost only in patients with POAG but not in healthy subjects. Therefore, it is difficult to determine whether the increase of ocular circulation in the macular region after tafluprost treatment is a unique phenomenon of self-regulation disruption in patients with POAG or whether it can be applied to normal subjects as well.
Ocular Pulse Amplitude (OPA)
OPA is the difference between the systolic and diastolic IOP during the IOP measurement [50]. OPA is thought to be caused by the blood volume pumped into the eye (mainly the choroidal bed) during each cardiac cycle. Jin et al. [51] modeled the origin of the ocular pulse and showed that the OPA and choroidal dilation could deform the ONH with a net shearing of neural tissues within the neuroretinal rim. The OPA might play a role in the clinical course of glaucoma [52]. Seo et al. [53] used dynamic contour tonometry to compare the OPA-lowering effects of preservative-free tafluprost and dorzolamide–timolol fixed combination (DTFC) in patients with NTG and POAG. The results showed that the OPA-lowering effects of tafluprost were significantly greater than those of DTFC at 6 months after administration.
Possible Mechanism of Improvement of OBF by Tafluprost
ET-1 is one of the most potent vasoactive peptides. It acts as a vasoconstrictor by binding to its receptor (usually the ETA receptor) on vascular smooth muscle, leading to an increase in intracellular free Ca2+ concentration by the continuous input of exogenous Ca2+ through different Ca2+ entry channels [54]. Studies have reported elevated ET-1 levels in plasma and aqueous humor of patients with glaucoma. Shoshani et al. found that compared with the non-glaucoma control group, ET-1 levels in plasma were increased significantly in patients with NTG (as opposed to patients with high tension glaucoma, HTG). However, patients with HTG only had a significant increase in the level of ET-1 in aqueous humor. These results indicate that in NTG, ET-1 might be involved in local and systemic vascular disorders. In contrast, the role of ET-1 in HTG might be mainly limited to the eye [55]. In animal models, a 2- to 2.5-fold increase was observed in aqueous humor immunoreactive ET-1 levels for rats subjected to elevated IOP compared to controls [56]. Intravitreal injection of ET-1 solution decreased ONH blood flow [34], while multiple intravitreal injections of ET-1 induced chronic hypoperfusion in the ONH and retina. This presumably caused a decrease in the neurofilament light chain content and axon number in the optic nerve [57]. Thus, ET-1 may be involved in the pathological process of OBF disorders in patients with glaucoma and might be playing a potential role in the pathogenesis of glaucoma [19, 55]. Kurashima et al. [34] used the isolated ciliary artery of male rabbits to observe the effect of tafluprost on the ET-1-induced contraction of the isolated ciliary artery. Furthermore, tafluprost concentration-dependently relaxed the ET-1-induced ciliary artery contraction. According to the mechanism of action of ET-1, the possible mechanisms of the tafluprost antagonistic effect on ET-1 are speculated as follows:
-
1.
Since tafluprost has no affinity for ETA receptors [22], it does not have any direct antagonistic effect on ETA receptors.
-
2.
In rhesus monkeys, the increased tissue blood velocity in the ONH returned to the pre-treated level after 180 min following tafluprost administration, while IOP remained at the lowest level [22]. The finding suggests that the improvement in blood flow caused by tafluprost was not dependent on an increase in ocular perfusion pressure secondary to altered IOP [58].
-
3.
Dong et al. [59] found that tafluprost could concentration-dependently dilate the ciliary arteries of rabbits, which were constricted by the high concentration of potassium solution. The degree of dilation was independent of L-NAME (an NO synthase inhibitor), indomethacin (cyclooxygenase inhibitor), or denudation of the vascular endothelium. Thus, the relaxing effect of tafluprost does not depend on the production of endodermal vasodilators such as NO and prostacyclin. Furthermore, tafluprost’s effect on ONH circulation disappeared after the intravenous injection of indomethacin in monkeys, suggesting that tafluprost might function through the secondary synthesis of prostaglandins in vivo [37]. Interestingly, indomethacin reduced the concentration of intracellular free Ca2+ ([Ca2+]i) in the isolated ciliary arteries of WT mice induced by 3 mM tafluprost, but not at higher doses [60]. These contradictory results require further in-depth studies to unravel the exact mechanism.
-
4.
Abe et al. [60] demonstrated that tafluprost could concentration-dependently reduce the increase of [Ca2+]i in the isolated ciliary arteries of WT mice induced by high potassium solution. Thus, tafluprost might play an antagonistic role to ET-1 by inhibiting the increased [Ca2+]i concentration. However, Dong’s study [59] showed that the diastolic effect of tafluprost on the ciliary arteries of rabbits was not affected by histamine, thapsigargin (an inhibitor of the sarcoendoplasmic reticulum (SR) Ca2+-ATPase), and ouabain (Na+-K+-ATPase inhibitor). This indicates that the relaxing effect of tafluprost did not depend on the release and restoration of Ca2+ from SR and the promotion of Ca2+ extrusion. Thus, tafluprost did not affect the [Ca2+]i cycle or the Ca2+ extrusion component of the extracellular Ca2+ ([Ca2+]e) cycle. In addition, the investigators found that the relaxing effect of tafluprost was not dependent on the voltage-dependent Ca2+ channel. Further, Dong et al. [59] reported during the depletion of [Ca2+]e, the [Ca2+]i concentration increased upon reintroduction of [Ca2+]e, and tafluprost decreased the amplitude of [Ca2+]i concentration upon this reintroduction. These results indicated that tafluprost inhibits the Ca2+ entry at least in part by suppressing the capacitative pathway through the plasma membrane from the extracellular space. However, more detailed evidence is vital to prove this concept.
-
5.
Abe et al. [60] found that tafluprost significantly reduced the [Ca2+]i concentration in isolated ciliary artery strips of EP2 receptor-deficient mice compared with WT mice. The effect of tafluprost on [Ca2+]i might be partially realized through the EP2 receptor. Since the acid form of tafluprost has no binding affinity for EP2 receptors [61], the involvement of EP2 receptors in tafluprost-associated reduction of [Ca2+]i concentration might be an indirect mechanism. Similar to humans, in mice, the EP2 receptor is highly expressed in all retinal layers [62] so the conjecture also seems true in humans.
Furthermore, tafluprost has a more long-lasting effect than other PGAs in improving OBF. It is speculated that the difluoro group at carbon-15 might contribute to its metabolic stability and long-lasting effect, as it enables tafluprost to resist oxidation by 15-hydroxyl prostaglandin dehydrogenase in the ONH and blood [34]. Figure 2 summarizes the possible mechanisms discussed above.
Summary and Prospects
The 0.0015% tafluprost eye drops have been widely used in clinical practice, but the mechanism of action is not yet fully understood. In addition to lowering IOP, the beneficial effects of 0.0015% tafluprost eye drops on OBF may be one of the mechanisms of action for glaucoma therapeutics. Several animal experiments showed that topical tafluprost significantly increased optic nerve head and retinal blood flow. A number of clinical trials also showed a beneficial effect of tafluprost on optic nerve head and macula blood flow, and a good ocular pulse amplitude-lowering effect. Furthermore, some results indicate that the OBF-improving effect of tafluprost is probably independent from its IOP-lowering effect, which also is expected to improve OBF. But, there are still a few conflicting results. Exploring the effect of tafluprost on OBF remains challenging.
First, previous reports studying the effect of tafluprost on OBF mainly focused on superficial retinal blood flow. Thus, deep retinal and choroidal-related studies are limited. Importantly, choroidal blood flow, especially in the peripapillary area, is closely related to the glaucoma optic nerve damage. So it is necessary to explore the effect of tafluprost on the deep retinal and choroidal layer blood flow. New OBF evaluation techniques such as swept-source optical coherence tomography angiography (SS-OCTA) with a long wavelength (1050 nm) can also be applied and developed for more robust deep layer imaging. The aforementioned technique enables automatic identification and stratification of deep retinal and choroidal blood flow [63]. In addition, to ensure comparability of data between groups, the Delta method can be used to incorporate all confounding factors (such as age, sex, IOP, physical activity, and systemic disease) [64].
Secondly, there is still a lack of evidence in long-term follow-up for assessing the effects of improved OBF on the visual field, visual acuity, and nerve fiber layer thickness. Therefore, more studies are required on patients with ocular hypertension and different types of glaucoma, such as OAG and NTG. These future studies will help explore the role of long-term medication in improving blood flow, preventing ocular hypertension from developing into glaucoma besides delaying the progression of glaucoma.
In exploring the possible mechanism of action of tafluprost in improving OBF, the studies were mostly based on the isolated ciliary artery of animals. Although this method is relatively simple and easy to perform, no blood flow perfusion and neuro-humoral regulation mechanisms are considered. Thus, such ex vivo studies cannot reproduce the actual in vivo environment. Therefore, the conclusions drawn from these studies may not necessarily apply to humans. Moreover, studies on the mechanism of tafluprost inhibiting ET-1-induced vasoconstriction were limited to the ciliary arteries. However, other ocular vessels such as retinal arteries or microvessels should also be involved. Therefore, researchers must adopt more reasonable experimental methods and designs to explore the exact mechanism of IOP reduction and improvement of OBF. Nevertheless, the outcomes of these studies can guide us in developing new drugs for treating glaucoma.
In conclusion, decreased OBF is one of the important factors for glaucomatous optic nerve damage. Patients with glaucoma develop reduced OBF velocity, blood flow, and blood vessel density. Several animal and clinical studies have demonstrated that tafluprost can improve OBF and ocular microcirculation. But, there are still a few conflicting results. More well-designed studies are required to validate these findings.
References
Surgucheva I, McMahan B, Ahmed F, Tomarev S, Wax MB, Surguchov A. Synucleins in glaucoma: implication of gamma-synuclein in glaucomatous alterations in the optic nerve. J Neurosci Res. 2002;68(1):97–106.
Tham YC, Li X, Wong TY, Quigley HA, Aung T, Cheng CY. Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology. 2014;121(11):2081–90.
Bourne RRA, Flaxman SR, Braithwaite T, et al. Magnitude, temporal trends, and projections of the global prevalence of blindness and distance and near vision impairment: a systematic review and meta-analysis. Lancet Glob Health. 2017;5(9):e888–97.
Quigley HA, Broman AT. The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol. 2006;90(3):262–7.
Lee JY, Sung KR, Lee JY. Comparison of the progression of high- and low-tension glaucoma as determined by two different criteria. Korean J Ophthalmol. 2016;30(1):40–7.
Kuerten D, Fuest M, Koch EC, Koutsonas A, Plange N. Retrobulbar hemodynamics and visual field progression in normal tension glaucoma: a long-term follow-up study. Biomed Res Int. 2015;2015: 158097.
Shin JD, Wolf AT, Harris A, et al. Vascular biomarkers from optical coherence tomography angiography and glaucoma: where do we stand in 2021? Acta Ophthalmol. 2021. https://doi.org/10.1111/aos.14982.
Shoji T, Zangwill LM, Akagi T, et al. Progressive macula vessel density loss in primary open-angle glaucoma: a longitudinal study. Am J Ophthalmol. 2017;182:107–17.
Hou H, Moghimi S, Zangwill LM, et al. Macula vessel density and thickness in early primary open-angle glaucoma. Am J Ophthalmol. 2019;199:120–32.
Chen HS, Liu CH, Wu WC, Tseng HJ, Lee YS. Optical coherence tomography angiography of the superficial microvasculature in the macular and peripapillary areas in glaucomatous and healthy eyes. Invest Ophthalmol Vis Sci. 2017;58(9):3637–45.
Choi J, Kook MS. Systemic and ocular hemodynamic risk factors in glaucoma. Biomed Res Int. 2015;2015: 141905.
Liu L, Jia Y, Takusagawa HL, et al. Optical coherence tomography angiography of the peripapillary retina in glaucoma. JAMA Ophthalmol. 2015;133(9):1045–52.
Yarmohammadi A, Zangwill LM, Diniz-Filho A et al. Relationship between optical coherence tomography angiography vessel density and severity of visual field loss in glaucoma. Ophthalmology. 2016;123(12):2498–508.
Bojikian KD, Chen PP, Wen JC. Optical coherence tomography angiography in glaucoma. Curr Opin Ophthalmol. 2019;30(2):110–6.
Moghimi S, Zangwill LM, Penteado RC, et al. Macular and optic nerve head vessel density and progressive retinal nerve fiber layer loss in glaucoma. Ophthalmology. 2018;125(11):1720–8.
Kwon JM, Weinreb RN, Zangwill LM, Suh MH. Juxtapapillary deep-layer microvasculature dropout and retinal nerve fiber layer thinning in glaucoma. Am J Ophthalmol. 2021;227:154–65.
Jia Y, Wei E, Wang X, et al. Optical coherence tomography angiography of optic disc perfusion in glaucoma. Ophthalmology. 2014;121(7):1322–32.
Kwon JM, Weinreb RN, Zangwill LM, Suh MH. Parapapillary deep-layer microvasculature dropout and visual field progression in glaucoma. Am J Ophthalmol. 2019;200:65–75.
Rosenthal R, Fromm M. Endothelin antagonism as an active principle for glaucoma therapy. Br J Pharmacol. 2011;162(4):806–16.
Sutton A, Gouws P, Ropo A. Tafluprost, a new potent prostanoid receptor agonist: a dose-response study on pharmacodynamics and tolerability in healthy volunteers. Int J Clin Pharmacol Ther. 2008;46(8):400–6.
Nakajima T, Matsugi T, Goto W, et al. New fluoroprostaglandin F(2alpha) derivatives with prostanoid FP-receptor agonistic activity as potent ocular-hypotensive agents. Biol Pharm Bull. 2003;26(12):1691–5.
Takagi Y, Nakajima T, Shimazaki A, et al. Pharmacological characteristics of AFP-168 (tafluprost), a new prostanoid FP receptor agonist, as an ocular hypotensive drug. Exp Eye Res. 2004;78(4):767–76.
Hellberg MR, Sallee VL, McLaughlin MA, et al. Preclinical efficacy of travoprost, a potent and selective FP prostaglandin receptor agonist. J Ocul Pharmacol Ther. 2001;17(5):421–32.
Ota T, Murata H, Sugimoto E, Aihara M, Araie M. Prostaglandin analogues and mouse intraocular pressure: effects of tafluprost, latanoprost, travoprost, and unoprostone, considering 24-hour variation. Invest Ophthalmol Vis Sci. 2005;46(6):2006–11.
Traverso CE, Ropo A, Papadia M, Uusitalo H. A phase II study on the duration and stability of the intraocular pressure-lowering effect and tolerability of tafluprost compared with latanoprost. J Ocul Pharmacol Ther. 2010;26(1):97–104.
Konstas AG, Boboridis KG, Kapis P, et al. 24-hour efficacy and ocular surface health with preservative-free tafluprost alone and in conjunction with preservative-free dorzolamide/timolol fixed combination in open-angle glaucoma patients insufficiently controlled with preserved latanoprost monotherapy. Adv Ther. 2017;34(1):221–35.
Sutton A, Gilvarry A, Ropo A. A comparative, placebo-controlled study of prostanoid fluoroprostaglandin-receptor agonists tafluprost and latanoprost in healthy males. J Ocul Pharmacol Ther. 2007;23(4):359–65.
Orme M, Collins S, Dakin H, Kelly S, Loftus J. Mixed treatment comparison and meta-regression of the efficacy and safety of prostaglandin analogues and comparators for primary open-angle glaucoma and ocular hypertension. Curr Med Res Opin. 2010;26(3):511–28.
Izumi N, Nagaoka T, Sato E, et al. Short-term effects of topical tafluprost on retinal blood flow in cats. J Ocul Pharmacol Ther. 2008;24(5):521–6.
Stjernschantz J, Selen G, Astin M, Resul B. Microvascular effects of selective prostaglandin analogues in the eye with special reference to latanoprost and glaucoma treatment. Prog Retin Eye Res. 2000;19(4):459–96.
Roth S. The effects of halothane on retinal and choroidal blood flow in cats. Anesthesiology. 1992;76(3):455–60.
Roth S, Pietrzyk Z, Crittenden AP. The effects of enflurane on ocular blood flow. J Ocul Pharmacol. 1993;9(3):251–6.
Akaishi T, Kurashima H, Odani-Kawabata N, Ishida N, Nakamura M. Effects of repeated administrations of tafluprost, latanoprost, and travoprost on optic nerve head blood flow in conscious normal rabbits. J Ocul Pharmacol Ther. 2010;26(2):181–6.
Kurashima H, Watabe H, Sato N, Abe S, Ishida N, Yoshitomi T. Effects of prostaglandin F(2alpha) analogues on endothelin-1-induced impairment of rabbit ocular blood flow: comparison among tafluprost, travoprost, and latanoprost. Exp Eye Res. 2010;91(6):853–9.
Giannico AT, Lima L, Shaw GC, Russ HH, Froes TR, Montiani-Ferreira F. Effects of prostaglandin analogs on blood flow velocity and resistance in the ophthalmic artery of rabbits. Arq Bras Oftalmol. 2016;79(1):33–6.
Lanzl I, Hamacher T, Rosbach K, et al. Preservative-free tafluprost in the treatment of naive patients with glaucoma and ocular hypertension. Clin Ophthalmol. 2013;7:901–10.
Mayama C, Ishii K, Saeki T, Ota T, Tomidokoro A, Araie M. Effects of topical phenylephrine and tafluprost on optic nerve head circulation in monkeys with unilateral experimental glaucoma. Invest Ophthalmol Vis Sci. 2010;51(8):4117–24.
Yaoeda K, Shirakashi M, Abe H. Microcirculation in the optic nerve head before and after instillation of tafluprost in healthy humans. Rinsho Ganka (Jpn J Clin Ophthalmol). 2010;64(4):455–8 (in Japanese).
Ohguro I, et al. Effects of administration of tafluprost on optic nerve head blood flow in patients with normal tension glaucoma. Ganka. 2010;52(13):1921–6 (in Japanese).
Sugiyama T, Shibata M, Kojima S, et al. Changes in microcirculation in the optic nerve head following topical tafluprost in eyes with primary open-angle glaucoma. Rinsho Ganka (Jpn J Clin Ophthalmol). 2011;65(4):475–9 (in Japanese).
Shibata M, Sugiyama T, Kojima S, et al. Effects on visual field, morphology and microcirculation of optic nerve head following tafluprost treatment for 3 years in patients with glaucoma. Jpn J Clin Ophthalmol. 2015;69(5):741–7 (in Japanese).
Jonas JB, Wang YX, Dong L, Panda-Jonas S. High myopia and glaucoma-like optic neuropathy. Asia Pac J Ophthalmol (Phila). 2020;9(3):234–8.
Jonas JB, Weber P, Nagaoka N, Ohno-Matsui K. Glaucoma in high myopia and parapapillary delta zone. PLoS ONE. 2017;12(4): e0175120.
Tsuda S, Yokoyama Y, Chiba N, et al. Effect of topical tafluprost on optic nerve head blood flow in patients with myopic disc type. J Glaucoma. 2013;22(5):398–403.
Iida Y, Akagi T, Nakanishi H, et al. Retinal blood flow velocity change in parafoveal capillary after topical tafluprost treatment in eyes with primary open-angle glaucoma. Sci Rep. 2017;7(1):5019.
Weindler H, Spitzer MS, Schultheiss M, Kromer R. OCT angiography analysis of retinal vessel density in primary open-angle glaucoma with and without tafluprost therapy. BMC Ophthalmol. 2020;20(1):444.
Kurysheva NI. Assessment of the optic nerve head, peripapillary, and macular microcirculation in the newly diagnosed patients with primary open-angle glaucoma treated with topical tafluprost and tafluprost/timolol fixed combination. Taiwan J Ophthalmol. 2019;9(2):93–9.
Kurysheva NI, Maslova EV, Trubilina AV, Fomin AV, Lagutin MB. Pattern visual evoked potentials and their relation to the peripapillary and retrobulbar blood flow in glaucoma. Vestn Oftalmol. 2018;134(3):19–27.
Ishigaki J, Miyaka S, Harino S, et al. Effect of Tafluprost on choroidal blood flow in glaucoma. Atarashii Ganka (J Eye). 2010;27(8):1115–8 (in Japanese).
Kaufmann C, Bachmann LM, Robert YC, Thiel MA. Ocular pulse amplitude in healthy subjects as measured by dynamic contour tonometry. Arch Ophthalmol. 2006;124(8):1104–8.
Jin Y, Wang X, Zhang L, et al. Modeling the origin of the ocular pulse and its impact on the optic nerve head. Invest Ophthalmol Vis Sci. 2018;59(10):3997–4010.
Cheng L, Ding Y, Duan X, Wu Z. Ocular pulse amplitude in different types of glaucoma using dynamic contour tonometry: diagnosis and follow-up of glaucoma. Exp Ther Med. 2017;14(5):4148–52.
Seo DR, Ha SJ. Comparison of ocular pulse amplitude lowering effects of preservative-free tafluprost and preservative-free dorzolamide-timolol fixed combination eyedrops. Biomed Res Int. 2015;2015: 435874.
Rubanyi GM, Polokoff MA. Endothelins: molecular biology, biochemistry, pharmacology, physiology, and pathophysiology. Pharmacol Rev. 1994;46(3):325–415.
Shoshani YZ, Harris A, Shoja MM, et al. Endothelin and its suspected role in the pathogenesis and possible treatment of glaucoma. Curr Eye Res. 2012;37(1):1–11.
Prasanna G, Hulet C, Desai D, et al. Effect of elevated intraocular pressure on endothelin-1 in a rat model of glaucoma. Pharmacol Res. 2005;51(1):41–50.
Sasaoka M, Taniguchi T, Shimazawa M, Ishida N, Shimazaki A, Hara H. Intravitreal injection of endothelin-1 caused optic nerve damage following to ocular hypoperfusion in rabbits. Exp Eye Res. 2006;83(3):629–37.
Liu CJ, Ko YC, Cheng CY, Chou JC, Hsu WM, Liu JH. Effect of latanoprost 000.5% and brimonidine tartrate 0.2% on pulsatile ocular blood flow in normal tension glaucoma. Br J Ophthalmol. 2002;86(11):1236–9.
Dong Y, Watabe H, Su G, Ishikawa H, Sato N, Yoshitomi T. Relaxing effect and mechanism of tafluprost on isolated rabbit ciliary arteries. Exp Eye Res. 2008;87(3):251–6.
Abe S, Watabe H, Takaseki S, Aihara M, Yoshitomi T. The effects of prostaglandin analogues on intracellular Ca2+ in ciliary arteries of wild-type and prostanoid receptor-deficient mice. J Ocul Pharmacol Ther. 2013;29(1):55–60.
Aihara M. Clinical appraisal of tafluprost in the reduction of elevated intraocular pressure (IOP) in open-angle glaucoma and ocular hypertension. Clin Ophthalmol. 2010;4:163–70.
Biswas S, Bhattacherjee P, Paterson CA. Prostaglandin E2 receptor subtypes, EP1, EP2, EP3 and EP4 in human and mouse ocular tissues—a comparative immunohistochemical study. Prostaglandins Leukot Essent Fatty Acids. 2004;71(5):277–88.
Stanga PE, Tsamis E, Papayannis A, Stringa F, Cole T, Jalil A. Swept-source optical coherence tomography angio (Topcon Corp, Japan): technology review. Dev Ophthalmol. 2016;56:13–7.
Brucher VC, Storp JJ, Eter N, Alnawaiseh M. Optical coherence tomography angiography-derived flow density: a review of the influencing factors. Graefes Arch Clin Exp Ophthalmol. 2020;258(4):701–10.
Acknowledgements
Funding
This work was supported by the National Natural Science Foundation of China [Grant Numbers 81970801 to XD]; the Hunan Province research and development plan funding projects in key areas [Grant Numbers 2020SK2133 to XD]; the Science and Technology Foundation of Changsha, Hunan, China [Grant Numbers kh1801229 to XD]; the Natural Science Foundation of Hunan Province, China [Grant Numbers 2019JJ40001 to XD]; and the Science and Technology Foundation of Aier Eye Hospital Group, China [Grant Numbers AR1906D1, AM1906D2 to XD]. The National Natural Science Foundation of China is funding the journal’s Rapid Service fee.
Editorial, Medical Writing, and Other Assistance
The authors thank China Santen Medical Affairs [China Santen Medical Affairs, Santen Pharmaceutical (China)Co., Ltd.] for their assistance with conducting an extensive literature search.
Author Contributions
Xuanchu Duan proposed and designed the study. Xiaoyu Zhou and Xiang Yang searched the literature. Xinyue Zhang drafted the manuscript. Dengming Zhou, Baihua Chen and Yang Zhao revised the manuscript. All authors read and approved the final manuscript.
Disclosures
Xinyue Zhang, Xiaoyu Zhou, Yang Zhao, Xiang Yang, Dengming Zhou, Baihua Chen and Xuanchu Duan confirm that they have no conflicts of interest to declare.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Data Availability
All data generated or analyzed during this study are included in this published article/as supplementary information files.
Author information
Authors and Affiliations
Corresponding author
Additional information
Chemical compounds studied in this article are tafluprost (PubChem CID 9868491), latanoprost (PubChem CID 5311221), travoprost (PubChem CID 5282226), endothelin-1 (PubChem CID 16212950), and bimatoprost (PubChem CID 5311027).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Zhang, X., Zhou, X., Zhao, Y. et al. Effects of Tafluprost on Ocular Blood Flow. Ophthalmol Ther 11, 1991–2003 (2022). https://doi.org/10.1007/s40123-022-00566-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-022-00566-z