Abstract
Introduction
This study aimed to determine if tocilizumab treatment for coronavirus disease 2019 (COVID-19) increases bacteremia and suppresses fever and inflammatory reactants.
Methods
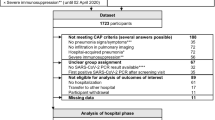
In this single-center, retrospective, observational study, all patients with COVID-19 admitted to our emergency intensive care unit from March 2020 to August 2021 were categorized into tocilizumab-treated and tocilizumab-naïve groups, and the incidence of bacteremia and other factors between the two groups were compared. Patients with bacteremia were further classified into tocilizumab-treated and tocilizumab-naïve groups to determine if fever and inflammatory reactants were suppressed.
Results
Overall, 144 patients were included in the study, 51 of whom received tocilizumab, which was administered on the day of admission. Further, of the 24 (16.7%) patients with bacteremia, 13 were in the tocilizumab-treated group. Results revealed a significant difference in the C-reactive protein level (p < 0.001) at the onset of bacteremia between the tocilizumab-treated group [median 0.42 mg/dL (0.27–0.44 mg/dL)] and the tocilizumab-naïve group [7.48 mg/dL (4.56–13.9 mg/dL)]. The median number of days from admission to onset of bacteremia was not significantly different between the tocilizumab-treated group [10 days (9–12 days)] and the tocilizumab-naïve group [9 days (7.5–11 days)] (p = 0.48). There was no significant difference in fever between the groups. Multivariate logistic analysis showed that tocilizumab treatment did not affect the probability of bacteremia.
Conclusion
Treatment of patients with COVID-19 with tocilizumab does not increase the risk of bacteremia. Tocilizumab suppresses C-reactive protein levels but not fever. Therefore, careful monitoring of fever can reduce the risk of missed bacteremia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Tocilizumab has been reported to reduce COVID-19 mortality. |
However, some studies have indicated tocilizumab, an IL-6 inhibitor, to increase susceptibility to bacteremia through inhibition of inflammatory responses. |
Thus, this study aimed to investigate the incidence of bacteremia between patients with COVID-19 treated and untreated with tocilizumab. |
What was learned from the study? |
We found that treatment with tocilizumab did not increase the risk of bacteremia in patients with COVID-19. |
As tocilizumab reduces C-reactive protein levels through anti-inflammatory effects, but not fever, monitoring for fever would aid in early detection of bacteremia. |
Introduction
The coronavirus disease 2019 (COVID-19) broke out in late 2019 in China, causing a global pandemic. Pro-inflammatory cytokines, including interleukin-6 (IL-6), have been linked to severe and high mortality cases of COVID-19. Blocking inflammatory pathways may prevent disease progression [1]. IL-6 plays an important role in systemic and local inflammation and is often associated with acute-phase reactions such as fever and changes in the level of the acute-phase protein, C-reactive protein (CRP). Tocilizumab is a humanized monoclonal antibody against the IL-6 receptor (IL-6R). Tocilizumab interferes with the action of cytokines by binding to both membrane-bound and soluble forms of human IL-6R, thereby inhibiting the binding of the native cytokine to its receptor. Tocilizumab was found to reduce COVID-19 mortality in previous studies [2,3,4,5]. Prior studies have shown that administration of IL-6 inhibitors may be associated with an increased risk of secondary infections [6, 7], while others have found no such association [8]. A meta-analysis of 10 observational studies in patients with COVID-19 showed no association between tocilizumab and increased frequency of secondary infections [9].
Moreover, IL-6 inhibitors have anti-inflammatory effects, and suppress fever and the level of acute-phase proteins, such as CRP. This may delay the diagnosis of infection by masking the signs and symptoms of acute inflammation [10, 11].
Therefore, we conducted a retrospective observational study to determine whether tocilizumab increases the frequency of bacteremia as a secondary infection in patients with COVID-19 and whether its anti-inflammatory action suppresses fever and CRP levels at the onset of bacteremia.
Methods
This retrospective case–control study was conducted at the Hyogo College of Medicine, a tertiary university hospital in Japan.
Patients
All patients with COVID-19 admitted to the emergency intensive care unit (ICU) of our hospital from March 2020 to August 2021 were included in the study. The preferred treatment of COVID-19 has changed in a short period of time. Almost all patients have been treated with steroids; patients treated with high-flow nasal cannulas and ventilators were not treated with tocilizumab prior to 2021 but have been treated with tocilizumab since early 2021. Tocilizumab was administered at 8 mg/kg for 2 days. All patients with COVID-19 included in the study were grouped into the tocilizumab-treated group or the tocilizumab-naïve group.
Data Collection
The following information was extracted from the electronic medical records: age, sex, body mass index (BMI), use of steroids, tocilizumab, and venovenous extracorporeal membrane oxygenation (VV-ECMO), rates of tracheostomy, intubation, and bacteremia, number of days from admission to bacteremia, type of causative organism, indication for obtaining blood culture, CRP levels, white blood cell count, temperature at the onset of bacteremia, and death.
Outcomes
The primary outcome is tocilizumab increases the risk of bacteremia. The secondary outcomes are tocilizumab (1) suppresses fever and (2) suppresses CRP levels.
Statistical Analysis
Statistical analysis was performed using EZR [12] (Saitama Medical Center, Jichi Medical School). The Mann–Whitney U test was performed on continuous variables, which were expressed as medians (interquartile range). χ2 tests and Fisher’s exact test were performed on the nominal variables, which were expressed as N (%). Multivariate logistic analysis was performed with tocilizumab administration, tracheostomy status, ECMO status, and intubation status as independent variables, and bacteremia and death as dependent variables.
Next, we compared tocilizumab-treated and tocilizumab-naïve patients who presented with bacteremia. In any one of the several sets of blood samples collected on the same day, detection of any of the following organisms was defined as contamination: coagulase-negative Staphylococcus, Propionibacterium acnes, Micrococcus, viridans group streptococci, Corynebacterium, Bacillus, or Clostridium perfringens [13]. In all analyses, the significance level was defined as a p value of less than 0.05. No missing data were found.
Ethical Considerations
The study was conducted in accordance with the Helsinki Declaration of 1964 and its later amendments. The collection of anonymized data for this study was approved by the Ethics Committee of Hyogo Medical College (registration number 202111-060). Because of the retrospective nature of this study, informed consent was not required. The reporting of this study complies with the STROBE statement.
Results
All Patients with COVID-19 and Tocilizumab Treatment
We analyzed 144 patients with COVID-19 admitted to our emergency ICU between March 2020 and August 2021 (Table 1). The median age of the patients with COVID-19 was 66.5, and 103 patients were male. The mean BMI was 24.2 [interquartile range (IQR), 21.6–27.3]. Steroids were used in 129 patients (89.6%); VV-ECMO was performed in 9 patients (6.3%). Tracheostomy was performed in 24 patients (16.7%). Intubation was performed in 62 patients (43.1%). There were 51 patients (35.4%) in the tocilizumab-treated group. There were no significant differences in the age, sex, BMI, steroid administration, diabetes mellitus, asthma, chronic obstructive pulmonary disease, or smoking history between the tocilizumab-treated and tocilizumab-naïve groups. There were significant differences in the use of VV-ECMO (p = 0.01) and the rates of tracheostomy (p = 0.02) and intubation (p < 0.001).
Bacteremia was observed in 13 patients (25.5%) in the tocilizumab-treated group and 11 patients (11.8%) in the tocilizumab-naïve group. Univariate logistic analysis [odds ratio (OR) 2.55, 95% confidence interval (CI) 1.05–6.21, p = 0.04] showed that tocilizumab was associated with an increased probability of bacteremia. Multivariate analysis was performed because of the selection of unbalanced variables as independent variables. However, multivariate logistic analysis with VV-ECMO, tracheostomy, and intubation as confounders showed that tocilizumab treatment was not an independent factor associated with bacteremia (OR 1.01, 95% CI 0.37–3.02, p = 0.99). There were no significant differences in mortality between the two groups.
Tocilizumab Treatment in Patients with COVID-19 and Bacteremia
There were 24 cases of bacteremia (16.7%). Table 2 shows the comparison of tocilizumab-treated and tocilizumab-naïve groups who had bacteremia, of which 13 (54.2%) were in the tocilizumab group. There were no significant differences in BMI, tracheostomy, intubation, chronic obstructive pulmonary disease, diabetes mellitus, smoking history, or steroid administration between the tocilizumab-treated and tocilizumab-naïve groups. There was a significant difference in age (p < 0.01) and VV-ECMO placement (p = 0.04) in the tocilizumab-treated group. The most common indication for performing blood culture was fever in 15 cases (62.5%), followed by hypotension in three cases (12.5%), increased inflammatory response in two cases (8.3%), and reticulocytosis in two cases (8.3%). There was no significant difference in indications for performing blood cultures between the tocilizumab-treated and tocilizumab-naïve groups (Table 3).
There was a significant difference (p < 0.001) in CRP at the onset of bacteremia between the tocilizumab-treated group [median 0.42 mg/dL (interquartile range 0.27–0.44 mg/dL)] and the tocilizumab-naïve group [7.48 mg/dL (4.56–13.9 mg/dL)]. There were no significant differences in white blood cell count, fever, or mortality rates between the groups. The median number of days from admission to onset of bacteremia was not significantly different between the tocilizumab-treated group [10 days (9–12 days)] and the tocilizumab-naïve group [9 days (7.5–11 days)] (p = 0.48).
The most common bacteria detected were methicillin-resistant Staphylococcus aureus in five cases (20.8%), followed by Enterobacter cloacae in four cases (16.7%) and methicillin-sensitive S. aureus in three cases (12.5%). E. cloacae was significantly more common in the tocilizumab-naïve group (p = 0.03) than in the tocilizumab-treated group. There were no significant differences in the detection of other organisms (Table 4).
Discussion
Several studies have reported on bacteremia in patients with COVID-19 [14,15,16]; however, this is the first study to compare the incidence of bacteremia between patients with COVID-19 who were treated with tocilizumab and those who were not. According to the results, tocilizumab is not an independent factor related to bacteremia in patients with COVID-19. This was similar to the results of a study of tocilizumab for rheumatoid arthritis in Japan [17].
Moreover, we found that tocilizumab administration may significantly reduce the CRP levels in patients with COVID-19 and bacteremia. This result was similar to the results reported so far [10, 11, 18, 19, 20]. Interestingly, however, fever was not suppressed, which could be due to the involvement of neurotransmitters since cytokines are not the only triggers of inflammation [21]. This was a different result than previously reported [10, 11].
There was no significant difference in the time from hospitalization to the onset of bacteremia between the tocilizumab-treated and tocilizumab-naïve groups, suggesting no delay in the diagnosis of bacteremia.
There are several limitations in this study. This was a retrospective observational study, and the difference in the severity of illness between the tocilizumab-treated and tocilizumab-naïve groups may have resulted in a differential risk of bacteremia. In addition, the study did not include the measurement of IL-6 levels and could not prove a correlation between IL-6 and tocilizumab. Finally, the data were limited to a single center and may not generally reflect the same observation across all patients of COVID-19 who developed bacteremia. Therefore, these limitations should be considered when interpreting the results.
Nevertheless, the results of this study allowed us to make the following inferences. IL-6 inhibitors have anti-inflammatory effects and suppress acute-phase reactants such as fever and CRP. This may delay the diagnosis of infection by masking the signs and symptoms of acute inflammation. Thus, tocilizumab administration in patients with COVID-19 would delay the diagnosis of infection. However, the results of this study showed no significant difference in the time from hospitalization to the onset of bacteremia between the tocilizumab-treated and tocilizumab-naïve groups. This may be because tocilizumab suppresses the CRP levels only and not fever, as demonstrated in this study. At our hospital, blood culture is performed if body temperature exceeds 38 °C. In other words, if fever is not suppressed, blood cultures would be taken in both tocilizumab-treated and tocilizumab-naïve groups, and the diagnosis of infection would have not been delayed.
In addition to monitoring for fever, physical examination, such as for the presence of reticulocutaneous plaques, is necessary to avoid delays in the diagnosis of bacteremia. The fact that our staff conducted thorough physical examinations of patients may have contributed to the prompt diagnosis.
On the basis of the results of this study, we should be alert to the physical findings, such as fever and reticulocutaneous plaques, and recommend blood cultures to be taken regularly.
Conclusion
Administration of tocilizumab to patients with COVID-19 does not increase the risk of bacteremia. Tocilizumab suppresses CRP levels but not fever. A thorough evaluation of fever and physical examination can eliminate delays in diagnosis.
References
Mehta P, McAuley DF, Brown M, et al. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395:1033–4. https://doi.org/10.1016/S0140-6736(20)30628-0.
WHO Rapid Evidence Appraisal for COVID-19 Therapies (REACT) Working Group, Shankar-Hari M, Vale CL, et al. Association between administration of IL-6 antagonists and mortality among patients hospitalized for COVID-19: a meta-analysis. JAMA. 2021;326:499–518. https://doi.org/10.1001/jama.2021.11330.
Ghosn L, Chaimani A, Evrenoglou T, et al. Interleukin-6 blocking agents for treating COVID-19: a living systematic review. Cochrane Database Syst Rev. 2021;3: CD013881. https://doi.org/10.1002/14651858.CD013881.
RECOVERY Collaborative Group. Tocilizumab in patients admitted to hospital with COVID-19 (RECOVERY): a randomised, controlled, open-label, platform trial. Lancet. 2021;397:1637–45. https://doi.org/10.1016/S0140-6736(21)00676-0.
REMAP-CAP Investigators, Gordon AC, Mouncey PR, et al. Interleukin-6 receptor antagonists in critically ill patients with Covid-19. N Engl J Med. 2021;384:1491–502. https://doi.org/10.1056/NEJMoa2100433.
Guaraldi G, Meschiari M, Cozzi-Lepri A, et al. Tocilizumab in patients with severe COVID-19: a retrospective cohort study. Lancet Rheumatol. 2020;2:e474–84. https://doi.org/10.1016/S2665-9913(20)30173-9.
Busani S, Bedini A, Biagioni E, et al. Two fatal cases of acute liver failure due to HSV-1 infection in COVID-19 patients following immunomodulatory therapies. Clin Infect Dis. 2021;73:e252–5. https://doi.org/10.1093/cid/ciaa1246.
Stone JH, Frigault MJ, Serling-Boyd NJ, et al. Efficacy of tocilizumab in patients hospitalized with Covid-19. N Engl J Med. 2020;383:2333–44. https://doi.org/10.1056/NEJMoa2028836.
Malgie J, Schoones JW, Pijls BG. Decreased mortality in coronavirus disease 2019 patients treated with tocilizumab: a rapid systematic review and meta-analysis of observational studies. Clin Infect Dis. 2021;72:e742–9. https://doi.org/10.1093/cid/ciaa1445.
Fujiwara H, Nishimoto N, Hamano Y, et al. Masked early symptoms of pneumonia in patients with rheumatoid arthritis during tocilizumab treatment: a report of two cases. Mod Rheumatol. 2009;19:64–8. https://doi.org/10.1007/s10165-008-0111-7.
Hirao M, Nampei A, Shi K, Yoshikawa H, Nishimoto N, Hashimoto J. Diagnostic features of mild cellulitis phlegmon in patients with rheumatoid arthritis treated with tocilizumab: a report of two cases. Mod Rheumatol. 2011;21:673–7. https://doi.org/10.1007/s10165-011-0459-y.
Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013;48:452–8. https://doi.org/10.1038/bmt.2012.244.
Hall KK, Lyman JA. Updated review of blood culture contamination. Clin Microbiol Rev. 2006;19:788–802. https://doi.org/10.1128/CMR.00062-05.
Giacobbe DR, Battaglini D, Ball L, et al. Bloodstream infections in critically ill patients with COVID-19. Eur J Clin Investig. 2020;50: e13319. https://doi.org/10.1111/eci.13319.
Bhatt PJ, Shiau S, Brunetti L, et al. Risk factors and outcomes of hospitalized patients with severe coronavirus disease 2019 (COVID-19) and secondary bloodstream infections: a multicenter case-control study. Clin Infect Dis. 2021;72:e995–1003. https://doi.org/10.1093/cid/ciaa1748.
Abelenda-Alonso G, Rombauts A, Gudiol C, et al. Immunomodulatory therapy, risk factors and outcomes of hospital-acquired bloodstream infection in patients with severe COVID-19 pneumonia: a Spanish case-control matched multicentre study (BACTCOVID). Clin Microbiol Infect. 2021;27:1685–92. https://doi.org/10.1016/j.cmi.2021.06.041.
Ryoko S, Soo-kyung C, Toshihiro N, et al. Head-to-head comparison of the safety of tocilizumab and tumor necrosis factor inhibitors in rheumatoid arthritis patients (RA) in clinical practice: results from the registry of Japanese RA patients on biologics for long-term safety (REAL) registry. Arthritis Res Ther. 2015;17:74.
Paola T, Simine P, Marco C, et al. Tocilizumab for the treatment of severe COVID-19 pneumonia with hyperinflammatory syndrome and acute respiratory failure: a single center study of 100 patients in Brescia, Italy. Autoimmun Rev. 2020;19:102568.
Tomasiewicz K, Piekarska A, Stempkowska-Rejek J, et al. Tocilizumab for patients with severe COVID-19: a retrospective, multi-center study. Expert Rev Anti-Infect Ther. 2021;19:93–100. https://doi.org/10.1080/14787210.2020.1800453.
Amin S, Rahim F, Bahadur S, Noor M, Mahmood A, Gul H. The effect of tocilizumab on inflammatory markers in survivors and non-survivors of severe COVID-19. J Coll Physicians Surg Pak. 2021;31:7–10. https://doi.org/10.29271/jcpsp.2021.Supp1.S7.
Gabay C, Kushner I. Acute-phase proteins and other systemic responses to inflammation. N Engl J Med. 1999;340:448–54. https://doi.org/10.1056/NEJM199902113400607.
Acknowledgements
We would like to thank Editage (https://www.editage.jp/) for English language editing.
Funding
No funding or sponsorship was received for this study or publication of this article. The journal’s Rapid Service Fee was funded by the authors.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
Masaatsu Kuwahara, Misa Kamigaito, and Jun-Ichi Hirata conceived and designed the experiments. Masaatsu Kuwahara analyzed the data. Masaatsu Kuwahara wrote the first draft, which was subsequently revised by all authors. All authors read and approved the final manuscript.
Disclosures
Masaatsu Kuwahara, Misa Kamigaito, Shou Nitta, Kana Hasegawa, Hiromoto Murakami, Tomoyuki Kobayashi, Kunihiro Shirai, Keisuke Kohama and Jun-Ichi Hirata confirm that they have no conflicts of interest to declare.
Compliance with Ethics Guidelines
The study was performed in accordance with the Helsinki Declaration of 1964, and its later amendments. The collection of anonymized data for this study was approved by the Ethics Committee of Hyogo Medical College (registration number 202111-060). Because of the retrospective nature of this study, informed consent was not required. The reporting of this study complies with the STROBE statement.
Data Availability
Data sharing will be considered under the form of collaborative projects. Proposals can be directed to the corresponding author.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Kuwahara, M., Kamigaito, M., Nitta, S. et al. Effect of Tocilizumab Treatment on Patients with Coronavirus Disease 2019 and Bacteremia: A Retrospective Cohort Study. Infect Dis Ther 11, 533–541 (2022). https://doi.org/10.1007/s40121-022-00592-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40121-022-00592-1