Abstract
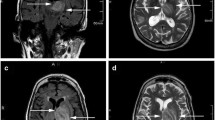
Acanthamoeba spp. is a free-living amoeba, frequently involved in keratitis by contact lens in immunocompetent hosts. Anecdotal reports associate Acanthamoeba spp. as a cause of severe granulomatous encephalitis in immunocompromised and, less frequently, in immunocompetent subjects. Data regarding clinical and therapeutic management are scanty and no defined therapeutic guidelines are available. We describe an unusual case of non-granulomatous Acanthamoeba cerebellitis in an immunocompetent adult male, with abrupt onset of neurological impairment, subtle hemorrhagic infarction at magnetic resonance imaging, and initial suspicion of cerebellar neoplasm. Histopathological findings of excised cerebellar mass revealed the presence of necrosis and inflammation with structure resembling amoebic trophozoites, but without granulomas. Polymerase chain reaction from cerebellar tissue was positive for Acanthamoeba T4 genotype. Due to gastrointestinal intolerance to miltefosine, the patient was treated with long-term course of fluconazole and trimethoprim/sulphamethoxazole, obtaining complete clinical and neuroradiological resolution.


Similar content being viewed by others
References
Koshy AA, Blackburn BGSU. Free living amebae. In: Mandell, Douglas, and Bennett’s principles and practice of infectious diseases. Philadelphia: Saunders; 2015. pp. 3059–69.
Zamora A, Henderson H, Swiatlo E. Acanthamoeba encephalitis: a case report and review of therapy. Surg Neurol Int. 2014;5:68.
Ong TYY, Khan NA, Siddiqui R. Brain-eating amoebae: predilection sites in the brain and disease outcome. J Clin Microbiol. 2017;55:1989–97.
Rodríguez-Pérez EG, Escandón-Vargas K, Ancer A. Granulomatous amebic encephalitis caused by Acanthamoeba sp. in an immunocompetent Mexican adult. Rev Soc Bras Med Trop. 2017;50:432.
McKellar MS, Mehta LR, Greenlee JE, Hale DC, Booton GC, Kelly DJ, et al. Fatal granulomatous Acanthamoeba encephalitis mimicking a stroke, diagnosed by correlation of results of sequential magnetic resonance imaging, biopsy, in vitro culture, immunofluorescence analysis, and molecular analysis. J Clin Microbiol. 2006;44:4265–9.
Singh P, Kochhar R, Vashishta RK, Khandelwal N, Prabhakar S, Mohindra S, et al. Amebic meningoencephalitis: spectrum of imaging findings. Am J Neuroradiol. 2006;27:1217–21.
Guarner J, Bartlett J, Shieh WJ, Paddock CD, Visvesvara GS, Zaki SR. Histopathologic spectrum and immunohistochemical diagnosis of amebic meningoencephalitis. Mod Pathol. 2007;20:1230–7.
Qvarnstrom Y, Visvesvara GS, Sriram R, Da Silva AJ. Multiplex real-time PCR assay for simultaneous detection of Acanthamoeba spp. Balamuthia mandrillaris, and Naegleria fowleri. J Clin Microbiol. 2006;44:3589–95.
Satlin MJ, Graham JK, Visvesvara GS, Mena H, Marks KM, Saal SD, et al. Fulminant and fatal encephalitis caused by Acanthamoeba in a kidney transplant recipient: case report and literature review. Transpl Infect Dis. 2013;15:619–26.
Meersseman W, Lagrou K, Sciot R, Jonckheere J, Haberler C, Walochnik J, et al. Rapidly fatal Acanthamoeba encephalitis and treatment of cryoglobulinemia. Emerg Infect Dis. 2007;13:469–71.
Shirwadkar CG, Samant R, Sankhe M, Deshpande R, Yagi S, Schuster FL, et al. Acanthamoeba encephalitis in patient with systemic lupus, India. Emerg Infect Dis. 2006;12:984–6.
Lorenzo-Morales J, Khan NA, Walochnik J. An update on Acanthamoeba keratitis: diagnosis, pathogenesis and treatment. Parasite. 2015;22:10.
Acknowledgements
We thank Marguerite Kelly Keating, formerly Infectious Disease Pathology Branch, Centers for Disease Control and Prevention (CDC), for critical revision of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
SM, CM, MGC, GC, VFM, FI, CN, IKMA, SR, AC, GZ: no conflict. ADL reports research grants to his Institutions by ViiV Healthcare, Gilead Sciences (fellowship program) and MSD Italy; he has received consultant fees from ViiV Healthcare, Gilead Sciences, MSD Italy, Janssen, Bristol-Myers Squibb and Abbvie; all outside the submitted work. FM has received non-financial support from Angelini and Astellas, outside the submitted work. She has done contract research for Novartis Vaccine and Diagnostic S.rl. (now GSK Vaccine S.r.l.) on behalf of the University Hospital of Siena; she is Infectious Diseases Consultant for GSK (consultancy fee on behalf of University of Siena).
Rights and permissions
About this article
Cite this article
Modica, S., Miracco, C., Cusi, M.G. et al. Non-granulomatous cerebellar infection by Acanthamoeba spp. in an immunocompetent host. Infection 46, 885–889 (2018). https://doi.org/10.1007/s15010-018-1231-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-018-1231-4