Abstract
Viruses cause a large number of diseases in humans, some of which are fatal, while others are highly debilitating. A majority of viral diseases attack infants and young children, while others strike people in their prime. Development of preventive measures against viral diseases is, therefore, of paramount importance. Vaccination is the most cost-effective medical intervention for preventing mortality and morbidity against infectious diseases. A number of effective and safe vaccines are currently available against several viral diseases of significant medical importance. Many of these manufactured in India, are at par with international standards and are affordable. For many other viral diseases, for which vaccines are currently not available, research is underway at various national laboratories, as well as in the private sector companies in India. The present overview highlights the various vaccine preventable viral diseases that are of special importance to India and aims to provide a glimpse of the various vaccines that are currently available, or are under development in India.
Similar content being viewed by others
Introduction
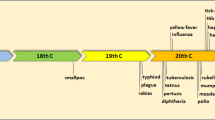
Vaccines are one of the most powerful and cost-effective health interventions to have been invented. Vaccines not only provide benefits at the level of the individual, but also to society at large. These are powerful as they not only prevent the primary disease, but also its complications or sequelae. Of the many medically important viral diseases prevalent in India, vaccines for only two, namely polio and measles, find a place in the Universal Immunization Programme (UIP) implemented by the Government of India. The other diseases that find a place in the UIP are of bacterial origin, namely, diphtheria, pertussis, tetanus, and childhood tuberculosis. All these UIP vaccines are available free of cost. The UIP is one of the largest programs of its kind in the world, in terms of the number of vaccine doses used and the number of people reached.
Undoubtedly, there are multiple issues that hinder the introduction of vaccines in the national programme, in spite of the availability of these vaccines. One of the major hindrances is cost, while others include programmatic and logistic issues, as well as the absence of disease-burden data in certain cases. While for many viral diseases total eradication is impossible due to their zoonotic nature, but for diseases like polio and measles the story is different. These two childhood viral diseases can be totally eradicated since human beings are the only host. What is required is a concerted and sustained global effort, with active public participation and co-operation, as was the case when smallpox was eradicated from the planet Earth.
India’s Strengths in Vaccine Production Capacity
India has a strong presence in the global vaccine scenario. Currently there are at least 13 major vaccine manufacturers in the country, with the number steadily increasing. India is a major importer as well as exporter of vaccines [1], with the Indian market for vaccines being valued at over USD 260 million [2]. India is a major supplier of vaccines to the United Nations Children’s Fund (UNICEF), which meets 40% of the global vaccine demand for routine childhood immunization programs in approximately 100 developing countries [3].
Development of biologicals such as vaccines goes hand-in-hand with other endeavors such as development of drugs and diagnostics. India has been able to contribute to all-round development in the health sector since it has an excellent R&D infrastructure, both in the public as well as the private sectors. Since independence, it has established top-class research institutes, medical colleges and hospitals. It has excellent drug testing laboratories, bio-safety labs, clinical trial centers, clinical research organizations (CRO) and other world-class facilities. The major R&D facilities in the public sector include Indian Immunologicals Ltd., Bharat Immunologicals & Biologicals Corp. Ltd., Haffkine Bio-Pharmaceutical Corp. Ltd., and the Central Research Institute (Kasauli). Their counterparts in the private sector include Serum Institute of India Ltd., Bharat Biotech International Ltd., Shantha Biotech, and Panacea Biotec Ltd. A new vaccine production plant has been completed at Dholka (Gujarat) by CPL Biologicals (a joint venture between Cadila Pharmaceuticals Ltd. and Novavax Inc., USA). The plant will have the capacity to manufacture 60 million doses of seasonal and pandemic (H1N1) flu vaccines annually [4]. Pune-based Serum Institute of India makes one out of every two vaccines produced in the world. Interestingly, Serum Institute of India was the first Indian company to be approached by the World Health Organization (WHO) to develop and manufacture the pandemic influenza vaccine. The institute launched its intranasal H1N1 vaccine (NASOVAC™) in July 2010 [5]. Panacea Biotec (New Delhi) has been playing a major role in the polio eradication programme by supplying over 6 billion doses of oral polio vaccine (OPV) to the Government of India and UNICEF [6]. From the South, Shantha Biotech’s Shanvac-B was the first Indian Hepatitis B vaccine to be pre-qualified by WHO for global distribution through the UN agencies. With Shantha’s Hepatitis B vaccine priced at just one-tenth of the imported vaccine, along with five other Indian companies entering the market, India has the cheapest Hepatitis B vaccine in the world [7]. Moreover, with the recent efforts of the Government of India, the Central Research Institute (Kasauli), Pasteur Institute of India (Coonoor), and the BCG Vaccine Laboratory (Guindy) have been enabled to resume vaccine production [8]. Hence, this is indeed an exciting time for vaccine production in India.
The present overview aims to highlight the major viral diseases where vaccines are either available in India or are under clinical or pre-clinical development in the country. It provides a bird’s eye view of the epidemiology, clinical features, current diagnostic and treatment modalities, as well as preventive measures, with special stress on vaccination. Table 1 provides some of the key details of the viral vaccines produced in India.
Arboviral Diseases Relevant to India
Arboviral (arthropod-borne viral) diseases constitute a major category of viral diseases that are transmitted by arthropods (e.g. mosquitoes, sandflies, or ticks). The importance accorded to this group of viral diseases stems from the fact that India has a significantly high density of mosquito population and a wide distribution of various mosquito species. Globally, more than 130 arboviruses are known to cause human diseases and some of these have a significant presence in India. Most arboviruses of public health importance belong to one of the three virus genuses: Flavivirus, Alphavirus, and Bunyavirus. In the Indian context, Japanese encephalitis virus (JEV) and Dengue virus (DENV) are two important Flaviviruses, whereas Chikungunya virus (CHIKV) is an important Alphavirus. Although the epidemiology of each of these diseases is unique, there is a certain degree of similarity that underlies all these diseases, particularly with reference to socio-economic, ecological and environmental factors that substantially contribute to the emergence, spread and sustenance of these diseases in nature [9].
Japanese Encephalitis Virus (JEV): Leading Cause of “Brain Fever” in Children
JEV is a Flavivirus that is spread to humans and animals by Culicine mosquitoes. The virion particles are spherical (~45 nm diameter), enveloped and possess a single-stranded, positive-sense, non-segmented RNA genome of approximately 11 kb length. The genome codes for 10 viral proteins (VP); three structural (capsid, pre-membrane/membrane, and envelope), and seven non-structural (NS1, NS2a, NS2b, NS3, NS4a, NS4b, NS5). The virus is responsible for causing Japanese encephalitis (JE), which is the most important form of viral encephalitis globally [10]. JE originated in Japan in the late 1800s, and has since spread over vast regions of South and South-East Asia, where approximately 3 billion people are at risk of contracting JE [11]. Needless to say that JE is a major public health problem in the region, accounting for ~50,000 cases and ~10,000 fatalities. This is a very conservative figure that may merely be indicating the proverbial tip-of-the-iceberg. In India, JE was first reported in 1955 from Vellore (formerly North Arcot district), Tamil Nadu, with a total of ~65 cases being reported between 1955 and 1966 from the area [12]. The first major outbreak occurred in 1973 in Burdwan and Bankura districts of West Bengal, with ~700 cases and 300 deaths [13]. Over the years JE epidemics have been reported from most parts of India and it has become endemic in several districts. There are no comprehensive figures on JE disease burden in India but it constitutes a substantial proportion of the total global burden.
JEV is maintained in nature by means of a zoonotic cycle involving Culicine mosquitoes (the vectors), pigs (the amplifying hosts) and ardeid birds (vertebrate reservoir). Humans act as the so called dead-end hosts, since infection with JEV usually does not produce sufficiently high titers of viremia for further propagation of the virus. JE, being a zoonosis, cannot be totally eradicated, but can be effectively kept in check by prophylactic vaccination of susceptible human populations. Vaccination becomes all the more important for controlling JE, since there is currently no effective treatment available, coupled with the fact that vector control measures are not totally effective. A mouse brain-derived, formalin-inactivated JE vaccine was produced by Central Research Institute (Kasauli) till about a couple of years ago. The vaccine was largely effective although there were concerns relating to its safety. Besides, the vaccine was produced in only limited quantities and prices were high. As the vaccine production facilities of the century-old Central Research Institute (Kasauli) did not comply with the internationally accepted cGMP guidelines, JE vaccine production was halted in 2008 [14]. However, there are a couple of JE vaccines that are in the advanced stages of development [15]. The front runners are IXIARO® (IC51), a purified inactivated vaccine (PIV) developed by Intercell (Austria) [16], and IMOJEV® a chimeric vaccine by Sanofi Pasteur [17] employing the Yellow fever virus 17D (YFV17D) ChimeriVax Technology platform. These two vaccines have proven themselves to be exemplary throughout pre-clinical and clinical development, with reference to safety and efficacy, the two cardinal properties of a “good” vaccine. Intercell’s Indian partner is Biological E, who will be manufacturing and marketing IXIARO® in India.
The Indian government is currently importing SA 14-14-2, a primary hamster kidney (PHK) cell-cultured, live-attenuated JE vaccine, from the Chengdu Institute of Biological Products (China). While this vaccine is safe, efficacious, and also cheap, it has not been taken up by the international community due to the PHK cell substrate used in its preparation. It will be interesting to see if the government adopts a change in its JE vaccination policy, once IXIARO® becomes available in the Indian market. The most important factor that will affect the decision-making process will definitely be the cost, because the Intercell vaccine is likely to be much costlier than the Chinese vaccine. However, this is unlikely to be a hindrance for IXIARO®’s commercial viability as Intercell’s primary target is the tourism market, since tourists from the West increasingly prefer to travel to exotic destinations that are inevitably JE endemic. Hence, efforts to develop safe and effective indigenous JE vaccines that are likely to be cheaper still continue. Our laboratory at the National Institute of Immunology has been engaged in this endeavor for the past several years. We have utilized conventional vaccine development strategies such as cell culture of virus followed by formalin-inactivation, as well as newer approaches involving recombinant DNA techniques. A PIV [18] has been developed using an Indian strain (P20778) of JEV grown in Vero cells, the technology for which has been transferred to Panacea Biotec for commercial development. A JEV DNA vaccine candidate has been evaluated in non-human primates with limited success [19], while an adenovirus 5 (Ad5)-vectored JEV vaccine candidate has shown promising results in mice [20]. Due to the widespread presence of Ad5 neutralizing antibodies in the human population and the recent disappointing outcome of the Ad5 based HIV vaccine trial [21] efforts are on to use novel adenoviral vectors for engineering recombinant JE vaccine.
Dengue Virus (DENV): A Flavivirus of Global Public Health Importance
DENV is a Flavivirus transmitted to humans by Aedes mosquitoes. The virion structure and the genome organization are similar to that of JEV. The virus is responsible for dengue fever (DENF), and its life-threatening complications, namely, dengue hemorrhagic fever (DHF) and dengue shock syndrome (DSS). These diseases are caused by four, related but antigenically distinct, DENVs (DENV 1–4). With over 2.5 billion people at risk of contracting dengue, and 50–100 million individuals being infected annually, this is undoubtedly a serious global public health problem [22].
DENV is transmitted primarily by Aedes aegypti, although Aedes albopictus has also been implicated. DENV is more dangerous than other arboviruses from a transmission-dynamics standpoint, because the viremia in humans is sufficiently high for further propagation of the virus. Hence, unlike JEV infections, humans do not act as dead-end-hosts in case of DENV infections, and a vertebrate reservoir/amplifying host is not required for maintenance of the virus in nature. For example, in an urban setting, DENV life-cycle can easily be maintained between humans and mosquitoes.
A major risk factor for the occurrence of dengue complications is the existence of sub-neutralizing levels of circulating antibodies to a heterologous DENV strain that may have been acquired in utero or from mosquito bites, giving rise to antibody dependent enhancement (ADE) [23]. It is believed that the phenomenon of ADE arises when the sub-neutralizing antibodies become complexed with heterotypic DENV from a secondary infection, as a result of which they are taken up more efficiently by the Fc receptor-bearing monocytes and macrophages [24].
Tackling complications of DEN such as DHF and DSS is a medical emergency, and requires immediate hospitalization in order to save the patients, who are very often school-going children [25]. As currently there is no specific antiviral treatment for DEN, management of complications is supportive, involving fluid replacement, in order to counteract the plasma leakage observed in Grade III/IV DHF and DSS [26]. Moreover, even implementation of supportive care is hindered by the absence of a low-cost rapid diagnostic test (RDT) having a sufficiently high specificity and sensitivity that can accurately predict disease severity [27].
DEN can be prevented by vaccination of susceptible human populations, and efforts in this direction have been on globally for over three decades, albeit without much success. The Indian effort to develop a dengue vaccine by the International Center for Genetic Engineering and Biotechnology (ICGEB) has utilized an adenovirus-vectored approach to develop a tetravalent DENV vaccine candidate. Here, the genes encoding the domain III of the envelope (E) protein (EDIII) of the respective DENV strains have been stitched together to create the tetravalent gene (EDIII-T) cassette that was inserted into a replication-defective Ad5 vector. This vaccine candidate was evaluated in mice, where cell-mediated immune responses as well as virus-neutralizing antibodies were generated [28]. Again, this vaccine construct suffers from the limitations of Ad5 vectors described above. Efforts are currently ongoing at ICGEB to produce EDIII-T in Pichia expression system.
Chikungunya Virus (CHIKV): An Important Re-Emerging Arbovirus in India
CHIKV is an Alphavirus that is spread to humans by Aedes mosquitoes. The Alphaviruses are small, enveloped viruses (~50–70 nm diameter), that possess a single-stranded, positive-sense RNA genome of approximately 12 kb length. The genome is organized into two distinct regions; the 5′ two-thirds encoding the non-structural proteins (NSP) (NSP1, NSP2, NSP3, NSP4) and the 3′ one-third encoding the four major structural proteins, including the capsid protein and three envelope proteins (E1, E2, E3) [29].
Chikungunya fever (CHIKF) is clinically characterized by a triad of symptoms, including fever, rash and arthralgia. Clinical diagnosis of CHIKF is complicated by the fact that many clinical features overlap with those of DENF. Hence, efforts need to be directed towards development of CHIKV-specific diagnostics that can be used in field situations, especially during epidemics. CHIKF has no specific treatment. Treatment is purely symptomatic and supportive.
No commercial CHIK vaccine is currently available anywhere in the world, although efforts are on to develop tissue culture derived or virus-like particle (VLP) based vaccines, following the recent re-emergence of the virus in many parts of Asia, including the explosive outbreak in India in 2006 that amounted to a staggering ~1.4 million cases [30, 31]. Efforts are also on in India to develop Vero cell cultured, inactivated CHIKV vaccine. Scientists at the Defence Research and Development Establishment (DRDE), Gwalior have developed a Vero cell adapted, formalin-inactivated CHIKV vaccine candidate using an Indian strain of CHIKV (DRDE 06) isolated from a patient in Hyderabad during the 2006 outbreak. Immunization of Swiss albino mice with the inactivated vaccine generated high titers of CHIKV neutralizing antibodies. However, the efficacy of the vaccine formulation was tested by means of in vitro and in vivo neutralization tests, and direct challenge experiments in an animal model with a lethal/clinical dose of the virus was not carried out [32].
Chandipura Virus (CHPV): An Important Emerging Arbovirus in India
CHPV is a rhabdovirus with a non-segmented, single-stranded, negative-sense RNA genome. The rhabdoviruses derive their name from the Greek word rhabdo meaning rod-shaped. These viruses exhibit a typical bullet-shaped morphology and the most common member is the rabies virus, which will be discussed later.
The CHPV virions consist of a ribonucleoprotein (RNP) particle core containing a non-segmented single-stranded genomic RNA wrapped around by a nucleocapsid protein (N). The viral RNA dependent RNA polymerase (RdRp) is composed of a large protein (L), the catalytic subunit and a phosphorylated form of phosphoprotein (P) that acts as a transcriptional activator. Components of the viral RdRp, L and P are packaged within the mature virion and remain associated with the core RNP particle. The mature virus is covered by an outer lipoprotein envelope (E). The glycoprotein (G) protrudes externally from the outer membrane, while the matrix protein (M) lies within the bilayer structure of the membrane. G is the only spike protein of CHPV that enables virion adsorption, assembly and budding. M helps to tether the core RNP particle to the membrane [33].
CHPV was first isolated in 1965 from two adult patients suffering from febrile illness in a village called Chandipura, in the Nagpur region (Maharashtra)—hence the name Chandipura virus [34]. CHPV was subsequently isolated from a child suffering from acute encephalitis in Raipur (Chhattisgarh) [35]. Although the epidemic potential of the virus was initially underestimated, CHPV outbreaks in two consecutive years, in Andhra Pradesh in 2003 [36] and Gujarat in 2004 [37], followed by another in Nagpur division in 2007 [38] highlighted CHPV as an emerging pathogen that demanded its due share of attention from the arbovirus community.
CHPV is spread by sandflies (Phlebotomus argentipes), as demonstrated by virus isolation from the vector in Aurangabad [39], as well as detection of viral RNA in Karimnagar [40]. More recently, the susceptibility and transmission potential of Phlebotomus argentipes for CHPV has been conclusively demonstrated experimentally under laboratory conditions [41].
The main clinical features of CHPV encephalitis (CHPE) include fever, seizures, altered sensorium and headache, often accompanied by GI tract symptoms. Shock, rash and hemorrhagic symptoms are present less often. The major complication is encephalitis. There is no specific treatment for CHPE, the mainstay being supportive hospital-based care, coupled with good nursing. CHPE can be held in check by prophylactic vaccination of susceptible populations, along with vector control measures. Currently there is no CHPE vaccine available commercially. The only candidate CHPV vaccine under development in India is by the National Institute of Virology [42]. This vaccine candidate is based on the glycoprotein (G) gene of CHPV, which has been expressed as a recombinant protein using a Baculovirus expression system. Immunogenicity studies in mice have shown promising results, particularly the fact that an intracerebral (i.c.) challenge using a homologous CHPV led to 90% protection.
Other Vaccine Preventable Viral Diseases Relevant to India
Besides the arboviral diseases, there are quite a few viral diseases in India that are essentially endemic, and pose a major public health problem. Many of these vaccine preventable diseases (VPD) are also a major global problem, particularly in developing countries. A brief overview of some of these VPDs of special concern for India is given below.
Rotavirus: A Major Cause of Infant Diarrhea in India
In India, diarrheal diseases are responsible for approximately 13% of deaths in infants and children <5 years of age, amounting to an estimated 334,000 deaths annually [43]. Rotavirus (RV) is responsible for a substantial proportion (~40%) of these deaths, estimated at ~125,000 annually, with up to 884,000 hospitalizations, and 2 million outpatient visits annually in children <5 years of age [44].
RVs belong to the Family Reoviridae, and are classified into seven groups (A–G), of which groups A, B and C are known to infect humans. Group A RVs are the leading cause of diarrhea in infants and children, while Groups B and C are primarily responsible for sporadic cases. RVs are non-enveloped, double-stranded RNA viruses having a segmented genome, divided into 11 segments. The segmented genome allows for extensive recombination among various strains, resulting in tremendous diversity in the RV strains. Each genome segment codes for a VP or NSP. The viral capsid encloses the RNA genome, and is composed of three VPs, namely VP4, VP6 and VP7. While VP6 bears antigenic determinants responsible for group and sub-group specificities, VP4 (P-protease-sensitive) and VP7 (G-glycoprotein) determine the P- and G-types of the various RV strains that form the basis of classification of the various serotypes [45]. Around 48 G- and P-genotypes (20 G; 28 P) have been reported [46], of which the most common strains that infect children worldwide are G1, G2, G3, G4, G9, P[4], P[6], and P[8] [47, 48].
RV disease is characterized by watery diarrhea, often accompanied by fever, vomiting and nausea, leading to rapid dehydration that can be fatal in the absence of medical intervention. There is no specific treatment for RV infection. The main aim of therapy is to maintain the electrolyte balance and reversing the dehydration by administering oral rehydration solution (ORS). However, the costs incurred for the management of RV disease is quite staggering. The sum-total of the direct medical and direct non-medical costs borne by the Indian public health system for tackling RV diarrhea cases annually is approximately USD 41–72 million, and coupled with the disease burden, makes a compelling case for introducing prophylactic measures such as vaccination [44].
Two US FDA-approved RV vaccines, RotaTeq® (Merck Sharp & Dohme) and Rotarix® (GlaxoSmithKline) are currently available internationally. RotaTeq® is a pentavalent live oral vaccine made from human-bovine reassortant RV containing G1, G2, G3, G4 and P1A[8]. Rotarix® is a monovalent live oral vaccine made from human RV strain G1P[8]. However, these vaccines are expensive in the Indian context and feasibility of incorporating these in the Indian childhood immunization program would very much depend on their cost-effective availability [49, 50]. Efforts are also on to develop cheaper indigenous RV vaccines. One RV vaccine candidate, based on the strain 116E, having the genotype G9,P[11], originally isolated from a neonate at the All India Institute of Medical Sciences (AIIMS), New Delhi, has recently completed a dose-escalation randomized, double-blind, placebo-controlled trial in infants in New Delhi. The study indicated that the vaccine candidate elicits a robust immune response following three doses [51]. Phase III clinical trials of this vaccine candidate are currently in progress. If this indigenous vaccine candidate is successful, it will be an effective yet cheaper alternative to the already licensed RV vaccines. Another candidate, based on the UK human-bovine reassortant developed at the National Institutes of Health (NIH), Bethesda, USA [52, 53] has been licensed out to the Serum Institute of India (Pune) and Shantha Biotech (Hyderabad) for further development.
Rabies: An Age-Old Scourge that is Still a Major Problem in Modern-Day India
Rabies is one of the oldest zoonotic viral diseases to have plagued India since Vedic times, spanning well over 3,000 years. Although the rabies virus (RABV) is borne by a large number of terrestrial as well as flying mammals, dogs have been and still are the major reservoirs of the virus in India [54]. An estimated 55,000 deaths occur annually due to rabies, of which 20,000 are from India, accounting for approximately 36% of all global deaths. The annual incidence of rabies in India is 2 per 100,000 population [55]. Two distinct clinical syndromes are recognized in humans—furious (encephalitic) and paralytic. The furious form is characterized by fever, distal paresthesias, fasciculation, altered sensorium, pleocytosis in the cerebrospinal fluid, accompanied by rapid progression of symptoms, and is comparatively easier to diagnose. The paralytic form poses more difficulty in diagnosis, as it exhibits similar symptoms to Guillain-Barré syndrome, and in the absence of a history of dog bite, the clinical picture is similar to a psychiatric syndrome [56]. The incubation period for RABV, unlike other viral infections, can be quite long, ranging from <1 week to >1 year, but typically 1–3 months. However, it should be noted that once symptoms of the disease develop, rabies is fatal to both animals and humans. Moreover, since no specific test for RABV is currently available, in the absence of the classical rabies-specific signs, such as hydrophobia or aerophobia, clinical diagnosis is very difficult [55].
RABV belongs to the Family Rhabdoviridae. The virions have a helical symmetry, 180 nm in length and 75 nm in diameter. These are enveloped viruses, having a single-stranded, negative-sense RNA genome, in which the genetic information is tightly packaged as a RNP complex. The genome encodes the nucleoprotein (N), phosphoprotein (P), matrix protein (M), glycoprotein (G), and the RdRp (L) [57].
Rabies can be very effectively prevented through vaccination. The vaccine can be given pre-exposure, as well as post-exposure. Pre-exposure prophylaxis is recommended for anyone who is at increased risk of exposure to RABV such as laboratory workers, while post-exposure prophylaxis is recommended for affected individuals. There are essentially two types of vaccines for human use, the nerve tissue vaccine (NTV) and the cell culture vaccines (CCV). The NTV is produced by growing RABV in sheep brain, and in India, it is called Semple vaccine, after the British Director of the Central Research Institute (Kasauli) who developed the technique at the turn of the last century. The Semple vaccine requires a large number of painful intramuscular (i.m.) injections. Moreover, since it contains myelin protein, there is a possibility of occurrence of allergic encephalomyelitis (AEM) in certain vaccine recipients. The WHO has recommended that the NTV be replaced with the more efficacious and safer CCV [58]. Following a Supreme Court order in 2005, the production of the Semple vaccine has been banned, and is gradually being phased out from the Indian health system. Two WHO approved CCVs have been available in India for over two decades. These include a purified chick embryo cell (PCEC) vaccine (Rabipur®) produced by Chiron Vaccines (India) and marketed by Sanofi Aventis (India). The other is a purified Vero cell rabies vaccine (PVRV), manufactured by Sanofi Pasteur (France), and marketed by Ranbaxy (India) under the brand name Verorab®. Considering the high price of these vaccines, rabies CCVs have been developed indigenously. Indirab™, a Vero cell-based rabies vaccine manufactured by Bharat Biotech International Ltd., (Hyderabad) has been found to be safe and immunogenic in humans [59]. Abhayrab™ is another PVRV available from Indian Immunologicals Ltd. (Hyderabad). Rabies vaccines have also been prepared using human diploid cells, the international standard being the Merieux inactivated rabies vaccine (MIRV), manufactured by Sanofi Pasteur (Lyon, France). In 1999, Serum Institute of India (Pune) indigenously developed an adsorbed human diploid cell rabies vaccine (Rabivax®) using the Pitman-Moore RABV strain grown on human diploid cells, followed by inactivation with BPL. This vaccine was found to be immunogenic and safe for rabies prophylaxis in humans [60]. A purified duck embryo vaccine (PDEV) against rabies, is manufactured by Berna Biotech (Switzerland) and available internationally as Lyssavac N for over two decades. Following technology transfer, the same vaccine is manufactured in India by Zydus Cadila Health Care Ltd. (Ahmedabad), and marketed as Vaxirab®. An open label, randomized phase IV comparative clinical trial indicated that Vaxirab® was as safe, tolerable and immunogenic as Rabipur® and Verorab® the two WHO approved vaccines, and could be used as an alternative vaccine for post-exposure prophylaxis of rabies [61]. A multicentric study has also indicated the safety and efficacy of this indigenously manufactured PDEV for post-exposure prophylaxis [62]. For the purpose of immunotherapy, anti-RABV immunoglobulins raised in horses are also available in the Indian market. For example, AbhayRIG is available from Indian Immunologicals Ltd. (Hyderabad), while Equirab is available from Bharat Serums and Vaccines Ltd. (Thane).
From a vaccine delivery standpoint, it has been established that the intradermal (i.d.) route is much more cost-effective than the conventional i.m. route, and can amount to over 3-fold reduction in costs [63]. Besides the vaccines discussed so far, which are already available in the Indian market, at least two indigenous anti-rabies DNA vaccine candidates are currently under development [64, 65]. Moreover, microparticle-based delivery systems are also being explored in India [66].
It is evident that a multi-pronged approach will be required to reduce human rabies cases in India. Some of the strategies that need to be adopted include (i) compulsory licensing and vaccination of pet dogs, (ii) stringent dog birth control programmes for controlling the population of stray street dogs, (iii) the issue of incorporation of pre-exposure rabies vaccine in childhood immunization programme needs to be considered, (iv) sustained Information, Education and Communication (IEC) activities, and (v) declaration of rabies as a notifiable disease. Hence, prevention of human rabies in the long-run will require an all-inclusive, co-ordinated, community-based effort, with active participation of the general public, non-governmental organizations (NGOs), as well as government staff from the veterinary and public health wings of the health system.
Hepatitis B: A Vaccine with a Programmatic Issue in India
Hepatitis B is a global public health problem, with approximately 2 billion people i.e. almost a third of the world’s population being infected with the virus. At least a million deaths occur annually that are related to Hepatitis B virus (HBV) infection. India has intermediate endemicity, with Hepatitis B surface antigen (HBsAg) prevalence between 2 and 7%. There are over 40 million HBsAg carriers in India. With over 100,000 deaths annually, India accounts for over 10% of global deaths due to HBV infections [67].
HBV is a DNA virus belonging to Family Hepadnaviridae. The virion particle is enveloped by a lipid covering that encloses the nucleocapsid core, which in turn encloses the viral DNA and a DNA polymerase. HBV replicates in the hepatocytes of humans and higher primates. The HBsAg is a lipoprotein of the viral envelope and has a neutralizing epitope “a” [68]. A large body of evidence suggests that the majority of infants of e-antigen positive HBsAg carrier mothers are very much likely to become chronically infected unless vaccinated at birth [69]. Thus, mother-to-child transmission at the time of birth is a very common mode of transmission of HBV [70]. Amongst adults, people at high risk of HBV infections include patients with sexually transmitted infections (STIs), homosexuals, promiscuous heterosexuals, commercial sex workers, injection-drug users, household contacts of chronically infected HBV patients, chronic renal failure patients requiring regular hemodialysis, patients requiring blood products, HIV+ patients, and healthcare workers where HBV exposure is an occupational hazard.
A number of strategies, primarily based on vaccination, need to be adopted to block the transmission of HBV. These include (i) universal vaccination at birth, (ii) compulsory screening of all pregnant women for HBsAg, (iii) post-exposure immunotherapy of infants born to HBsAg+ women, (iv) catch-up vaccination for children and adolescents, and (v) vaccination of “at-risk” adults.
In the case of HBV, HBsAg is the protective antigen. Current Hepatitis B vaccines contain HBsAg produced by recombinant DNA technology, and are available as monovalent formulations or in fixed-dose combinations with other vaccines. Some of the other vaccines used in the combos include diphtheria-tetanus–pertussis (DTP), Haemophilus influenzae type b (Hib), Hepatitis A, and inactivated polio vaccine (IPV). The immunogenicity and safety profile of these combos are comparable to those when the vaccines are administered individually [71–73]. However, for immunization at birth, only the monovalent HBV vaccine is recommended, which should be administered within 24 h of birth [68]. This particular requirement has been a steep challenge for Hepatitis B vaccination in India. With >60% of births still taking place at home, often in remote, inaccessible, poverty-stricken areas, reaching the newborn within this short time period has been the major hindrance in introducing the vaccine in the UIP.
Recombinant Hepatitis B vaccine is currently manufactured indigenously by a number of leading Indian companies, including Serum Institute of India, Shantha Biotech, Panacea Biotec and others. Thus, availability of the vaccine at a suitable price for supplying to the public health system should not be a problem. What will be required is out-of-the-box thinking to troubleshoot the programmatic issues in order to expedite the Hepatitis B vaccination programme, which has already commenced in project-mode since 2002 in designated cities in India [67].
Human Papilloma Virus: Need for Indigenously Developed Affordable Vaccines
Human papilloma virus (HPV), belonging to the Family Papovaviridae has non-enveloped virion particles (~55 nm diameter) with double stranded DNA as the genetic material. HPV is an epitheliotropic virus of humans that causes proliferative lesions in epidermal or mucosal epithelia. Of the 150 or so types of HPV that have been identified, at least 30 types infect the genital mucosa in humans, and hence, are sexually transmitted. These HPV types are categorized as low- and high-risk types. The former are responsible for genital warts, as well as recurrent respiratory papillomatosis (RRP), while the latter are responsible for cervical cancer. The most common low-risk HPV types that cause up to 90% of all genital warts are HPV-6 and HPV-11 [74], while the most common high-risk HPV types that account for ~70% of cervical cancers are HPV-16 and HPV-18 [75]. HPV infections are one of the most common STIs amongst women. Approximately 80% of sexually active women and men become infected with HPV at some point in their lives [76]. Most infections are transient, and are usually cleared by the immune response, and usually do not present any clinical symptoms [77]. However, persistent infection can lead to cervical cancer. In India, there are an estimated 132,000 new cases of cervical cancer and 74,000 deaths annually [78].
Currently two licensed vaccines, Gardasil® (Merck Sharp & Dohme) and Cervarix® (GSK) are available internationally. Both are VLP-based vaccines, the former being quadrivalent (covering HPV types 6, 11, 16, 18), while the latter being bivalent (covering HPV types 16, 18). Although, the Indian Academy of Pediatrics Committee on Immunization (IAPCOI) recommends the HPV vaccine to all female children aged between 10 and 12 years of age who can afford the vaccine [79], access to these vaccines will, for the moment, be restricted to the economically well-off class, who ironically, require the vaccine least of all. Accessibility to these life-saving vaccines has been hindered by their exorbitant cost, being the most expensive vaccines produced so far [80]. The retail price in India for the complete schedule of Gardasil® is Rs. 6,900 and that for Cervarix® is Rs. 7,800, which clearly indicates that this vaccine is still essentially out-of-reach of the general Indian public. Hence, there is a strong argument for the development of indigenous HPV vaccines that would be more affordable, and hence, more accessible.
Development of HPV vaccines indigenously that can be priced competitively for greater accessibility to the target population is technically and economically feasible. In retrospect, it may be remembered that when the HBV vaccine was introduced in the early 1980s, it was priced at ~USD 50–80 per dose, one of the costliest vaccines at the time. However, within a decade, companies from developing countries like India developed and introduced the vaccine at USD 3 per dose, which due to the ensuing competition, came down to less than 30 cents per dose by 2001 [81]. This same approach should be feasible for the HPV vaccine. Four leading Indian companies, namely Shantha Biotech, Serum Institute of India, Bharat Biotech and Indian Immunologicals are currently developing HPV vaccines that could be much cheaper than the current vaccines [82]. Shantha has even indicated that its vaccine could be initially priced at just USD 15 [83]. Besides these companies, two others, namely, Virchow Biotech and Gennova Biopharmaceuticals are also developing HPV vaccines with support from the Department of Biotechnology (DBT), Government of India, under the Biotechnology Industry Partnership Programme (BIPP) [84]. All these efforts are still in their infancy and it’s going to be some time before an Indian HPV vaccine becomes available.
Measles, Mumps, Rubella (MMR): Important but Often Neglected in India
Measles is an acute viral illness in infants and children that is a major public health problem in developing countries like India, and is one of the single-most important causes of childhood mortality. The prodromal stage of the disease exhibits non-specific symptoms as for most viral infections, and is characterized by fever, malaise, conjunctivitis and respiratory symptoms such as coryza and coughing. A characteristic clinical feature of measles is the appearance of rash, which is erythematous and maculopapular in nature, and begins in the head, then spreads to the trunk and finally to the limbs over a span of 3–4 days. Two to 3 days before the onset of the rash, Koplik’s spots, the pathognomonic enanthem of measles, appear in the mucosa of the buccal cavity. This disease is highly contagious and spreads by droplet transmission. The most common complications of measles are otitis media, pneumonia, diarrhea and convulsions. More rare complications include encephalitis and sub-acute sclerosing pan-encephalitis (SSPE) [85].
The measles virus (MV) is a member of the Family Paramyxoviridae, with ~16 kb single-stranded RNA of negative polarity as genome. The genome encodes six proteins, all of which are structural proteins. Three proteins, nucleoprotein (N), phosphoprotein (P), and large protein (L), are complexed with viral RNA to form the nucleocapsid. The other three proteins, matrix protein (M), hemagglutinin (H), and fusion protein (F), participate in the formation of the viral envelope [85].
Measles is a VPD and it was incorporated into the UIP in 1985. The commercial live-attenuated measles vaccine available from the Serum Institute of India (M-VAC™) uses the Edmonston-Zagreb strain of MV, propagated in human diploid cells. In spite of the availability of a cheap measles vaccine, India’s measles vaccination programme faces many problems and challenges. Some of these include the unfinished polio eradication agenda, lack of surveillance for VPD, as well as financial and manpower constraints. With the traditionally low routine immunization coverage in India, it has been estimated that of the 22.7 million infants who missed their first dose of measles vaccine through routine immunization services in 2008, 7.63 million were from India alone, accounting for ~33.6% of the global figures [86]. India is the only country in the world not to have introduced a second dose of measles vaccine in spite of documented evidence of the efficacy of two doses of the vaccine in reducing measles related mortality [87]. Moreover, India has not followed the recommendations made by the WHO Strategic Advisory Group of Experts (SAGE) on immunization in November 2008 for administering two doses of the measles vaccine [88]. In recent times, death of four infants shortly after administration of measles vaccine, possibly due to human error has led to public distrust in vaccination efforts [89]. There is an urgent need to initiate the second-dose measles vaccination in India, as well as catch-up vaccination for those children who are yet to receive the first dose of the measles vaccine.
The mumps virus is also a member of the Family Paramyxoviridae. Mumps is spread by droplet infection and mainly affects school-going children. Mumps, also known as “Parotitis”, is clinically characterized by swelling and pain in the parotid salivary glands. Orchitis occurs in about one in four males who develop mumps after puberty. Oophoritis is the corresponding symptom in adolescent females. The incubation period is ~18 days [90]. Mumps is also a VPD, and vaccines against it are available in India.
Rubella virus, an enveloped RNA virus, is the sole member of the Genus Rubivirus in the Family Togaviridae. Rubella, also known as “German measles”, is also a VPD that is transmitted by droplet infection. The disease tends to affect older children, adolescents, and young adults, and is spread less readily than measles. The clinical course of the disease is generally mild, with complete recovery being the rule. The disease is of particular relevance if it occurs in pregnant women within the first 4 months of pregnancy, as it can cause congenital abnormalities in the fetus, if the women had not received prior vaccination against rubella [90].
The Serum Institute of India manufactures a live-attenuated rubella vaccine (R-VAC™) prepared by propagating the Wistar RA 27/3 rubella virus strain in human diploid cells. A combined Measles–Mumps–Rubella (MMR) vaccine that provides protection against mumps in addition to measles and rubella is also manufactured by Serum Institute of India (TRESIVAC™). The live-attenuated L-Zagreb strain of mumps virus propagated on chick embryo fibroblast cells is used in the combined vaccine preparation. The MMR vaccine available from Indian Immunologicals (Abhay-Vac 3) is manufactured with the same virus strains in exactly the same fashion as that of the Serum Institute vaccine. The MMR vaccine exhibits >95% seroconversion against measles and rubella, and 90% seroconversion against mumps in infants 9–15 months of age [91]. Moreover, the immunity generated is long-lasting, with significant levels of seropositivity even after 6 years post vaccination [92]. The Indian Academy of Pediatrics (IAP) recommends two doses of MMR vaccine, one at 15–18 months of age, and the other at 5 years of age [93]. Due to the severity of complications arising from measles in adults; recent outbreaks of mumps including in India [94]; as well as rubella seropositivity in infants suspected to be infected in utero [95], as well as in pregnant women [96], it has been recommended by the Advisory Committee on Immunization Practices (ACIP) that all adults born after 1957 should receive at least two doses of MMR vaccine, unless otherwise contraindicated [97]. Efforts should be directed at vaccinating susceptible adolescents and adults, especially against rubella, particularly women of child bearing age since the virus can cause congenital defects if contracted during pregnancy.
Influenza: Need for Surveillance and Pandemic Preparedness
Acute respiratory infections (ARI) are a major killer of children in developing countries, responsible for ~1.9 million deaths annually, with 20% of these deaths occurring in India alone [98, 99]. Influenza is the most frequent cause of ARI requiring medical attention because it affects all age groups and because of its recurrence [100]. Influenza virus (INFV) belongs to the Family Orthomyxoviridae where enveloped virions have a segmented negative-stranded RNA genome. Influenza viruses are classified into three genera, namely, A, B and C, of which the first two are known to cause human disease. INFV are typed on the basis of two surface proteins—hemagglutinin (HA) and neuraminidase (NA). Influenza A and B viruses possess eight different RNA segments that code for 10 and 11 different proteins respectively. Influenza C viruses lack an NA gene and thus have only seven RNAs, which code for at least nine different polypeptides [101].
In India, seasonal influenza cases are influenced by climatic fluctuations. Although there is no defined seasonal pattern, it has been generally observed that in northern India cases occur during winter, while in the south cases occur during the monsoon season. Viral ARI in India is caused primarily by influenza A and B viruses, parainfluenza virus and respiratory syncytial virus (RSV) [102, 103]. The burden of seasonal influenza in India appears to be low [104], although further cross-sectional studies as well as active surveillance are required. However, influenza does account for a large number of absentees at schools, colleges and offices annually. A trivalent inactivated vaccine (TIV) against seasonal influenza is available in India from companies like Chiron, Solvay, Lupin, GSK and Sanofi Pasteur. The 2010–2011 trivalent vaccine contains A/California/7/2009 (H1N1)-like, A/Perth/16/2009 (H3N2)-like, and B/Brisbane/60/2008-like antigens. We believe that currently there are no sufficient reasons to initiate vaccination against seasonal influenza in India and the seasonal influenza should be prevented by implementation of simple public health interventions such as hand washing with soap and inculcating habits for improving general respiratory hygiene. However, surveillance systems should be in place so that vaccination options may be kept open for special cases, such as mass human congregations that occur during religious occasions like the Maha-Kumbh Mela, Ganga Sagar Mela and the Muslim pilgrimage of Hajj [105].
It should be kept in mind that influenza viruses can mutate rapidly (antigenic shift) as opposed to the slower changes (antigenic drift) that occur over a longer period of time. Moreover, the genes of INFV from different species can recombine and undergo reassortment, giving rise to INFV with pandemic potential, such as the influenza A (H1N1) virus that caused the 2009 influenza (swine flu) pandemic [106]. The virus can also “jump” the species barrier, as occurred during the avian influenza outbreaks, when a bird-specific influenza A (H5N1) virus infected humans. This bird flu virus originated in China, but rapidly spread across three continents—Asia, Africa and Europe, causing outbreaks in over 30 countries, including India [107]. Threats like bird flu are very real and can only be checked by implementing a surveillance system that can closely monitor viruses circulating in birds, especially those that have a direct bearing on humans, such as poultry. There is really no justification for developing a bird flu vaccine due to its limited human-to-human transmission potential. Moreover, human cases can be treated with antivirals such as Oseltamivir and Amantadine, while outbreaks in poultry can be controlled by effective culling activities. However, for pandemic influenza A (H1N1) virus, a vaccine is essential. Currently, India has its own swine flu vaccine manufactured by the Serum Institute of India (Pune). This is a live-attenuated vaccine (NASOVAC™) that uses the California isolate (A/17/California/2009/38) of human H1N1, which is propagated in specific pathogen free (SPF) embryonated hen eggs, followed by lyophilization, and is formulated for intranasal administration. Serum Institute of India is also developing other immunogens and monoclonal antibodies against pandemic H1N1 with funding from DBT under BIPP [84]. Moreover, Panacea Biotec is also developing a H1N1 pandemic influenza vaccine with funding from the same source. Bharat Biotech also has a pandemic influenza vaccine in its product pipeline [108]. We are of the opinion that the pandemic H1N1 influenza (swine flu) vaccine should be reserved for individuals at high-risk of contracting infection, and for the management of outbreak situations.
Polio: An Unfinished Agenda
Poliomyelitis, commonly referred to as polio, is an age-old viral disease that has affected humanity since time immemorial. In fact, Egyptian stone carvings suggest that polio could have existed since pre-biblical times; as far back as 1580 B.C. Polio is an acute illness that follows invasion through the gastro-intestinal (GI) tract by one of the three serotypes of polio virus. Polio viruses are enteroviruses that belong to the Family Picornaviridae, since they are very small (pico) and possess an RNA genome. As indicated above, wild polio viruses (WPV) are of three types—WPV1, WPV2 and WPV3 [109]. The virus replicates in the gut, and then invades the bloodstream. It has a high degree of tropism for nervous tissue, and once the peripheral nerves become infected, the virus reaches the central nervous system (CNS) by retrograde axonal transport. Infection might be clinically asymptomatic, but when symptoms appear, they may range from fever to aseptic meningitis or paralysis. Infection is spread by feco-oral route, as well as from pharyngeal secretions from infected individuals. Over-crowding and poor sanitation facilitate the rapid spread of polio, a major reason for this disease being endemic in developing countries.
Polio is a VPD, and vaccines against the disease have been developed over half a century ago. The IPV was developed by Jonas Salk in 1955, while the live-attenuated OPV was developed by Albert Sabin in 1961. Vaccination efforts have essentially eradicated the disease from the western hemisphere. The Global Polio Eradication Initiative (GPEI) a public–private partnership (established in 1988) led by ~200 national governments and spearheaded by the WHO, CDC, UNICEF and Rotary International is the driving force behind all efforts directed at global polio eradication. Largely due to this huge global effort, polio is on the verge of eradication. Currently, four countries (Afghanistan, India, Nigeria, Pakistan) are polio endemic, while four others (all in Africa) are having re-established polio transmission. There are 13 other countries that have reported imported poliovirus cases [110]. Due to sustained vaccination efforts, WPV2 has been eradicated from the wild, the last case being detected in India in 1999. In this final stage of the eradication process, the goal is to wipe out the remaining WPV1 and 3. Both these types circulate in endemic areas and are highly infectious, and both cause paralysis. While WPV1 is more widespread, WPV3 is more localized in northern India, northern Nigeria, Pakistan and Afghanistan. In order to tackle this problem, a bivalent OPV (bOPV) has been developed. A randomized, double-blind, controlled trial indicated the superiority of bOPV compared to trivalent OPV (tOPV), and non-inferiority compared with monovalent OPV1 (mOPV1) and monovalent OPV3 (mOPV3) [111]. The bOPV was first introduced in Afghanistan in December 2009, when 2.8 million children <5 years old received the vaccine. This vaccine was introduced in India in January 2010, following which polio cases decreased dramatically. As of April 20, 2011, the historically polio-prone State of Uttar Pradesh has not reported a single case of polio for over a year, the last case being reported on April 21, 2010, from Ferozabad. Only a single paralytic-polio case has been reported so far this year (WPV1 infection, reported on January 13, 2011) from Howrah district in West Bengal. This has set the West Bengal outbreak response team into action, which has initiated Sub-National Immunization Days (SNID) since April 24, 2011, in an effort to check any further polio cases. In fact, India is currently faring better than some other countries, for example, the Democratic Republic of Congo (36 cases; all WPV1), Pakistan (28 cases; all WPV1), and Chad (20 cases; 18 WPV1; 2 WPV3), which have reported comparatively much higher number of polio cases so far this year [112].
India currently manufactures all types of OPV, and has contributed immensely to the polio eradication programme by supplying vaccines to international organizations like UNICEF. Panacea Biotec, India’s leading manufacturer of polio vaccines manufactures the entire range—mOPV1, mOPV2 (discontinued), mOPV3, tOPV (phased out), and bOPV. Haffkine Bio-Pharmaceutical Corporation Ltd. (HBPCL) manufactures mOPV1, tOPV (phased out), and bOPV. Bharat Biotech manufactures tOPV (BIOPOLIO™) (phased out). Needless to say, these OPVs are of international quality, and except for Bharat Biotech’s tOPV, all are WHO prequalified vaccines [113].
It seems that the stage is all set for polio to be eradicated once and for all from the globe. However, extensive surveillance is required, for gathering evidence for any WPV that might be circulating in the environment, as well as for vaccine-associated paralytic polio (VAPP) cases, which appears to be an emerging problem—a by-product of the intensive polio vaccination campaigns over the years.
HIV/AIDS: An Ideal Vaccine Still a Long Way Off
The Acquired Immune Deficiency Syndrome (AIDS) pandemic, caused by the Human Immunodeficiency Virus (HIV) has ravaged the globe for nearly three decades, and is still showing no signs of abating. Currently, with over 33 million people living with HIV/AIDS worldwide, with over 7,000 becoming infected every day, this is undoubtedly one of the greatest human calamities caused by a virus in modern times. HIV belongs to the Family Retroviridae, where virions possess an enzyme called reverse transcriptase (RT). The enzyme causes reverse transcription of the viral genetic information contained in the RNA genome into DNA. This is unique in the sense that it goes against the general flow of genetic information (DNA → RNA → Protein) as per the Central Dogma. There are two types of HIV—HIV-1 and HIV-2, both of which cause human disease. HIV-1 is responsible for the global AIDS pandemic. HIV-2 also causes AIDS, but the progression is much slower, and is essentially limited to countries in West Africa and to Portugal [114].
With the discovery of HIV in the early 1980s, early optimism indicated that a vaccine would soon be developed. However, this initial optimism was dampened by continual setbacks faced over the years. Some of the major obstacles included the vast genetic variability of HIV, arising from the absence of a proof-reading mechanism in RT that allows mutations to happen rapidly during the replication cycle. Absence of a suitable animal model has also been a major hindrance in vaccine development efforts, with the chimpanzee model being far from ideal. Moreover, there are no clear correlates of protection, necessitating Phase III human clinical trials in order to establish the efficacy of a vaccine.
Three separate large-scale Phase III clinical trials (VAX 004, VAX 003, RV 144) have been conducted in a total of over 24,000 human volunteers, yet the vaccine candidates were unable to prevent HIV-1 infection [115–117]. The International AIDS Vaccine Initiative (IAVI), founded in 1996, is a global not-for-profit, public–private partnership that has been working to accelerate the development of a HIV/AIDS vaccine. IAVI currently supports five clinical trials of candidate AIDS vaccines and two trials of an intermittent pre-exposure prophylaxis (PrEP) regimen. In collaboration with the Indian Council of Medical Research (ICMR), IAVI is supporting a Phase I clinical trial to evaluate the safety and immunogenicity of a prime-boost regimen of two AIDS vaccine candidates, ADVAX and TBC-M4. Initial analyses of the data gathered in this trial suggest that the vaccine regimen is both safe and immunogenic [118].
In spite of sub-optimal results, the clinical trials have generated new knowledge that will be helpful in designing and developing new vaccine candidates. In fact, recent modeling studies indicate that if a HIV/AIDS vaccine (possessing 70% efficacy) could be developed by 2015, and administered to 40% of the population, it would reduce the annual number of new infections by 81% by 2030 [119]. However, with over three decades of sustained global efforts, it is now widely accepted that developing a HIV/AIDS vaccine is one of the most difficult challenges confronting bio-medical scientists today. But the quest goes on.
Concluding Remarks
Viral diseases have a major impact on the health of all Indians. With the burgeoning population, zoonotic niché that were previously undisturbed are increasingly being encroached by humans. As a consequence, many viral diseases that were previously unheard-of are emerging, while those that were quiescent for decades are re-emerging. Vaccines could confer protection against many of these emerging viral diseases. However, there are several key programmatic areas that need to be looked into and properly addressed, in order to ensure that vaccines become a reality. One of the areas that require attention is improving the understanding of disease burden through surveillance. Establishment of an integrated surveillance system across Asia, with various stakeholder countries contributing to its sustenance is the need of the hour. This will help in detecting diseases like Severe Acute Respiratory Syndrome (SARS) before they cause large outbreaks. India was lucky last time, with only one imported case of SARS. Next time, luck might not be on India’s side, since improvements in aviation can now send infected people to any part of the globe within 24 h. For surveillance to be sustainable, financial support needs to be garnered for the economically weaker countries. Moreover, dedicated advocacy is a must, in order to keep the topic of vaccine preventable viral diseases on the national, regional and international agendas.
However, we should simultaneously ask the question: A vaccine for every viral disease—is it practicable? We should do justice by trying to find a proper answer. Vaccines for all viral diseases are not feasible in a vast and diverse country like India. Disease burden is not clear for many viral diseases. Hence the need for disease burden studies. Resources should be properly utilized so that indigenous vaccine development efforts focus on viral diseases with a proven and established burden of disease. Many viruses mutate so rapidly that strain replacement occurs every year e.g. seasonal influenza. Here, India cannot afford to mimic the West by trying to introduce a seasonal influenza vaccine. Not only would this be financially impractical, but also a logistical nightmare. For viruses like HIV, for which vaccines are not available, and probably will not be for quite some time, efforts need to be focused in bringing about behavioral changes as an adjunct to therapeutic interventions. For diseases like Hepatitis B, for which cheap and effective vaccines are already available, the programmatic deadlock should be broken so that every newborn gets the vaccine. Other types of hepatitis, like Hepatitis A and E should be managed by implementation of simple public health measures such as hand-washing and improvements in sanitation. There is now renewed hope of treating Hepatitis C with a new potent oral HCV-protease inhibitor (Boceprevir). Moreover, there is a need for health education activities so that parents can make informed choices about vaccines for their children, some of which are not mandatory (Varicella vaccine), while others are highly expensive (HPV vaccine). Lastly, unfinished programmes like Polio eradication should be completed as soon as possible, and at the same time, the second dose measles vaccination initiative should be kick-started, so that it picks up momentum, in time to achieve the targets set in the Millennium Development Goals by 2015.
References
Madhavi Y (2005) Vaccine policy in India. PLoS Med 2:e127
Lohray BB (2003) Medical biotechnology in India. Adv Biochem Eng Biotechnol 85:215–281
Gogtay NJ, Dhingra MS, Yadav A, Chandwani H (2009) Vaccine policy, regulations and safety in India. Int J Risk Saf Med 21:23–30
Rand R (2010) Bethesda biotech focuses on personalized vaccines. BioWatch, June 25, 2010. http://www.gazette.net/stories/06252010/businew170825_32549.php. Accessed on 11 April 2011
Som N (2010) Serum Institute launches intra-nasal swine flu vaccine Nasovac in India. BioSpectrum (Asia Edition) July 15, 2010. http://www.biospectrumasia.com/content/150710IND13091.asp. Accessed on 14 April 2011
CyberMedia (2010) Bangalore loses India’s top biotech city tag. CyberMedia News June 17, 2010. http://www.ciol.com. Accessed 11 April 2011
Suresh N, Rao CS (2009) Profiles of four top biotech companies in India. Biotechnol J 4:295–300
UPA Government (2010) Report to the people 2009–2010 (presented by Prime Minister Manmohan Singh to mark the completion of the first year of the UPA Government’s second five-year term), May 7, 2010: http://pmindia.nic.in/english_report_01.06.10.pdf. Accessed on 14 April 2011
Morens DM, Folkers GK, Fauci AS (2004) The challenge of emerging and re-emerging infectious diseases. Nature 430:242–249
Bharati K, Vrati S (2009) Japanese encephalitis. In: Sharma SK, Singal RK, Agarwal AK (eds) Monograph on adult immunization the association of physicians of India. Jaypee Brothers Medical Publishers (P) Ltd., New Delhi, pp 104–110
Senior K (2008) Is Japanese encephalitis control achievable by 2013? Lancet Infect Dis 8:534
Carey DE, Myers RM, Pavri KM (1968) Japanese encephalitis studies in Vellore, South India. II. Antibody response of patients. Indian J Med Res 56:1319–1329
Chakravarty SK, Sarkar JK, Chakravarty MS, Mukherjee MK, Mukherjee KK, Das BC, Hati AK (1975) The first epidemic of Japanese encephalitis studied in India—virological studies. Indian J Med Res 63:77–82
Rajalakshmi TK (2008) Testing times. Frontline 25(7) March 29–April 11, 2008. http://www.hindu.com/fline/fl2507/stories/20080411250702500.htm. Accessed 8 May 2011
Halstead SB, Thomas SJ (2010) New vaccines for Japanese encephalitis. Curr Infect Dis Rep 12:174–180
Eder S, Dubischar-Kastner K, Firbas C, Jelinek T, Jilma B, Kaltenboeck A, Knappik M, Kollaritsch H, Kundi M, Paulke-Korinek M, Schuller E, Klade CS (2011) Long term immunity following a booster dose of the inactivated Japanese encephalitis vaccine IXIARO®, IC51. Vaccine 29:2607–2612
Appaiahgari MB, Vrati S (2010) IMOJEV®: a Yellow fever virus-based novel Japanese encephalitis vaccine. Expert Rev Vaccines 9:1371–1384
Appaiahgari MB, Vrati S (2004) Immunogenicity and protective efficacy in mice of a formaldehyde-inactivated Indian strain of Japanese encephalitis virus grown in Vero cells. Vaccine 22:3669–3675
Bharati K, Rani R, Vrati S (2009) Evaluation of Japanese encephalitis virus DNA vaccine candidates in rhesus monkeys [Macaca mulatta]. Vaccine 27:10–16
Appaiahgari MB, Saini M, Rauthan M, Jyoti, Vrati S (2006) Immunization with recombinant adenovirus synthesizing the secretory form of Japanese encephalitis virus envelope protein protects adenovirus-exposed mice against lethal encephalitis. Microb Infect 8:92–104
Robb ML (2008) Failure of Merck HIV vaccine: an uncertain step forward. Lancet 372:1857–1858
Halstead SB (2007) Dengue. Lancet 370:1644–1652
Mathew A, Rothman AL (2008) Understanding the contribution of cellular immunity to dengue disease pathogenesis. Immunol Rev 225:300–313
Halstead SB (2003) Neutralization and antibody dependent enhancement of dengue viruses. Adv Virus Res 60:421–467
Gubler DJ, Meltzer M (1999) Impact of dengue/dengue hemorrhagic fever on the developing world. Adv Virus Res 53:35–70
Lee IK, Lee WH, Yang KD, Liu JW (2010) Comparison of the effects of oral hydration and intravenous fluid replacement in adult patients with non-shock dengue hemorrhagic fever in Taiwan. Trans R Soc Trop Med Hyg 104:541–545
Julander JG, Perry ST, Shresta S (2011) Important advances in the field of anti-dengue virus research. Antivir Chem Chemother 21:105–116
Khanam S, Pilankatta R, Khanna N, Swaminathan S (2009) An adenovirus type 5 (AdV5) vector encoding an envelope domain III-based tetravalent antigen elicits immune responses against all four dengue viruses in the presence of prior AdV5 immunity. Vaccine 27:6011–6021
Gubler DJ, Roehrig JT (1998) Arboviruses (Togaviridae and Flaviviridae) (Chapter 29) In: Collier L, Balows A, Sussman M (eds) vo 1: Mahy BWJ, Collier L (eds) Virology: topley & wilson’s microbiology and microbial infections, 9th edn. Arnold, a Member of the Hodder Headline Group, London, Sydney, Auckland, 579–600
Mavalankar D, Shastri P, Raman P (2007) Chikungunya epidemic in India: a major public-health disaster. Lancet Infect Dis 7:306–307
Tandale BV, Santhe PS, Arankalle VA, Wadia RS, Kulkarni R, Shah SV, Shah SK, Sheth JK, Sudeep AB, Tripathy AS, Mishra AC (2009) Systemic involvements and fatalities during Chikungunya epidemic in India, 2006. J Clin Virol 46:145–149
Tiwari M, Parida M, Santosh SR, Khan M, Dash PK, Rao PVL (2009) Assessment of immunogenic potential of Vero adapted formalin inactivated vaccine derived from novel ECSA genotype of Chikungunya virus. Vaccine 27:2513–2522
Basak S, Mondal A, Polley S, Mukhopadhyay S, Chattopadhyay D (2007) Reviewing Chandipura: A vesiculovirus in human epidemics. Biosci Rep 27:275–298
Bhatt PN, Rodrigues FM (1967) Chandipura virus: A new arbovirus isolated in India from patients with febrile illness. Indian J Med Res 55:1295–1305
Rodrigues JJ, Singh PB, Dave DS, Prasan R, Ayachit V, Shaikh BH, Pavri KM (1983) Isolation of Chandipura virus from the blood in acute encephalopathy syndrome. Indian J Med Res 77:303–307
Rao BL, Basu A, Wairagkar NS, Gore MM, Arankalle VA, Thakare JP, Jadi RS, Rao KA, Mishra AC (2004) A large outbreak of acute encephalitis with high fatality rate in children in Andhra Pradesh, India, in 2003, associated with Chandipura virus. Lancet 364:869–874
Chadha MS, Arankalle VA, Jadi RS, Joshi MV, Thakare JP, Mahadev PVM, Mishra AC (2005) An outbreak of Chandipura virus encephalitis in the eastern districts of Gujarat state, India. Am J Trop Med Hyg 73:566–570
Gurav YK, Tandale BV, Jadi RS, Gunjikar RS, Tikute SS, Jamgaonkar AV, Khadse RK, Jalgaonkar SV, Arankalle VA, Mishra AC (2010) Chandipura virus encephalitis outbreak among children in Nagpur division, Maharashtra, 2007. Indian J Med Res 132:395–399
Dhanda V, Rodrigues FM, Ghosh SN (1970) Isolation of Chandipura virus from sand flies in Aurangabad. Indian J Med Res 58:179–180
Geevarghese G, Arankalle VA, Jadi R, Kanojia PC, Joshi MV, Mishra AC (2005) Detection of Chandipura virus from sand flies in the genus Sergentomyia (Diptera: Phlebotomidae) at Karimnagar District, Andhra Pradesh, India. J Med Entomol 42:495–496
Mavale MS, Fulmali PV, Ghodke YS, Mishra AC, Kanojia P, Geevarghese G (2007) Experimental transmission of Chandipura virus by Phlebotomus argentipes (Diptera: Psychodidae). Am J Trop Med Hyg 76:307–309
Venkateswarlu CH, Arankalle VA (2009) Recombinant glycoprotein based vaccine for Chandipura virus infection. Vaccine 27:2845–2850
Million Death Study Collaborators, Bassani DG, Kumar R, Awasthi S, Morris SK, Paul VK, Shet A, Ram U, Gaffey MF, Black RE, Jha P (2010) Causes of neonatal and child mortality in India: a nationally representative mortality survey. Lancet 376:1853–1860
Tate JE, Chitambar S, Esposito DH, Sarkar R, Gladstone B, Ramani S, Raghava MV, Sowmyanarayanan TV, Gandhe S, Arora R, Parashar UD, Kang G (2009) Disease and economic burden of rotavirus diarrhoea in India. Vaccine 275:F18–F24
Estes MK, Kapikian AZ (2007) Rotaviruses. In: Knipe DM, Howley PM, Griffin DE, Martin MA, Lamb RA, Roizman B, Straus SE (eds) Fields virology, 5th edn. Lippincott-Raven, Philadelphia, pp 1917–1974
Solberg OD, Hasing ME, Trueba G, Eisenberg JNS (2009) Characterization of novel VP7, VP4, and VP6 genotypes of a previously untypeable group A rotavirus. Virology 385:58–67
Gentsch JR, Laird AR, Bielfelt B, Griffin DD, Banyai K, Ramachandran M, Jain V, Cunliffe NA, Nakagomi O, Kirkwood CD, Fischer TK, Parashar UD, Bresee JS, Jiang B, Glass RI (2005) Serotype diversity and reassortment between human and animal rotavirus strains: implications for rotavirus vaccine programs. J Infect Dis 192:S146–S159
Santos N, Hoshino Y (2005) Global distribution of rotavirus serotypes/genotypes and its implication for the development and implementation of an effective rotavirus vaccine. Rev Med Virol 15:29–56
Rose J, Hawthorn RL, Watts B, Singer ME (2009) Public health impact and cost effectiveness of mass vaccination with live attenuated human rotavirus vaccine (RIX4414) in India: model based analysis. Br Med J 339:b3653
Esposito DH, Tate JE, Kang G, Parashar UD (2011) Projected impact and cost-effectiveness of a rotavirus vaccination program in India, 2008. Clin Infect Dis 52:171–177
Bhandari N, Sharma P, Taneja S, Kumar T, Rongsen-Chandolia T, Appaiahgari MB, Mishra A, Singh S, Vrati S, Rotavirus Vaccine Development Group (2009) A dose-escalation safety and immunogenicity study of live attenuated oral rotavirus vaccine 116E in infants: a randomized, double-blind, placebo-controlled trial. J Infect Dis 200:421–429
Clements-Mann ML, Makhene MK, Mrukowicz J, Wright PF, Hoshino Y, Midthun K, Sperber E, Karron R, Kapikian AZ (1999) Safety and immunogenicity of live attenuated human-bovine (UK) reassortant rotavirus vaccines with VP7-specificity for serotypes 1, 2, 3 or 4 in adults, children and infants. Vaccine 17:2715–2725
Clements-Mann ML, Dudas R, Hoshino Y, Nehring P, Sperber E, Wagner M, Stephens I, Karron R, Deforest A, Kapikian AZ (2001) Safety and immunogenicity of live attenuated quadrivalent human-bovine (UK) reassortant rotavirus vaccine administered with childhood vaccines to infants. Vaccine 19:4676–4684
Menezes R (2008) Rabies in India. Can Med Assoc J 178:564–566
World Health Organization (2010) Rabies vaccines: WHO position paper. Wkly Epidemiol Rec 85:309–320
Gadre G, Satishchandra P, Mahadevan A, Suja MS, Madhusudana SN, Sundaram C, Shankar SK (2010) Rabies viral encephalitis: clinical determinants in diagnosis with special reference to paralytic form. J Neurol Neurosurg Psychiatry 81:812–820
Finke S, Conzelmann KK (2005) Replication strategies of rabies virus. Virus Res 111:120–131
World Health Organization (2005) WHO expert consultation on rabies: first report. WHO Tech Rep Ser No. 931. World Health Organization, Geneva
Sampath G, Madhusudana SN, Sudarshan MK, Ashwathnarayana DH, Mahendra BJ, Ullas TP, Mohan K, Madhusudhan SK, Ravish HS (2010) Immunogenicity and safety of Indirab: a Vero cell based chromatographically purified human rabies vaccine. Vaccine 28:4086–4090
Sudarshan MK, Bhardwaj S, Mahendra BJ, Sharma H, Sanjay TV, Ashwathnarayana DH, Bilagumba G (2008) An immunogenicity, safety and post-marketing surveillance of a novel adsorbed human diploid cell rabies vaccine (Rabivax®) in Indian subjects. Hum Vaccin 4:275–279
Ashwathnarayana DH, Madhusudana SN, Sampath G, Sathpathy DM, Mankeshwar R, Ravish HHS, Ullas PT, Behra TR, Sudarshan MK, Gangaboraiah, Shamanna M (2010) A comparative study on the safety and immunogenicity of purified duck embryo vaccine (PDEV, Vaxirab) with purified chick embryo cell vaccine (PCEC, Rabipur) and purified vero cell rabies vaccine (PVRV, Verorab). Vaccine 28:148–151
Mahendra BJ, Madhusudana SN, Sampath G, Datta SS, Ashwathnarayana DH, Venkatesh GM, Sudarshan MK, Bilugumba G, Shamanna M (2010) Immunogenicity, safety and tolerance of a purified duck embryo vaccine (PDEV, VAXIRAB) for rabies post-exposure prophylaxis: results of a multicentric study in India. Hum Vaccin 6:721–724
Rahim A, Kuppuswamy K, Thomas B, Raphael L (2010) Intradermal cell culture rabies vaccine: a cost effective option in antirabies treatment. Indian J Community Med 35:443–444
Gupta PK, Dahiya SS, Kumar P, Rai A, Patel CL, Sonwane AA, Saini M (2009) Sindbis virus replicon-based DNA vaccine candidate encoding rabies virus glycoprotein elicits specific humoral and cellular immune response in dogs. Acta Virol 53:83–88
Kaur M, Saxena A, Rai A, Bhatnagar R (2010) Rabies DNA vaccine encoding lysosome-targeted glycoprotein supplemented with Emulsigen-D confers complete protection in preexposure and postexposure studies in BALB/c mice. FASEB J 24:173–183
Ramya R, Verma PC, Chaturvedi VK, Gupta PK, Pandey KD, Madhanmohan M, Kannaki TR, Sridevi R, Anukumar B (2009) Poly (lactide-co-glycolide) microspheres: a potent oral delivery system to elicit systemic immune response against inactivated rabies virus. Vaccine 27:2138–2143
World Health Organization (2011) Hepatitis B: introducing hepatitis b vaccine in Universal Immunization Programme in India—a brief scenario. WHO India, 2011. http://www.whoindia.org/en/section6%5Csection8.htm. Accessed 18 April 2011
World Health Organization (2009) Hepatitis B vaccines: WHO position paper. Wkly Epidemiol Rec 84:405–420
Beasley RP, Hwang LY, Lee GC, Lan CC, Roan CH, Huang FY, Chen CL (1983) Prevention of perinatally transmitted hepatitis B virus infections with hepatitis B virus infections with hepatitis B immune globulin and hepatitis B vaccine. Lancet 2:1099–1102
Wong VC, Ip HM, Reesink HW, Lelie PN, Reerink-Brongers EE, Yeung CY, Ma HK (1984) Prevention of the HBsAg carrier state in newborn infants of mothers who are chronic carriers of HBsAg and HBeAg by administration of hepatitis-B vaccine and hepatitis-B immunoglobulin. Double-blind randomised placebo-controlled study. Lancet 1:921–926
Bavdekar SB, Maiya PP, Subba Rao SD, Datta SK, Bock HL (2007) Immunogenicity and safety of combined diphtheria tetanus whole cell pertussis hepatitis B/Haemophilus influenzae type b vaccine in Indian infants. Indian Pediatr 44:505–510
Pichichero ME, Bernstein H, Blatter MM, Schuerman L, Cheuvart B, Holmes SJ, 085 Study Investigators (2007) Immunogenicity and safety of a combination diphtheria, tetanus toxoid, acellular pertussis, hepatitis B, and inactivated poliovirus vaccine coadministered with a 7-valent pneumococcal conjugate vaccine and a Haemophilus influenzae type b conjugate vaccine. J Pediatr 151:43–49
Heininger U, DTP-HBV-IPV-059 Study Group, DTP-HBV-IPV-096 Study Group, Sänger R, Jacquet JM, Schuerman L (2007) Booster immunization with a hexavalent diphtheria, tetanus, acellular pertussis, hepatitis B, inactivated poliovirus vaccine and Haemophilus influenzae type b conjugate combination vaccine in the second year of life: safety, immunogenicity and persistence of antibody responses. Vaccine 25:1055–1063
Shah KV, Howley PM (1990) Papillomavirus. In: Fields BN, Knipe DM, Chanock RM, Hirsch MS, Melnik TP, Roizman B (eds) Fields virology, 2nd edn. Raven Press Ltd., New York, pp 1651–1676
Bosch FX, Manos MM, Muñoz N, Sherman M, Jansen AM, Peto J, Schiffman MH, Moreno V, Kurman R, Shah KV (1995) Prevalence of human papillomavirus in cervical cancer: a worldwide perspective. International biological study on cervical cancer (IBSCC) Study Group. J Natl Cancer Inst 87:796–802
Koutsky LA, Galloway DA, Holmes KK (1997) Epidemiology of genital human papillomavirus infection. Am J Med 102:3–8
Ho GYF, Bierma R, Beardsley L, Chan CJ, Burk RD (1998) Natural history of cervicovaginal papillomavirus infection in young women. N Engl J Med 338:423–428
Parkin DM, Bray F, Ferlay J, Pisani P (2004) GLOBOCAN 2002: Cancer incidence, mortality and prevalence worldwide. IARC cancer base No. 5, version 2.0. IARC Press, Lyon
Indian Academy of Pediatrics Committee on Immunization (IAPCOI) (2008) Consensus recommendations on immunization, 2008. Indian Pediatr 45:635–648
CDC Vaccine Price List (2011) http://www.cdc.gov/vaccines/programs/vfc/cdc-vac-price-list.htm. Accessed 19 April 2011
Gacic-Dobo M, Mayers G, Birmingham M, Kane M, Hadler SC, Perilla MJ, Shaw FE, Goldstein ST, Mast EE, Margolis HS, Samandari T (2003) Global progress toward universal childhood hepatitis B vaccination, 2003. Morb Mortal Wkly Rep 52:868–870
Padmanabhan S, Amin T, Sampat B, Cook-Deegan R, Chandrasekharan S (2010) Intellectual property, technology transfer and manufacture of low-cost HPV vaccines in India. Nat Biotechnol 28:671–678
Sinha GP (2007) Shantha developing $15 cervical cancer vaccine. The Economic Times October 16, 2007. http://articles.economictimes.indiatimes.com/2007-10-16/news/27671464_1_cervical-cancer-vaccine-merck-s-gardasil-hpv-types. Accessed 19 April 2011
Biotechnology Industry Partnership Programme (BIPP), Department of Biotechnology, Government of India (2011) Products/processes under development through BIPP support. http://www.birapdbt.nic.in/uploads/Upload_Dec2010/Products-Processes_Under_Development_Through_BIPP_Support.pdf. Accessed 19 April 2011
Oxman MN (1997) Measles. In: Richman DD, Whitley RJ, Hayden FG (eds) Clinical virology, 1st edn. Churchill Livingstone, New York, pp 821–861
Dabbagh A, Gacic-Dobo M, Simons E, Featherstone D, Strebel P, Okwo-Bele JM, Hoekstra E, Chopra M, Uzicanin A, Cochi S (2009) Global measles mortality, 2000–2008. Morb Mortal Wkly Rep 58:1321–1326
van den Ent M, Gupta SK, Hoekstra E (2009) Two doses of measles vaccine reduce measles deaths. Indian Pediatr 46:933–938
World Health Organization (2009) Meeting of the immunization Strategic Advisory Group of Experts, November 2008—conclusions and recommendations. Wkly Epidemiol Rec 84:1–16
Amdekar YK, Singhal T (2008) Measles vaccine deaths—the IAP-COI stand. Indian Pediatr 45:479–480
Geddes AM, Bryceson ADM, Thin RN, Mitchell DM (1995) Diseases due to infection. In: Edwards CRW, Bouchier IAD, Haslett C, Chilvers ER (eds) Davidson’s principles and practice of medicine, 17th edn. ELBS with Churchill Livingstone, Edinburgh, pp 65–189
Yadav S, Thukral R, Chakarvarti A (2003) Comparative evaluation of measles, mumps and rubella vaccine at 9 and 15 months of age. Indian J Med Res 118:183–186
Raut SK, Kulkarni PS, Phadke MA, Jadav SS, Kapre SV, Dhere RM, Dhorje SP, Godse SR (2007) Persistence of antibodies induced by measles-mumps-rubella vaccine in children in India. Clin Vaccine Immunol 14:1370–1371
Indian Academy of Pediatrics (2011) Immunization schedule: January–March 2011. http://www.iapindia.org/immunisation/immunisation-schedule. Accessed 20 April 2011
John TJ (2004) An outbreak of mumps in Thiruvananthapuram district. Indian Pediatr 41:298–300
Abraham M, Abraham P, Jana AK, Kuruvilla KA, Cherian T, Moses PD, Mathai E, John TJ, Sridharan G (1999) Serology in congenital infections: experience in selected symptomatic infants. Indian Pediatr 36:697–700
Gupta E, Dar L, Broor S (2006) Seroprevalence of rubella in pregnant women in Delhi, India. Indian J Med Res 123:833–835
Advisory Committee on Immunization Practices (2007) Recommended adult immunization: United States, October 2007–September 2008. Ann Intern Med 147:725–729
Williams BG, Gouws E, Boschi-Pinto C, Bryce J, Dye C (2002) Estimates of world-wide distribution of child deaths from acute respiratory infections. Lancet Infect Dis 2:25–32
Reddaiah VP, Kapoor SK (1988) Acute respiratory infections in rural under fives. Indian J Pediatr 55:424–426
Cox NJ, Subbarao K (1999) Influenza. Lancet 354:1277–1282
Hayden FG, Palese P (1997) Influenza virus. In: Richman DD, Whitley RJ, Hayden FG (eds) Clinical virology, 1st edn. Churchill Livingstone, New York, pp 911–942
Broor S, Parveen S, Bharaj P, Prasad VS, Srinivasulu KN, Sumanth KM, Kapoor SK, Fowler K, Sullender WM (2007) A prospective three-year cohort study of the epidemiology and virology of acute respiratory infections of children in rural India. PLoS ONE 2:e491
Ramamurthy N, Pillai LC, Gunasekaran P, Elango V, Mohana, Priya P, Sheriff AK (2005) Influenza activity among the pediatric age group in Chennai. Indian J Med Res 121:776–779
Mathew JL (2009) Influenza vaccination for children in India. Indian Pediatr 46:304–307
Balkhy HH, Memish ZA, Bafaqeer S, Almuneef MA (2004) Influenza a common viral infection among Hajj pilgrims: time for routine surveillance and vaccination. J Travel Med 11:82–86
Jameel S (2010) The 2009 influenza pandemic. Curr Sci 98:306–311
Ray K, Potdar VA, Cherian SS, Pawar SD, Jadhav SM, Waregaonkar SR, Joshi AA, Mishra AC (2008) Characterization of the complete genome of influenza A (H5N1) virus isolated during the 2006 outbreak in poultry in India. Virus Genes 36:345–353
Bharat Biotech (2009) Product pipeline. http://www.bharatbiotech.com/prod_pipeline.htm. Accessed 22 April 2011
Rotbart HA (1997) Enteroviruses. In: Richman DD, Whitley RJ, Hayden FG (eds) Clinical virology, 1st edn. Churchill Livingstone, New York, pp 997–1023
Global Polio Eradication Initiative. Infected countries: http://www.polioeradication.org/Infectedcountries.aspx. Accessed 23 April 2011
Sutter RW, John TJ, Jain H, Agarkhedkar S, Ramanan PV, Verma H, Deshpande J, Singh AP, Sreevatsava M, Malankar P, Burton A, Chatterjee A, Jafari H, Aylward RB (2010) Immunogenicity of bivalent types 1 and 3 oral poliovirus vaccine: a randomized, double-blind, controlled trial. Lancet 376:1682–1688
Global Polio Eradication Initiative (2011) Data and monitoring—polio this week. http://www.polioeradication.org/Dataandmonitoring/Poliothisweek.aspx. Accessed 23 April 2011
World Health Organization (2011) WHO prequalified vaccines: http://www.who.int/immunization_standards/vaccine_quality/PQ_vaccine_list_en/en/index.html. Accessed 23 April 2011
Folks TM, Khabbaz RF (1998) Retroviruses and associated diseases in humans (Chapter 38) In: Collier L, Balows A, Sussman M (eds) vol 1: Mahy BWJ, Collier L (eds) Virology: topley & wilson’s microbiology and microbial infections, 9th edn. Arnold, a Member of the Hodder Headline Group, London, Sydney, Auckland, pp 781–803
The rgp120 HIV Vaccine Study Group (2005) Placebo-controlled phase 3 trial of a recombinant glycoprotein 120 vaccine to prevent HIV-1 infection. J Infect Dis 191:654–665
Pitisuttithum P, Gilbert P, Gurwith M, Heyward W, Martin M, van Griensven F, Hu D, Tappero JW, Choopanya K (2006) Bangkok Vaccine Evaluation Group. Randomized, double-blind, placebo-controlled efficacy trial of a bivalent recombinant glycoprotein 120 HIV-1 vaccine among injection drug users in Bangkok, Thailand. J Infect Dis 194:1661–1671
Rerks-Ngarm S, Pitisuttithum P, Nitayaphan S, Kaewkungwal J, Chiu J, Paris R, Pemsri N, Namwat C, de Souza M, Adams E, Benenson M, Gurunathan S, Tartaglia J, McNeil JG, Francis DP, Stablein D, Birx DL, Chunsuttiwat S, Khamboonruang C, Thongcharoen P, Robb ML, Michael NL, Kunasol P, Kim JH, for the MOPH-TAVEG Investigators (2009) Vaccination with ALVAC and AIDSVAX to prevent HIV-1 infection in Thailand. N Engl J Med 361:2209–2220
International AIDS Vaccine Initiative (IAVI) (2011) Research and Development: clinical trials. http://www.iavi.org/researchdevelopment/trials/Pages/ClinicalTrials.aspx. Accessed 24 April 2011
Stover J, Bollinger L, Hecht R, Williams C, Roca E (2007) The impact of an AIDS vaccine in developing countries: a new model and initial results. Health Aff 26:1147–1158
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bharati, K., Vrati, S. Viral Vaccines in India: An Overview. Proc. Natl. Acad. Sci. Sect B. Biol. Sci. 82, 181–198 (2012). https://doi.org/10.1007/s40011-011-0014-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40011-011-0014-9