Abstract
Introduction
Carbapenem-resistant organisms (CRO) have emerged as a major global public health threat, but their role in critical acute pancreatitis (CAP) is still not defined. Our study aims to investigate risk factors associated with mortality and drug resistance among CAP patients with CRO infection.
Methods
The clinical characteristics of CAP patients with CRO infection and drug resistance of causative pathogens from January 1, 2016, to October 1, 2021, were reviewed retrospectively. Independent risk factors for mortality were determined via univariate and multivariate analyses.
Result
Eighty-two CAP patients suffered from CRO infection, with mortality of 60.0%. The independent risk factors for mortality were procalcitonin > 5 ng/L (hazard ratio = 2.300, 95% confidence interval = 1.180–4.484, P = 0.014) and lactic acid > 2 mmol/L (hazard ratio = 2.101, 95% confidence interval = 1.151–3.836, P = 0.016). The pancreas was the main site of infection, followed by lung, bloodstream and urinary tract. Klebsiella pneumoniae and Acinetobacter baumannii were the main pathogenic bacteria of CRO strains with extensive antibiotic resistance (> 60%) to 6 of 8 common antibiotics, except sulfamethoxazole (56.3%) and tigecycline (33.2%).
Conclusion
CRO infection has become a serious threat for CAP patients, with high rates of mortality. Procalcitonin and lactic acid represent two independent risk factors for mortality in CAP patients with CRO infection. Klebsiella pneumoniae and Acinetobacter baumannii are the primary categories of CRO pathogens. Greater efforts are needed for early prevention and prompt treatment of CRO infections in CAP patients.
Similar content being viewed by others
Why carry out this study? |
Carbapenem-resistant organisms are considered a major global public health threat. |
Critical acute pancreatitis is the most severe form of acute pancreatitis, and patients with critical acute pancreatitis (CAP) are at the greatest risk of acquiring infections caused by carbapenem-resistant organisms. |
This study aimed to determine the mortality risk factors and drug resistance of causative pathogens in this multi-threat scenario. |
What was learned from the study? |
In patients with critical acute pancreatitis, infection with carbapenem-resistant organisms has become a serious threat, with high mortality. |
Procalcitonin and lactic acid represent two independent mortality risk factors in this critical population. |
Carbapenem-resistant Klebsiella pneumoniae and carbapenem-resistant Acinetobacter baumannii are the major species requiring more attention in prevention. |
Introduction
Carbapenem was once considered the most effective antibiotic for multidrug-resistant bacterial infections, but increasing resistance rates indicate that carbapenem-resistant organisms (CRO) have emerged as a frequent and challenging problem around the world [1, 2]. CRO comprise lethal pathogens such as carbapenem-resistant Klebsiella pneumoniae (CRKP), Acinetobacter baumannii (CRAB) and Pseudomonas aeruginosa, resulting in increasing morbidity given the lack of safe and effective antibiotics [2,3,4,5,6].
Severe acute pancreatitis (SAP) is a category of acute pancreatitis (AP) complicated by persistent organ failure, with mortality of up to 30% [7]. In addition to the first peak mortality rate of SAP, which is caused by systemic inflammatory response syndrome and subsequent organ failure, the second peak results from infection and related organ failure [8].
Compensatory anti-inflammatory response syndrome in SAP patients induces immune suppression or deficiency which predispose them to secondary bacterial infections due to insufficient immune reaction [9]. Hence, SAP is associated with high mortality, requiring invasive treatment and prolonged intensive care unit stays so that it does not develop into critical acute pancreatitis (CAP), which is considered the most fatal category, with mortality of up to 34% [10,11,12,13]. Overuse of antibiotics for AP patients in China is ranked highest in the world; thus Chinese AP patients are more susceptible to antimicrobial-resistant infections [14].
According to Windsor et al., organ failure caused by noninfectious cytokine storm may be difficult to distinguish from infections among AP patients, especially CAP patients with poor clinical outcomes due to persistent organ failure complicated by infection [12]. Therefore, it is necessary to dynamically monitor bacterial infections, especially CRO infections, and investigate the risk factors associated with mortality in this population [15]. To date, several studies have demonstrated that complications due to the widespread incidence of multidrug-resistant bacterial infections have increased the mortality rate in AP patients [16,17,18,19,20]. However, no study has focused on CAP patients with CRO infection.
Therefore, to increase the survival rate among CAP patients with CRO infection, alternative treatment options in this population are essential. Our primary objective herein was to identify the risk factors of mortality in order to improve the outcomes and advance the therapeutic regimens of these critically ill patients. The secondary objective was to investigate the distribution and rates of drug resistance of CRO pathogens which may shed light on appropriate antibiotic treatment strategies.
Methods
Study Design and Setting
CAP patients who developed CRO infections were enrolled between January 1, 2016, and October 1, 2021, from two tertiary-care teaching hospitals—Xiangya Hospital, a 3500-bed facility, and the Third Xiangya Hospital, an 1800-bed facility, both affiliated to Central South University in Changsha, Hunan, China. Patients between 18 and 80 years old were enrolled, excluding patients with conservative treatment of infected pancreatic necrosis (IPN) or only a positive result of extra-pancreatic infections. Clinical characteristics included age, gender, etiology, site of infection, species of bacteria, referral, length of hospital and intensive care unit stays, antibiotic therapy and details of therapeutic treatments for IPN. Laboratory data were recorded within the first 24 h after the first interventions for IPN. If patients had two or more of the same laboratory test during the first 24 h, the earliest was prioritized for inclusion in the analyses. The follow-up period was 90 days or until death after the date of first interventions. Univariate and multivariate Cox regression analyses were performed to identify the mortality risk factors as shown in the Supplementary Material.
Ethics
Because of the retrospective nature of this cohort study, the institutional review boards of both Xiangya Hospital (no. 202202038) and the Third Xiangya Hospital (no. 22028) waived the need for direct patient enrollment and informed consent. Information was gathered from electrical medical systems in an anonymous manner, where all authors could ensure the confidentiality of patient data.
Patients and Management Protocol
At the initial admission, all patients were assessed and managed via a multidisciplinary team, including pancreatic surgeons and emergency, gastroenterology and intensive care unit physicians, according to the latest international guidelines [21]. All the CAP patients with CRO infection were diagnosed with positive culture results after first interventional or surgical treatment instead of fine-needle aspiration, which was never used in either medical center. Decisions about the IPN treatments depended on the individual patient’s condition. The antibiotic therapy we recorded was the initial regimen after first intervention (3 days), which could be adjusted according to the patient’s condition. Tigecycline (TGC) was prescribed at 50 mg every 12 h (100 mg for the first dose).
Definitions
CRO, including carbapenem-resistant Enterobacteriaceae, CRAB and carbapenem-resistant P. aeruginosa, were defined as strains resistant to at least one of the carbapenem agents, and CRO infections were diagnosed based on the clinical manifestations with positive culture according to the Centers for Disease Control and Prevention criteria [22]. Mortality was defined as death within 90 days from enrollment. The etiological criteria were as follows: (1) gallstones, based on radiological evidence of abdominal ultrasonography and increased serum alanine aminotransferase levels; (2) alcoholism, drinking > 50 g/day for at least 1 year; (3) hypertriglyceridemia, serum triglycerides more than 1000 mg/dL without the above two causes [7]. Classification of AP was made using determinant-based classification criteria: (1) mild AP, no pancreatic necrosis and no organ failure; (2) moderate AP, sterile pancreatic necrosis and/or transient organ failure; (3) SAP, IPN or persistent organ failure; (4) CAP, IPN and persistent organ failure [10]. Organ failure was evaluated on the Marshall score as > 2 for three organ systems (respiratory, cardiovascular, or renal). Referral patients were defined as those transferred from other hospitals (mostly from primary hospitals). IPN was defined as the presence of gas bubbles within (peri)pancreatic necrosis on computed tomography and a positive culture of (peri)pancreatic necrotic fluid obtained during the first intervention. Carbapenem resistance was defined as resistance to any carbapenem minimum inhibitory concentration ≥ 2 mg/L). Carbapenem (high-dose, extended-infusion) was defined as an appropriate therapy at the early phase.
Microbiology
All specimens were collected by clinicians when patients were given the first intervention for IPN or suspected extra-pancreatic infections, and were immediately transported to the clinical microbiology laboratory following standard procedures. Identification and drug resistance tests of CRO were carried out using a VITEK-2 system and broth microdilution method, respectively. Intermediate susceptibility in vitro was considered as resistance.
Statistical Analysis
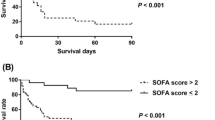
Categorical variables, expressed in absolute numbers with percentages, and continuous variables, described using mean and standard deviations, were compared with univariate Cox regression analysis. Only the variables with P values < 0.05 in univariate Cox regression analysis were further analyzed in multivariate Cox regression analysis, which was performed to determine the independent risk factors related to overall mortality. The results of the multivariate analysis are described as hazard ratio (HR) with 95% confidence interval (CI). Proportional hazards assumption was satisfied throughout. Kaplan–Meier curves were used to plot the distribution for the independent risk factors (log-rank test). A P value < 0.05 from two-tailed tests was considered statistically significant, and statistical analysis was performed using SPSS 24.0 software.
Results
Clinical Characteristics and Risk Factors of 90-Day Mortality
During the 5-year period, 82 CAP patients experienced CRO infections, including pancreatic and extra-pancreatic infections, with mortality of 60.0% (49 of 82). Fifty-eight patients (70.7%) were male, and hypertriglyceridemia (n = 32, 39.0%) and gallstones (n = 29, 35.4%) were the main etiologies in our cohort, followed by alcoholism (n = 6, 7.3%) and others (n = 15, 18.3%). Sixty-eight patients (82.9%) were referred from other hospitals after 2 days from onset of AP. Only seven patients (8.5%) had recurrent infections, and fungal strains were found in 29 patients (35.4%). For conservative treatment before intervention, combined antibiotics were the leading choice (n = 33, 40.2%), followed by wide-spectrum antibiotics (n = 30, 36.6%) and carbapenem (n = 19, 23.2%). A total of 36, 31, 13 and 2 patients were infected with one, two, three and four species, respectively. Forty-two and 40 patients received the first intervention for IPN within and after 28 days of onset of AP, respectively. Forty-four (53.7%) patients required mechanical ventilation support for respiratory failure. Percutaneous catheter drainage to minimal-access retroperitoneal necrosectomy was the most common choice (n = 36, 43.9%) for IPN. Carbapenem combined with TGC and carbapenem alone (high-dose, extended-infusion) were the most widely used subsequent antibiotic therapy in 31 and 25 patients, respectively. The clinical manifestation and laboratory variables for the 82 CAP patients with CRO infection are shown in Table 1.
Age (P = 0.029), mechanical ventilation (P < 0.001), number of infection sites (P = 0.006), lactic acid (P = 0.002), procalcitonin (P < 0.001) and hemorrhage (P = 0.004) were significantly associated with mortality in the univariate analysis (Table 2). Only procalcitonin > 5 ng/L (HR = 2.300, 95% CI 1.180–4.484, P = 0.014) and lactic acid > 2 mmol/L (HR = 2.101, 95% CI 1.151–3.836, P = 0.016) remained statistically significant in the multivariate analysis (Table 2). The survival time with independent risk factors is shown via Kaplan–Meier curve in Fig. 1. For the outcome of patients with procalcitonin > 5 mmol/L versus ≤ 5 mmol/L, the survival rate in the former group was significantly lower (10.0% vs. 57.7%, P < 0.001). Compared with the lactic acid ≤ 2 mmol/L group, the survival rate was significantly lower in the lactic acid > 2 mmol/L group (22.2% vs. 54.3%, P = 0.002).
Distribution and Drug Resistance of Strains
Table 3 shows in detail the distribution of all the respective bacterial species. The main pathogenic bacterium was CRKP (n = 77, 38.9%), followed by CRAB (n = 74, 37.4%), CR-P. aeruginosa (n = 12, 6.1%), CR-Klebsiella ozaenae (n = 12, 6.1%) and others. The pancreas was the main site of infection, followed by the lung, bloodstream and urinary tract. CRKP was the primary bacteria for both pancreatic (n = 34) and bloodstream (n = 23) infection, and CRAB was the primary cause of pneumonia (n = 37). In Table 4, the drug resistance rates for CRO pathogens to six antibiotics were > 60% excluding sulfamethoxazole (56.3%) and TGC (33.2%). As the most common pathogen, CRKP was susceptible to TGC (16.9%) and sulfamethoxazole (36.4%). Furthermore, CRAB, the second most common pathogen, was only susceptible to TGC (31.1%).
Discussion
Carbapenems were previously considered the last-line choice for multidrug-resistant Gram-negative bacterial infections [3, 5, 23]. With the overuse of antibiotics in recent years, CRO have become an important pathogen of nosocomial infections. The family Enterobacteriaceae and non-fermentative bacteria constitute the vast majority of Gram-negative bacilli, which easily develop different antibiotic resistance mechanisms, and evolve into CRO by inducing position changes and enzyme production [24]. Uncontrollable infection secondary to CAP is the leading cause of mortality in the late phase of the disease [16]. Here, this first retrospective cohort study focusing on CAP patients with CRO infection is important to advancing the understanding of this critical population.
Mortality among CAP patients with CRO infection (60.8%) in our cohort was higher than that for CAP in previous reports, indicating that CAP complicated by CRO infection poses a greater risk [12, 18]. IPN nearly always leads to step-up therapeutic intervention instead of only antibiotics. Recently, Besselink et al. revealed that immediate intervention did not show superiority over delayed intervention for IPN in a prospective randomized trial [25]. The timing of necessary invasive intervention may vary with differences in progression of the disease. It is worth noting that procalcitonin > 5 ng/L and lactic acid > 2 mmol/L at the first intervention of CRO-infected CAP patients are independent risk factors associated with mortality. According to Singer et al., lactic acid levels in serum had a significant predictive value for diagnosis of septic shock [26]. For the first time, our study suggests that the timing of first intervention should focus on lactic acid during the pre-intervention phase. In line with a previous study, our findings confirmed that procalcitonin plays a key role in the evaluation of infections, which alerts us to timely clearance of the source of infection [5, 27]. For CRO-infected CAP patients, clinicians also need to consider the efficacy of the infectious source control which, although difficult to assess, may influence the duration of antibiotic therapy [28]. Therefore, these two independent risk factors may be potential markers for the timing of interventions, and need to be verified in future studies.
For the distribution of causative pathogens, CRKP was the main CRO pathogen in our cohort rather than CRAB, which could be explained by intestinal bacterial translocation and strong inherent drug resistance of CRKP. In China, CRKP and CRAB are two common nosocomial pathogens which are increasingly resistant to most antibiotics [22]. Our findings are consistent with previous studies in which Klebsiella pneumoniae, the most common pathogen among IPN patients, was found to be resistant to a large number of antibiotics [16, 29]. Pancreatic necrosis is initially aseptic but can progress to infected necrosis if infected with intestinal bacteria among AP patients; the lung was the most common site of extra-pancreatic infection in our cohort with CRAB, which constituted the primary pathogenic bacterium, thus alerting clinicians to be wary of CRAB ventilator-associated pneumonia and subsequent IPN [30]. Since conventional disinfection methods are not effective against CRAB or CRKP, immunocompromised patients, including CAP patients, may be more susceptible to infection caused by CRO attached to medical devices and clinicians’ hands in intensive care units without thorough sterilization [5, 31].
Similar to previous research, our study showed that CRO are highly resistant to most common antibiotics, which may be attributed to the clinical use of wholly prophylactic antibiotic prescription [17, 31]. The vast majority of CAP patients received antibiotics before the IPN intervention because of suspected infections with possible manifestations. In line with previous studies, our cohort demonstrated that antibiotic therapy before intervention did not significantly impact the outcomes, which may also increase the risk of drug resistance and incidence of fungal infections [5, 32]. Given the size and limitations of these retrospective data, the comparison between monotherapy and combination prophylactic antibiotic therapy remains to be studied. Consistent with recent guidelines, it may also indicate that the clinician should not use prophylactic antibiotics, especially carbapenems, until obtaining the microbiological culture results [28].
The detection of drug resistance is a necessary reference for guiding clinical antibiotic prescription; thus, we analyzed the rates of resistance rate for all the CRO for eight common antibiotics, which indicated that CRO were more than 60% resistant to six antibiotics, the exceptions being sulfamethoxazole and tigecycline, which may be attributed to the overuse of antibiotics in China [14]. Similar to a previous study, TGC and sulfamethoxazole may be recommended as appropriate treatment in our study for CRO infections in CAP patients due to susceptibility testing in vitro [5]. Microbiological data for polymyxin and ceftazidime-avibactam were not analyzed because only nine patients were tested for drug resistance to both. However, increasing resistance to last-line antibiotics is emerging as a serious concern and may also be associated with antimicrobial therapy failure due to uncertainty of adequate penetration in necrotic pancreatic tissue [28]. In our cohort, clinical microbiology laboratories use phenotypic tests based on actual growth inhibition, which can provide a full actual susceptibility picture. Moreover, our recommendations of antibiotic therapy, based on drug resistance profiles of the strains, need to be interpreted with caution, and doctors should select an appropriate antimicrobial regimen according to the specific clinical scenario which includes tissue penetration, plasma concentration, renal function and host response [33]. In this era of CRO, the next phase of fighting not only may focus on the development of novel antibiotics, such as imipenem–relebactam and cefiderocol, but may also investigate “new” therapeutic regimens from “old” antibiotics and prevent the occurrence of resistance.
Although many advances have taken place, there are also some limitations in this study. First was its retrospective nature, with inevitable bias and missing variables, especially mechanisms of resistance, prophylactic antibiotics before admission, and unevaluated penetration of antibiotics in pancreatic necrosis, which may play a key role in outcome. Second, the location of the pancreatic necrosis and subsequent choice of intervention which focused on the surgical aspect were not highlights of this study because of the specific focus on antibiotic therapy for infectious disease. Third, persistent organ failure caused by the severity of AP itself required particular attention. Patients with persistent organ failure could experience longer intensive care unit stays and more invasive procedures, which may result in more serious antimicrobial resistance. Fourth, data on Gram-positive bacterial co-infections were lacking, thereby producing bias due to unmeasured confounders. Fifth, procalcitonin and lactic acid were dichotomized for multivariable analysis, which may have introduced selection bias and thus needs to be verified in further study. Finally, a noninvasive novel diagnostic method for timing of therapeutic intervention is urgently needed in CAP patients with CRO infection. In all, our findings should be interpreted cautiously and validated in the future.
Conclusion
The clinical characteristics and antibiotic resistance among CAP patients with CRO infection are described in this study for the first time. CRKP and CRAB are the primary categories of CRO among this population. Procalcitonin and lactic acid are associated with mortality, and may be good prognostic markers for the timing of therapeutic intervention. TGC and sulfamethoxazole are recommended to treat CRO infection among CAP patients. To further advance empirical and definitive therapy for CAP patients with CRO infection, future studies should evaluate patient- and infection-specific factors so that we may treat these infections more appropriately.
References
van Duin D, Doi Y. The global epidemiology of carbapenemase-producing Enterobacteriaceae. Virulence. 2017;8(4):460–9.
Kunz Coyne AJ, El Ghali A, Holger D, Rebold N, Rybak MJ. Therapeutic strategies for emerging multidrug-resistant Pseudomonas aeruginosa. Infect Dis Ther. 2022;11(2):661–82.
Guo D, Dai W, Shen J, Zhang M, Shi Y, Jiang K, Guo L. Assessment of prophylactic carbapenem antibiotics administration for severe acute pancreatitis: an updated systematic review and meta-analysis. Digestion. 2022;13:1–9.
Doi Y. Treatment options for carbapenem-resistant gram-negative bacterial infections. Clin Infect Dis. 2019;69(Suppl 7):S565–75.
Wu D, Xiao J, Ding J, et al. Predictors of mortality and drug resistance among carbapenem-resistant enterobacteriaceae-infected pancreatic necrosis patients. Infect Dis Ther. 2021;10(3):1665–76.
Bartal C, Rolston KVI, Nesher L. Carbapenem-resistant Acinetobacter baumannii: colonization, infection and current treatment options. Infect Dis Ther. 2022;11(2):683–94.
Mederos MA, Reber HA, Girgis MD. Acute pancreatitis: a review. JAMA. 2021;325(4):382–90.
Brown LA, Hore TA, Phillips AR, Windsor JA, Petrov MS. A systematic review of the extra-pancreatic infectious complications in acute pancreatitis. Pancreatology. 2014;14(6):436–43.
Kylänpää ML, Repo H, Puolakkainen PA. Inflammation and immunosuppression in severe acute pancreatitis. World J Gastroenterol. 2010;16(23):2867–72.
Dellinger EP, Forsmark CE, Layer P, et al. Determinant-based classification of acute pancreatitis severity: an international multidisciplinary consultation. Ann Surg. 2012;256(6):875–80.
Wu D, Lu B, Xue HD, et al. Validation of Modified Determinant-Based Classification of severity for acute pancreatitis in a tertiary teaching hospital. Pancreatology. 2019;19(2):217–23.
Windsor J, de-Madaria E. Critical acute pancreatitis: A category with clinical relevance. Dig Liver Dis. 2021;53(12):1588–9.
Garret C, Canet E, Corvec S, et al. Impact of prior antibiotics on infected pancreatic necrosis microbiology in ICU patients: a retrospective cohort study. Ann Intensive Care. 2020;10(1):82.
Párniczky A, Lantos T, Tóth EM, et al. Antibiotic therapy in acute pancreatitis: from global overuse to evidence based recommendations. Pancreatology. 2019;19(4):488–99.
Shi N, Liu T, de la Iglesia-Garcia D, et al. Duration of organ failure impacts mortality in acute pancreatitis. Gut. 2020;69(3):604–5.
Ning C, Huang G, Shen D, et al. Adverse clinical outcomes associated with multidrug-resistant organisms in patients with infected pancreatic necrosis. Pancreatology. 2019;19(7):935–40.
Wu D, Ding J, Jia Y, et al. Predictors of mortality in acute pancreatitis complicated with multidrug-resistant Klebsiella pneumoniae infection. BMC Infect Dis. 2021;21(1):977.
Li X, Li L, Liu L, et al. Risk factors of multidrug resistant pathogens induced infection in severe acute pancreatitis. Shock. 2020;53(3):293–8.
Labricciosa FM, Sartelli M, Abbo LM, et al. Epidemiology and risk factors for isolation of multi-drug-resistant organisms in patients with complicated intra-abdominal infections. Surg Infect (Larchmt). 2018;19(3):264–72.
Fan N, Hu Y, Shen H, et al. Compositional and drug-resistance profiling of pathogens in patients with severe acute pancreatitis: a retrospective study. BMC Gastroenterol. 2020;20(1):405.
Crockett SD, Wani S, Gardner TB, et al. American Gastroenterological Association Institute guideline on initial management of acute pancreatitis. Gastroenterology. 2018;154(4):1096–101.
Wu D, Chen C, Liu T, et al. Epidemiology, susceptibility, and risk factors associated with mortality in carbapenem-resistant gram-negative bacterial infections among abdominal solid organ transplant recipients: a retrospective cohort study. Infect Dis Ther. 2021;10(1):559–73.
Walker AS, White IR, Turner RM, et al. Personalised randomised controlled trial designs-a new paradigm to define optimal treatments for carbapenem-resistant infections. Lancet Infect Dis. 2021;21(6):e175–81.
Chen S, Shi J, Chen M, et al. Characteristics of and risk factors for biliary pathogen infection in patients with acute pancreatitis. BMC Microbiol. 2021;21(1):269.
Boxhoorn L, van Dijk SM, van Grinsven J, et al. Immediate versus postponed intervention for infected necrotizing pancreatitis. N Engl J Med. 2021;385(15):1372–81.
Singer M, Deutschman CS, Seymour CW, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016;315(8):801–10.
Mustafic S, Brkic S, Prnjavorac B, et al. Diagnostic and prognostic value of procalcitonin in patients with sepsis. Med Glas (Zenica). 2018;15(2):93–100.
Wolbrink DRJ, Kolwijck E, Ten Oever J, et al. Management of infected pancreatic necrosis in the intensive care unit: a narrative review. Clin Microbiol Infect. 2020;26(1):18–25.
Schmidt PN, Roug S, Hansen EF, Knudsen JD, Novovic S. Spectrum of microorganisms in infected walled-off pancreatic necrosis - impact on organ failure and mortality. Pancreatology. 2014;14(6):444–9.
Liu J, Huang L, Luo M, Xia X. Bacterial translocation in acute pancreatitis. Crit Rev Microbiol. 2019;45(5–6):539–47.
Wu D, Huang Y, Ding J, Jia Y, Liu H, Xiao J, Peng J. Impact of carbapenem-resistant Acinetobacter baumannii infections on acute pancreatitis patients. Pancreatology. 2022;22(2):194–9.
Ning C, Zhu S, Wei Q, et al. Candidemia indicates poor outcome in patients with infected pancreatic necrosis. Mycoses. 2021;64(6):684–90.
Maguire C, Agrawal D, Daley MJ, Douglass E, Rose DT. Rethinking carbapenems: a pharmacokinetic approach for antimicrobial selection in infected necrotizing pancreatitis. Ann Pharmacother. 2021;55(7):902–13.
Acknowledgements
We thank Prof. Junxia Yan for her help in verifying the statistical analysis in our study.
Funding
This work and the journal’s Rapid Service Fee were supported by Fundamental Research Funds for the Central Universities of Central South University (Grant No. 2021zzts0347), Hunan Provincial Innovation Foundation For Postgraduate (Grant No. CX20210357), China Scholarship Council, and National Natural Science Foundation of China (Grant No. 81670589 and No. 82170661).
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
Jie Peng conceived and designed the study; Di Wu, Yilin Huang, Ge Qin, Huanmiao Liu and Jie Xiao collected and cleaned the data; Di Wu analyzed the data, interpreted the results and wrote the first draft of the manuscript; Yilin Huang, Ge Qin, Huanmiao Liu and Jie Xiao interpreted the results; all authors critically revised the manuscript and gave final approval for publication.
Disclosures
Di Wu, Yilin Huang, Ge Qin, Huanmiao Liu, Jie Xiao and Jie Peng have nothing to disclose.
Compliance with Ethics Guidelines
Informed consents and the need for direct patient enrollment were waived from all the patients due to retrospective nature. Ethical approvals of this retrospective cohort study were granted by Institutional Review Board of Xiangya Hospital (NO. 202202038) and Third Xiangya Hospital (No. 22028).
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Wu, D., Huang, Y., Xiao, J. et al. Risk Factors for Mortality Among Critical Acute Pancreatitis Patients with Carbapenem-Resistant Organism Infections and Drug Resistance of Causative Pathogens. Infect Dis Ther 11, 1089–1101 (2022). https://doi.org/10.1007/s40121-022-00624-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40121-022-00624-w