Abstract
The COVID-19 has been declared a pandemic by the World Health Organization. Along with impairing the respiratory system, it also affects the gastrointestinal system. By reviewing experiments on the wastewater analysis for the detection of coronavirus, this study explores the fate, persistence, and various remediation strategies for the virus removal from the wastewater. The results indicated that the virus can be detected in the wastewater samples, feces, and sewage, even before the onset of symptoms. Coronavirus can be a potential panzootic disease, as several mammalian species get infected by the deadly virus. The disinfection strategies used earlier for the treatment of wastewater are not sufficient for the removal of viruses from the wastewater. Therefore, concerted efforts should be made to understand their fate, sources, and occurrence in the environmental matrices. To prevent the spread of the panzootic disease, revised guidelines should be issued for the remediation of the virus. Recent viral remediation methods such as membrane bioreactors and advanced oxidation methods can be used. Therefore, the present review puts a light on the current knowledge on the occurrence of coronaviruses in wastewater, the possible sources, fate, and removal strategies.
Similar content being viewed by others
Introduction
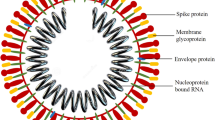
The novel SARS-CoV-2 virus is among the seventh coronavirus which is known to cause human infections. The previously recognized virus are HCoV-NL63, HCoV-OC43, MERS-CoV, SARS-CoV, HCoV-229E, and HCoV-HKU1 (Hasoksuz et al. 2020). Coronavirus is pleomorphic, with RNA as a genetic material, ranging in size from 80 to 160 nM with the positive polarity of 27–32 kb (Sahin et al. 2020). The SARS-CoV-2 virus shares 96.2% genome with bat coronavirus (Yang et al. 2020). The SARS-CoV-2 mortality rate is significantly less than that of severe acute respiratory syndrome SARS (9.6%) and the Middle East respiratory syndrome MERS (35%). The COVID -19 is declared as a pandemic and has caused restrictions and nationwide lockdowns in many countries to prevent the transmission of the infection. Worldwide research is being carried out to study the transmission mechanism of the virus, virus-host interaction, diagnostics, therapeutic strategies, and prevention of the disease (Cascella et al. 2021).
In the last 17 years three major outbreaks of the human coronavirus have been encountered including the SARS (SARS-CoV) which emerged in China in 2003 affecting 26 countries (Hemida 2019). The MERS Coronavirus (MERS-CoV) which emerged in 2012 was the second outbreak of human coronavirus, affecting 27 countries (Hemida 2019, World Health Organization 2020). A recent outbreak emerged in Wuhan China in 2019 of SARS-CoV-2 (Zhu et al. 2020). As of February 24, 2022, there has been a total of 43.7 crores confirmed cases of COVID-19, including 59.6 lac deaths, as indicated by the official data on World Health Organization (WHO) (WHO 2020). The poor proofreading ability of the RNA polymerase is attributed to the emergence of new coronaviruses in a short period (Hofer 2013). The new strains can emerge through recombination leading to their simultaneous occurrence in the same environment (Su et al. 2016).
This virus divides into the epithelial cells leading to infection of the respiratory tract. Symptoms include fever, myalgia, nausea, diarrhea, cough and some may be asymptomatic (Chan et al. 2020; Guan et al. 2020). During the SARS-CoV outbreak in 2003, diarrhea was reported in the first week of the disease in 16–73% of the patients (Yeo et al. 2020a, b). In the ongoing pandemic nearly 2–35% of patients had gastrointestinal symptoms (GI) including diarrhea and vomiting (Wang et al. 2020a).
Previous studies by Amirian 2020; Bowser 2020, detected the presence of viral RNA in the sewage and feces. Xiao et al. 2020a, b, showed the presence of infective virions in the feces (Xiao et al. 2020a, b). The electron microscopy has led to the detection of SARS-CoV-2 virions in stool and the infectious virus was also isolated using cell culture (Yang et al. 2020; Cascella et al. 2021). This raises the possibility of the SARS-CoV-2 transmission by fecal-nasal and fecal–oral pathways (Hemida et al. 2019). Studies by Medema et al. 2020, Randazzo et al. 2020 investigated the SARS-CoV-2 presence in the WWTP influent. A study by Peccia et al. 2020a, b successfully correlated the level of SARS-CoV-2 virus in sludge and wastewater with the disease spread in the population and contagious number of COVID-19. The novel beta coronavirus infects the GI tract using the angiotensin-converting enzyme (ACE-2) receptor by the epithelial cells of the GI tract. (Bivins et al. 2020). The fecal matter eventually reaches the sewage system. Therefore, it is important to understand the persistence of coronavirus in wastewater and its implications on the exposed populations.
The presence of SARS-CoV-2 has already been confirmed in sewage treatment plants (Quilliam et al. 2020). The major source of the transmission of the infection could be wastewater, therefore stringent majors should be adopted for the treatment of the sewage water (Wang et al. 2020a, b). The areas having poor sanitation and water treatment facilities can expose the public to the virus (Usman et al. 2020). The instant response to the pandemic has been focused on preventing the human to human transmission. As there has been an increase in the virus-contaminated biomedical wastewater generation, a possible hazard from contaminated wastewater has been generated. The existing disinfection killing the virus has been reported, the fate of the coronavirus in the water environment in the treatment plants is not yet elucidated (Nghiem et al. 2020; IWA 2020). The wastewater management can lead to the transmission of this deadly virus, the concerns for which have been highlighted during the Ebola virus and SARS-CoV-1 (Chattopadhyay and Taft 2018).
Despite the varying reports generated from the surrogate experiments on the occurrence of SARS-CoV-2 RNA in the wastewater, there is no data available about its persistence in the wastewater. Thus, it becomes imperative to determine the persistence of SARS-CoV-2 in the wastewater to characterize the risk of exposure of wastewater containing the infectious virus to the general public, and also for the researchers working on designing the wastewater-based epidemiology.
The present review puts light on the current state of knowledge of the SARS-CoV-2 in the wastewater processes. We address the potential sources of the coronavirus that might be the reason for the resurgence of the virus in the future. Additionally, the fate of the SARS-CoV-2 has been addressed, which gives an idea of their survival in the wastewater. Also, the virus remediation strategies have been reviewed.
Materials and methods
Firstly, to address the occurrence and fate of SARS-CoV-2 in the environment, the detection of the SARS-CoV-2 in the wastewater is required. Cell culture is used for the detection of infectious viruses. The limitation of the method includes the failure to detect the non-culturable viruses and differentiate between different types of viruses, which are time-consuming and labor-intensive. New techniques such as polymerase chain reaction (PCR), nested PCR, especially the Real-time quantitative PCR (qPCR) which is now frequently used to confirm the coronavirus infection in human nasal swab samples are highly sensitive and specific. The major challenge in the detection and quantification of SARS-CoV-2 is that there are no standardized protocols (Medema et al. 2020). Few considerations must be applied for the detection of SARS-CoV-2 in wastewater including the conditions and sampling time, inactivation of the virus, proper handling of the virus. For higher spatial resolution, upstream sampling of multiple locations is better than downstream sampling. The random sampling at an arbitrary time (Cervantes-Aviles et al. 2021). The composite sampling at 24 h provides the reliable average virus concentration in wastewater (Sherchan et al. 2020). Temperature plays a key role in virus sample collection and preservation. The virus samples can be preserved at 4 °C or − 20 °C. The SARS-CoV-2 RNA can be stored without getting degraded for at least 10 days (Quilliam et al. 2020). Biosafety levels (BSL) must be followed for the proper handling of virus samples. For ex, SARS-CoV-2 should be handled as per BSL 3 guidelines (Cascella et al. 2021). The viral RNA can be detected using a molecular method which includes the enrichment of the virus. Enrichment is required due to low virus titer in the wastewater. The enrichment can be done using filters (0.2 μm) (Wu et al. 2020), ultracentrifugation (Green et al. 2020), ultrafilters (Medema et al. 2020), or by analysis of unfiltered wastewater directly after precipitation, or by directly extracting RNA using electronegative 0.45 um membranes (Ahmed et al. 2020a, b, c). The RNA extraction is usually done via commercially available kits. For ex. PowerFecal Pro kit, Biomerieux Nuclisens kit, RNeasy PowerMicrobiome Kit. Table 1 shows the different methods which are used in the previously reviewed literature for the detection of coronavirus. Recent reports of SARS-CoV-2 RNA detection in wastewater samples suggested that the RNA titers recovered are very low which limits the quantitative detection of the SARS-CoV-2. One of the studies by Green et al. (2020), reported the optimization of simple cushion-based ultracentrifugation for the recovery of RNA from the wastewater. A small sample size (20 mL) was used for the virus recovery in 8 h.
Secondly, the occurrence of SARS-Cov-2 RNA in the wastewater is reviewed based on the previous literature. Table 2 shows the waterborne virus along with its genetic material and the disease caused. In wastewater mainly the occurrence of enteric viruses such as enteroviruses, rotaviruses, adenoviruses, noroviruses, and polioviruses have been reported (Ye et al. 2016). The coronavirus presence in wastewater could differ due to their partitioning behavior in water (Ye et al. 2016). Waterborne viruses are usually transmitted via the fecal-oral route. Vomit, feces, urine, sputum, and handwashing may introduce the coronavirus into the wastewater (Han et al. 2020). The main route of the SARS-CoV-2 virus entry in the wastewater is vi the shedding of viral RNA (Chen et al. 2020). During the SARS outbreak in 2003 in Hong Kong, a cluster of cases were linked to the coronavirus droplets in the wastewater which increased the interest of scientists towards the occurrence of coronavirus in wastewater. Wastewater-based epidemiology (WBE) can be an early warning signal disease outbreak since the virus can be detected weeks before the onset of the illness in the wastewater and feces (Xagoraraki and O’Brien 2020). The infectivity of the virus is not known but reports claim that even after the patient tests negative for COVID-19, the virus can still be present in their feces for up to 33 days (Quilliam et al. 2020). Viral RNA titer present per gram of feces of an infected person can influence the occurrence of coronavirus in wastewater. In SARS the viral load in the feces was reported to be 106.1 gc/g (Hung et al. 2004), whereas it is found to be variable in the stool of SARS-CoV-2 patients. The reports of SARS-CoV-2 presence in the wastewater and sewage around the world are continually increasing. India also reported the presence of the virus in the sewage samples (Kataki et al. 2020). China also reported the possibility the contamination of the drainage system, as the effluent from COVID-19 designated hospital was found to be positive for SARS-CoV-2. In Australia, the SARS-CoV-2 RNA is reported in untreated wastewater (Ahmed et al. 2020a, b, c). Medema et al. 2020, reported the SARS-CoV-2 RNA in wastewater in the Netherlands. The SARS-CoV-2 RNA genome is detected in raw or treated wastewater in France (Randazzo et al. 2020). In Spain, the RNA is detected in six wastewater treatment plants (WWTPs). In the USA, also the presence of coronavirus is confirmed in wastewater (Nemudryi et al. 2020). The coronavirus presence in the wastewater increases its possibility to be aerosolized particularly during the pumping of wastewater (Quilliam et al. 2020). There have been no reports of coronavirus in aerosols from water treatment plants (Fears et al. 2020). SARS-CoV was detected in China (Wang et al. 2005a, b). In India, the presence of the coronavirus is detected in the sewage (Kumar et al. 2020), SARS CoV-2 is detected in wastewater and river in Italy (La Rosa et al. 2020; Rimoldi et al. 2020), the SARS-CoV-2 is also detected in the wastewater in Israel (Or et al. 2020), Japan (Haramota et al. 2020; Hata et al. 2020), Netherlands (Medema et al. 2020), Pakistan (Sharif et al. 2020), Spain (Randazzo et al. 2020; Balboa et al. 2021), Turkey (Kocamemi et al. 2020), and USA (Wu et al. 2020; Nemudryi et al. 2020; Green et al. 2020; Peccia et al. 2020a, b). In Table 3, the list of countries in which the virus (SARS-CoV and SARS-CoV-2) was detected in the sewage and wastewater is presented in tabular form (Amoah et al. 2020).
Taking clue, terms as “detection”, “occurrence”, “wastewater”, “coronavirus”, “virus survival” search was made to identify the related studies. The studies were screened by reading abstracts and some relevant studies were extensively read. To identify the occurrence, fate, and remediation of coronavirus, these studies were divided into various groups: the fate of coronavirus in wastewater, virus remediation, and resurgence of coronavirus. Finally, 20 representative studies were selected, including ten representative studies on the fate and detection of coronavirus in wastewater, eight studies on the remediation of the virus, and two on its resurgence in the environment. Also, two case studies were discussed on the occurrence of coronavirus in wastewater.
Case study 1
The SARS-CoV-2 RNA presence in wastewater can aid to anticipate the COVID-19 infected area
Influent, secondary, and tertiary treated effluent water samples from six different WWTPs were collected in Murcia in March 2020 during the onset of the COVID-19 pandemic. Samples were collected in plastic containers and transferred at 4 °C, concentrated, and processed within 24 h of sampling. The aluminum hydroxide adsorption and precipitation method was used for virus concentration and was validated using a Mengovirus (MgV) and Porcine Epidemic Diarrhea Virus, (PEDV) (Cuevas-Ferrando et al. 2020). Subsequently, after the virus concentration, the viral RNA was extracted and quantified as described in Randazzo et al. 2020. In influent water, the average recoveries of MgV were 10 ± 2.1% and PEDV was 10 ± 3.5% and in effluent 6.2 ± 1.0% for MgV and 3.3 ± 1.6% for PEDV in the period of March to April 2020. On average in untreated wastewater the RNA titers were quantified to be 5.4 ± 0.2 log10 genomic copies/L. 2 out of 18 secondary wastewater samples were tested positive whereas no tertiary wastewater samples were tested positive (0 out of 12). This data reveals that the community members were shedding the SARS-CoV-2 RNA in their feces. Not only this, the presence of SARS-CoV-2 RNA can be detected using the RT-PCR (q-PCR) technique much before the first case is reported and the regular testing of the wastewater samples which comes under the environmental surveillance can help the concerned authorities to design strategies to prevent nationwide lockdowns and curb the infectious disease in the beginning.
Case study 2
Disinfection-based challenges in the septic tanks of hospitals in China
Zhang et al. 2020a, b, detected high titers of coronavirus in the septic tanks in a Chinese hospital which were disinfected using chlorination. The viruses in the feces of the virus-infected patients can behave as a secondary source of coronavirus infection and can potentially contribute to the spread via drainage pipelines. Treatment with a free chlorine concentration of less than 0.5 mg/L for at least 30 min as suggested by WHO and 6.5 mg/L free chlorine for 1.5 h for the complete removal of SARS-CoV-2 viral RNA by the China Center for Disease Control and Prevention has to be re-evaluated. In this study, the chlorination treatment followed by the sodium hypochlorite (800 g/m3) treatment could not potentially remove the SARS-CoV-2 virus from medical septic tanks. The viral RNA is embedded in the patient’s feces which is protected by organic matters from the disinfection treatment and it is released gradually as the free chlorine levels decline. Thus, it becomes imperative to re-consider the disinfection strategies and novel remediation methods that should be incorporated for the complete removal of the coronavirus from the wastewater.
Results and discussion
The fate of SARS-CoV-2 in wastewater
Studies by Kampf et al. 2020 reported that coronavirus is presumed to get inactivated rapidly in the water. But the reports of the presence of human enveloped virus in feces and sewage indicate that they can persist in the water environment longer than previously presumed. Their fate in the environment is mediated by the ability to survive the extreme water environment and their removal at different stages of wastewater treatment. It takes 2–3 days for the 99.9% removal of coronavirus from the wastewater (Gundy et al. 2009) whereas a study by Casanova et al. 2009 reported that coronavirus can be reduced to 99% in a week. For this data, transmissible gastroenteritis virus (TGEV) and mouse hepatitis virus (MHV) were used as coronavirus surrogates along pasteurized water was used to eliminate any possible predation by any microbe in the wastewater. The MHV and TGEV have longer survival as compared to human coronaviruses MERS-CoV and SARS-CoV which is mainly due to differences between different viruses. Based on all the data available, the coronaviruses can be reduced to 99.9% in 3 days at 20 °C (Dennis et al. 2021). The occurrence of SARS-CoV-2 in the wastewater is based on RNA detection. The presence of viable SARS-CoV-2. The temperature, pH, wastewater composition, and structure of the virus are key factors influencing the fate of the virus in wastewater. Coronaviruses are enveloped viruses and have a shorter life span in wastewater when compared to non-enveloped viruses. The shorter life span is attributed to the action of detergents and proteolytic enzymes on the outer lipid envelope of the virus (Aquino de Carvalho et al. 2017). The RNA is single-stranded and less stable and can be degraded by RNases (Brisebois et al. 2018). The MHV can get inactivated in 14 days whereas the TGV gets inactivated in 19 days in pasteurized wastewater (Casanova et al. 2009). The wastewater consists of metazoans, bacteria, chemicals having antiviral activities, and bacterial proteolytic enzymes which leads to faster inactivation of coronaviruses in wastewater (Yu et al. 2014). Temperature is a key factor that determines the fate of coronavirus in wastewater. The SARS-CoV-2 virus remains infectious for 2 days at 20 °C and 14 days at 4 °C in sewage. It is observed that at higher temperatures the virus persistence is reduced due to the increase in the extracellular enzymes and denaturation of nucleic acids and proteins (Aquino de Carvalho et al. 2017). The acidic pH increases the viral adsorption on particles present in wastewater.
The dissemination of coronavirus to aquatic ecosystems may take place mainly due to sewer leakage or during insufficient removal by the WWTPs. The direct discharge of the virus could take place during wastewater leakage and due to the poor infrastructure. The secondary effluent may carry the virus into the environment (Bogler et al. 2020). The rain can increase the concentration of the virus in natural water bodies by the overflowing of the sewer (Hata et al. 2014). Viruses are highly mobile in the subsurface due to the steric interaction between the spike glycoprotein and the porous media (Gutierrez and Nguyen 2013). The SARS-CoV-2 are persistent in water due to their long survival time and size (100 nm approximately). The SARS-CoV-2 virus travels distance which can lead to contamination of freshwater and aquifers which are used for portable use. However, Elkayam et al. 2018, reported that secondary effluent was free from any enteric viruses during infiltration resulting in zero viruses in the groundwater (Elkayam et al. 2018). The wastewater treatment is specifically designed to eliminate the contaminants. WHO prescribes the sanitation guidelines for effluents and no additional guidelines and sanitation protocols are recommended. The chemical, biological, and physical processes are used to remove the virus. The primary treatment consists of the use of sedimentation for virus removal and the secondary treatment is also called biological treatment which combines the aeration tanks along with secondary sedimentation retaining the activated sludge. The adsorption of the virus onto the organic particulates present in the wastewater plays a key role in the secondary treatment of effluents (Bogler et al. 2020). Unlike a non-enveloped virus, the enveloped virus is more likely removed with particulates (Ye et al. 2016). The SARS-CoV-2 virus might get inactivated by the proteolytic and hydrolytic enzymes presented in the consortia of bacteria (Chaudhry et al. 2015). Membrane bioreactors (MBRs) can maximize solid retention and removal and are suggested for eliminating viral loads from wastewater. In a metagenomic study of sludge from WWTPs by Bibby and Peccia 2013, viruses associated with respiratory diseases were detected and 80% of the genes were classified as CoV genes and CoV HKU1 was the second most common virus detected in untreated wastewater (Bibby and Peccia 2013). The complete inactivation or removal of viruses is not observed (Qiu et al. 2015). The secondary effluent is disinfected further before it is discharged in the environment and re-used in Israel. In the USA, it is reused without any disinfection to irrigate wetlands and vineyards Bogler et al. 2020. Chlorination is used to disinfect the secondary effluent but enveloped virus is more susceptible to chlorine treatment than a non-enveloped virus (Ye et al. 2018). The wastewater is concentrated and rich in organic matter which covers the SARS-CoV-2 virus and acts as a physical barrier against disinfection (Geller et al. 2012). The secondary effluent is a complex medium and rich in organic matter therefore sensitive to disinfectants. But in an outbreak of viral infection, in the pandemic the viral load is very high in the untreated wastewater leading to insufficient removal of the virus and the reuse of the water can lead to the transmission of the virus if not disinfected. One of the remedies to get rid of the virus is the tertiary treatment of wastewater which involves disinfection and advanced particle removal. The tertiary treatment includes advanced oxidation processes, sand filtration, membrane technologies, UV radiation, and managed aquifer recharge. In SARS-CoV-1, the UV irradiation at 254 nm is has proved to be beneficial. The tertiary treatment is done in industrialized countries. The membranes used in wastewater treatment are characterized by their pore size. There are four categories: microfiltration, nanofiltration, ultrafiltration, and reverse osmosis. The size of the SARS-CoV-2 is 100 μm, it could be removed via nanofiltration, ultrafiltration, and reverse osmosis.
Chemical disinfectants in the virus removal
Viruses consist of a protein capsid with or without an envelope and the genome can be single or double-stranded RNA or DNA). The SARS-CoV-2 is enveloped and consists of a single-stranded RNA. The chemical disinfectants, the chlorinated compounds do not damage the genome but have an impact on the viral capsid, i.e., lipids or protein of the viral envelope. The secondary treatment of wastewater removes 90–99% (1 to 2-log) of the virus at an average (McLellan et al. 2020), but the removal is highly variable. The primary process of virus inactivation in wastewater is disinfection using radiation or chemical. During the outbreak of the pandemic, the immediate guidelines which were issued by many countries for managing the wastewater were to continue the treated water disinfection. Occupational Safety and Health Administration, USA (OSHO, USA), has stated in February 2020, that disinfection methods to treat wastewater such as oxidation using peracetic acid and hypochlorous acid, and UV irradiation should be helpful in coronavirus inactivation (OSHA 2020). In China, the level of chlorine in disinfection was kept higher than 6.5 mg/L for a contact period of 90 min to disinfect the sewage disposal from the hospital (Kataki et al. 2020), and also as the level of chlorine used for disinfection has increased, the residual chlorine was detected in drinking water but in permissible concentrations, as reported by Ministry of Ecology and Environment, China. Nearly 431 disinfectants have been listed by Environmental Protection Agency (EPA) in June 2020, which are effective against coronavirus (USEPA 2020). The main ingredients of these disinfectants are ethanol, Triethylene glycol, Dischloroisocyanurate, Quaternary ammonium, Phenol, Isopropanol, Peroxyacetic acid, Hydrogen Peroxide, Sodium hypochlorite. To survive in the harsh conditions in the wastewater, the virus remains shielded as a biofilm or embedded physically in suspended particles and organic matter which makes them less vulnerable to the action of the disinfectant (Geller et al. 2012). In the literature survey, there are few reports of the effect of disinfectants on the virus. Firstly, to survive in the harsh conditions in the wastewater, the virus remains shielded as a biofilm or embedded physically in the suspended particle of organic matter which makes them less vulnerable to the action of the disinfectant (Geller et al. 2012) and also in many countries the microbial quality of wastewater guidelines pertains to the bacteriological indicators only (Zhang et al. 2016). Table 4 shows the disinfectants used for the virus elimination.
Disinfectants based on chlorine
These disinfectants release free available chlorine (FAC), i.e., Sodium hypochlorite, elemental chlorine, hypochlorite ion (ClO−), and hypochlorous acid (HOCl), are the most successful disinfectants for virus contamination. Hypochlorite is used to treat organic contaminants due to its strong oxidizing capacity. The virus gets inactivated by chlorine, which is mainly due to downregulation of DNA synthesis, fragmentation of DNA, loss of intracellular contents, inhibition of protein synthesis, decrease in ATP production, amino acids, respiratory products, and sulfhydryl enzymes oxidation, chlorination of amino acids, reduced oxygen uptake, and reduce nutritional uptake (Rutala et al., 2008). According to the reports of Wang et al. 2020a, b, after the primary treatment 30 mg/L to 50 mg/L of chlorine is added to the wastewater and after secondary treatment 15 mg/L to 25 mg/L of chlorine is added to the wastewater (Wang et al. 2020a, b). Chlorination is affected by pH as pH is a key factor in the virus inactivation and chlorine speciation is a critical factor. The chlorine/chloramine speciation in the wastewater must be known before the wastewater treatment (Naddeo and Liu 2020).
-
(a)
Hypochlorites are 5.25–6.15% aqueous solutions of NaOCl and are most commonly used as chlorine disinfectants. They are reported to have better activity as compared to chlorine dioxide against the SARS-CoV virus (Wang et al. 2005a, b). The hypochlorite could remove the SARS-CoV in 30 min at 10 mg/L of chlorine (Wang et al. 2005a, b). Surrogate coronavirus MHC can get a 3 log reduction in a 30 s contact period using a common disinfectant that contains 0.21% of sodium hypochlorite (Dellanno et al. 2009). The SARS-CoV virus can get completely inactivated in less than 1 min contact time at 0.05% concentrated hypochlorite solution (Ansaldi et al. 2004). Zhang et al. 2020a, b studied RNA removal of SARS-CoV-2 in septic tanks using 800–600 g/m3 for a contact period of 1.5 h (Zhang et al. 2020a, b). Hypochlorite is a broad-spectrum virucide. Hypochlorite is a slower virucide at higher pH levels it exists as a hypochlorite ion and in ammonia, the presence exists as ammonia chloramine which is even a slower virucide. Hypochlorite is a non-toxic, fast activity, low cost of operation, and has no adverse to the environment (Yu et al. 2014).
-
(b)
Hypochlorous acid (HOCl) damages the genome and protein of the virus (Wigginton and Kohn 2012). Its efficiency is 50 times more than that of chloramines. The hypochlorous acid virucidal activity was evaluated against avian influenza virus H7N1. The virucidal activity varied at varying concentrations, and at 100 and 200 mg/L of HOCl, the virus was inactivated immediately whereas at 50 mg/L of HOCl, 3 min contact time was required. HOCl has a high likelihood to disinfect the SARS-CoV-2 virus (Block and Rowan 2020). It is regarded as an effective disinfectant for the water which is free of any organic compounds, ammonia, and has no turbidity (Zhang et al. 2016). According to Block and Rowan 2020, the stability of HOCl decreases when exposed to solar radiation, temperature more than 25 °C, air contact, and UV.
-
(c)
Chloramine is a weaker disinfectant and oxidizing agent as compared to HOCl. They belong to the combined chlorinated compounds and pose certain advantages such as more stability (WHO 2004). They are found to inactivate the Coxsackie virus and Poliovirus (Kelly and Sanderson 1958). The tablets of chloramine are used in water purification by the military in an emergency. The chloramines can react slowly and penetrate the biofilm and gradually inactivate the embedded virus (Symons et al. 1978). They are preferred secondary disinfectants as compared to primary disinfectants as they have weak action. But their stability and low by-product formation make them a good choice as a secondary disinfectant (Earth Tech 2005).
-
(d)
Chlorine dioxide (ClO2) is advantageous as compared to chlorine. It is used as an ideal candidate for viral inactivation and can be used as a Cl alternative (Sanekata et al. 2010). ClO2 reacts with virus RNA and adsorbs into the capsomeres protein of the virus. ClO2 has less efficacy against the SARS-CoV virus than Cl (Wang et al. 2005a, b). ClO2 at 40 mg/L could disinfect the SARS-CoV virus after 30 min. According to Kim et al. 2016 studies, the murine coronavirus gets inactivated after direct exposure to ClO2 gas. It has certain advantages as no toxic by-product formation takes place, does not react with ammonia, and is active at a broad pH range but have certain disadvantages as it is unstable, can react with oxidizable materials, is capable of deodorizing and decolorizing, can lead to the explosive production of halogenated organic compounds (Harakeh et al. 1987).
MBRs for virus removal
For wastewater reuse, the MBR is a preferred technology and is an alternative to the conventional anaerobic digestion process. The membrane technology has a low capital cost and energy requirement which increases its prospect for the treatment of wastewater. MBR integrates membrane technology with an activated sludge process. There are mainly four processes that aid in the virus removal by the MBR namely the attachment of the membrane to organic particulates, membrane interception, an interception by the cake layer of the membrane, and contaminants breakdown by the enzymes (Chaudhry et al. 2015). Virus and bacterial removal along with the recycling of wastewater is the advantage of MBR. However higher operational cost and foaming propensity are certain disadvantages of the same. MBR is an effective technology for the removal of pathogens such as SARS-CoV-2 (Lesimple et al. 2020). MBR can efficiently remove viral loads as low as 27 μM and the diameter of SARS-CoV-2 range between 60 and 140 nm when viral load is between 202.103 copies/mL (Wang et al. 2020a, b).
Advanced oxidation process (AOP) for the virus removal
The presence of SARS-CoV-2 in wastewater is reported, and it has impacted the likelihood to reuse the water after treatment (Tetteh et al. 2020). The use of UV/H2O2 to remove the virus after tertiary treatment (Shu et al. 2016). The hydroxyl radicals can remove chemicals present in wastewater (Cuerda-Correa et al. 2020). The organic molecules get bombarded with hydroxyl rapidly and non-selectively. AOPs include Fenton, photo-Fenton, ultrasonic, and photocatalysis processes. Ozone combined with hydrogen peroxide, UV irradiation, and catalyst, Fe2+/UV/H2O2, H2O2/UV is used for the removal of contaminants (Tetteh et al. 2020). The AOP has a remarkable ability and can mineralize a broad range of contaminants including coronavirus, it is eco-friendly, does not require costly and hazardous artificial lights instead make use of solar lights (Chollom et al. 2020). The potential of AOPs is twice that commonly used disinfectant, chlorine. The pollutants concentration gets reduced to parts per billion (ppb) from parts per million (ppm) (Kim et al. 2016). The hydroxyl radical is reactive and non-selective which can potentially remove all the pollutants, after the formation of intermediates with the –OH radical (Cuerda-Correa et al. 2020). The AOPs have helped in the 90% inactivation of influenza A virus (H3N2), Mycobacterium smegmatis, Bacillus thuringiensis, and vaccinia virus. In the study, undoped platinum dioxide and platinized sulfated platinum dioxide was used along with microorganisms which were loaded over photocatalyst films from aerosols (Brugnera et al. 2016). The high oxidation potential of the hydroxyl molecule and fast reaction rate make AOPs better than the traditional treatment processes. The fast reaction process leads to low retention times which can be advantageous. Certain advantages of AOPs over other methods are: can treat almost all contaminants, robust technology and rapid, no new toxic by-products are introduced theoretically into the water as compared to the toxic by-product formation in dichlorination, stable inorganic compounds are formed, and as compared to chemical or biological process, no sludge formation is observed in AOP. High energy requirements, residual peroxide removal can be a problem, complex chemistry for certain contaminants and high cost and maintenance are certain disadvantages of AOPs.
Resurgence of coronavirus
Wastewater is one possible source of the resurgence of coronavirus since the viruses have been detected in the feces of COVID-19 patients, there is a growing concern over the risk for fecal-oral transmission to animals and humans. Not all sewage can reach WWTPs, it is only during storms there is a risk of overspill from drains that can leach the sewage and enter the environment. During heavy rainfall, the sewage can overspill from drains and lead to the resurgence of COVID-19. WBE is generally used to monitor the resurgence of the virus and its prevalence among the population (Ahmed et al. 2020a, b, c). Wastewater contains viruses excreted from the patients both symptomatic and asymptomatic present in a studied location. As the coronavirus is shed along with human excreta and due to poor sanitation facilities disposed of in the sewage or environment, thus the WBE can be successfully used for monitoring the spread of SARS-CoV-2. There are certain limitations on the use of WBE in monitoring the spread and resurgence of COVID-19, firstly not all patients excrete the SARS-CoV-2 in feces and low virus titer in fecal material can hamper its detection in wastewater.
WBE is used in many countries as a surveillance tool and a valuable warning alert for the determination of the population for testing, to tailor mitigation measures and containment. In the USA, WBE studies are carried out in many countries including Connecticut, Louisiana, Montana, Massachusetts, New York, and Virginia, and also in the sludge samples and wastewater. Viral RNA was detected between 13 and 100% in the investigations carried out which was in accordance with local epidemiological data. WBE is important as it can track the community-level spread of the disease. Although the shedding of the virus is approximately 51% only, the SARS-CoV-2 level in wastewater is a beneficial measurement than the actual number of cases that are confirmed in the community. This is mainly because people may shed the coronavirus earlier than the appearance of the confirmed cases, and many asymptomatic cases are also accounted for. Each SARS-CoV-2 infected person sheds millions of copies of the viral genome daily, which translates into > 100 million copies of genome per liter of wastewater generated (Hart et al. 2020). Sample from WWTPs may provide us with a snapshot of disease prevalence at a town or city level. This will allow the government to direct vaccines and tests in a specific area, and impose restrictions. Wastewater can potentially lead to a resurgence of coronavirus, but there are potential unknown sources that might lead to the resurgence of the virus in the future. An integrated approach that involves nanoscience and facilitates the early detection of the coronavirus is reported by Adeel et al. (2021). The study described the development of the gold nanoparticle-based colorimetric system which can allow the detection of SARS-CoV- 2 with “naked eye’”. The assay used can target the N-gene in SARS-CoV-2 and the agglomeration of gold nanoparticles against the target RNA results in a precipitate that can be visible and reduces the detection time to 10 min. These diagnostic systems are convenient, reliable, and rapid and have the potential for community-level diagnosis (Moitra et al. 2020).
Critical knowledge gaps
Only a few researchers have successfully isolated infective SARS-CoV-2 from urine and stool samples, although many studies have detected the virus in wastewater and stool (Sun et al. 2020). It is not clear to date if the SARS-CoV-2 virus in the stool originates from active replication within the gastrointestinal tract or in the sputum. If the virus replicates in the gastrointestinal tract then the virions may get disseminated via wastewater (Medema et al. 2020). However, the experimental study via bioinformatics modeling revealed that the virions get replicated in the GI tract (Danchin et al. 2021). An epidemiological model based on data in the Wuhan epidemic suggests that the fecal-oral route is important for the virus transmission, suggesting that there is a high possibility that the virus may replicate in the intestine. Thus, based on all these studies it might be assumed that the wastewater contains a considerable number of infective virions (Wu et al. 2020). The unsuccessful isolation of infective viruses from wastewater and stool samples is because of the difficulty to isolate enveloped virions (Bogler et al. 2020). Waterborne transmission imposes a great threat to the spread of COVID-19. The waterborne transmission risk is highest in the area which is densely populated, lacks an adequate system for wastewater treatment, and therefore has direct exposure to aerosolized wastewater, especially the developing and underdeveloped countries. There is an urgent need for the detection of infective SARS-CoV-2 virus in the wastewater, which is important for generating a quantitative risk assessment, along with the proper measures of the wastewater and disinfection strategies, and epidemic surveillance is vital to determine the extent, prevalence, and outbreak of the pandemic within the community. For proper mitigation of the SARS-CoV-2 following knowledge, gaps need to be addressed. Firstly, the SARS-CoV-2 virus concentration is estimated by quantifying the RNA of the virus rather than quantifying the infective virions. Secondly, the minimal dose from water and aerosols which can cause infection is not known. Thirdly, the extent to which the SARS-CoV-2 virus gets disseminated through waterborne pathways is not known.
Conclusion
Coronavirus emerged at the end of 2019 and was generated as a pandemic within a few months. It is a serious threat to health care systems globally. It was initially thought to affect the respiratory system but soon proved to affect the gastrointestinal system also. The infective virus is shed in feces which leads to their occurrence in wastewater. The virus can survive in wastewater for a few days and remains infectious. The survival of the virus in the wastewater depends on the composition of the wastewater, pH, structure of the virus, and temperature. The wastewater treatment is useful in the removal or inactivation of the virus, use of disinfectant after primary or secondary treatment, along with advanced oxidation processes and MBR can help in the remediation of the virus. Further study should focus on studying the shedding frequency of the SARS-CoV-2 in feces and urine which is significant in understanding the viral load per infected person. The quantification methods for the SARS-CoV-2 virus shall be optimized. SARS-CoV-2 has can be transmitted to animals via humans. SARS-CoV-2 can be a potential threat as it can be a panzootic disease, and therefore it is important to minimize the spread of coronavirus in the environment. WWTPs can aid in the early detection of the virus and using WBE, virus detection can be done in any area. The efficacy of different conventional WWTPs shall be studied. Global awareness should be developed even in developing countries to find remedies for the improvement in WWTPs. Although the SARS-CoV-2 transmission is not common through the fecal-oral route, because it is the third novel strain of coronavirus that has emerged as a global pandemic, there is a possibility of the pandemic more easily transmissible via this route. Virus models can be used to characterize the removal efficiency of the SARS-CoV-2. A combination of different methods such as the use of classical and advanced methods can be used for the remediation of virus. A combination of primary, secondary, and tertiary treatment methods can be used for the removal of the virus. Considering the huge economic cost the entire world has to pay for the pandemic, concerted efforts should be put into improving wastewater treatment.
References
Adeel M, Farooq T, Shakoor N, Ahmar S, Fiaz S, White JC, Rui Y (2021) Covid-19 and nanoscience in the developing world: rapid detection and remediation in wastewater. Nanomaterials 11(4):991
Ahmed W, Angel N, Edson J, Bibby K, Bivins A, O’Brien JW, Choi PM, Kitajima M, Simpson SL, Li J, Tscharke B, Mueller JF (2020a) First confirmed detection of SARS-CoV-2 in untreated wastewater in Australia: a proof of concept for the wastewater surveillance of COVID-19 in the community. Sci Total Environ 728:138764. https://doi.org/10.1016/j.scitotenv.2020.138764
Ahmed W, Bertsch PM, Bibby K, Haramoto E, Hewitt J, Huygens F, Gyawali P, Korajkic A, Riddell S, Sherchan SP, Simpson SL, Bivins A (2020b) Decay of SARS-CoV-2 and surrogate murine hepatitis virus RNA in untreated wastewater to inform application in wastewater-based epidemiology. Environ Res 191:110092
Ahmed W, Bertsch PM, Bivins A, Bibby K, Farkas K, Gathercole A, Haramoto E, Gyawali P, Korajkic A, McMinn BR, Mueller JF, Kitajima M (2020c) Comparison of virus concentration methods for the RT-qPCR-based recovery of murine hepatitis virus, a surrogate for SARS-CoV-2 from untreated wastewater. Sci Total Environ 739:139960
Amirian ES (2020) Potential fecal transmission of SARS-CoV-2: Current evidence and implications for public health. Int J Infect Dis 95:363–370
Amoah ID, Kumari S, Bux F (2020) Coronaviruses in wastewater processes: source, fate and potential risks. Environ Int 143:105962
Ansaldi F, Banfi F, Morelli P, Valle L, Durando P, Sticchi L, Contos S, Gasparini R, Crovari P (2004) SARS-CoV, influenza A and syncitial respiratory virus resistance against common disinfectants and ultraviolet irradiation. J Prev Med Hyg 45(1–2):5–8
Aquino de Carvalho N, Stachler EN, Cimabue N, Bibby K (2017) Evaluation of Phi6 persistence and suitability as an enveloped virus surrogate. Environ Sci Technol 51(15):8692–8700
Balboa S, Mauricio-Iglesias M, Rodriguez S, Martínez-Lamas L, Vasallo FJ, Regueiro B, Lema JM (2021) The fate of SARS-COV-2 in WWTPS points out the sludge line as a suitable spot for detection of COVID-19. Sci Total Environ 772:145268
Bibby K, Peccia J (2013) Identification of viral pathogen diversity in sewage sludge by metagenome analysis. Environ Sci Technol 47(4):1945–1951
Block MS, Rowan BG (2020) Hypochlorous acid–a review. J Oral Maxillofac Surg 78:1461–1466
Bogler A, Packman A, Furman A, Gross A, Kushmaro A, Ronen A, Dagot C, Hill C, Vaizel-Ohayon D, Morgenroth E, Bertuzzo E, Bar-Zeev E (2020) Rethinking wastewater risks and monitoring in light of the COVID-19 pandemic. Nat Sustain 1–10
Bowser AD (2020) Coronavirus may cause environmental contamination through fecal shedding. Medscape medical news. Accessed on 20th April
Brisebois E, Veillette M, Dion-Dupont V, Lavoie J, Corbeil J, Culley A, Duchaine C (2018) Human viral pathogens are pervasive in wastewater treatment center aerosols. J Environ Sci 67:45–53
Brugnera MF, de Araújo Souza BC, Zanoni MVB (2016) Advanced oxidation process applied to actinobacterium disinfection. Actinobacteria Basics Biotechnol Appl 353
Casanova L, Rutala WA, Weber DJ, Sobsey MD (2009) Survival of surrogate coronaviruses in water. Water Res 43(7):1893–1898
Cascella M, Rajnik M, Aleem A, Dulebohn S, Di Napoli R (2021) Features, evaluation, and treatment of coronavirus (COVID-19). StatPearls
Cervantes-Avilés P, Moreno-Andrade I, Carrillo-Reyes J (2021) Approaches applied to detect SARS-CoV-2 in wastewater and perspectives post-COVID-19. J Water Process Eng 40:101947
Chan KH, Poon LL, Cheng VCC, Guan Y, Hung IFN, Kong J, Yam LY, Seto WH, Yuen KY, Peiris JSM (2004) Detection of SARS coronavirus in patients with suspected SARS. Emerg Infect Dis 10(2):294
Chan JFW, Yuan S, Kok KH, To KKW, Chu H, Yang J, Xing F, Liu J, Yip CC, Poon RW, Tsoi HW, Yuen KY (2020) A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet 395(10223):514–523
Chattopadhyay S, Taft S (2018) Exposure Pathways to High-Consequence Pathogens in the Wastewater Collection and Treatment Systems. US Environmental Protection Agency, Cincinnati, OH
Chaudhry RM, Nelson KL, Drewes JE (2015) Mechanisms of pathogenic virus removal in a full-scale membrane bioreactor. Environ Sci Technol 49(5):2815–2822
Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, Qiu Y, Wang J, Liu Y, Wei Y, Yu T, Zhang L (2020) Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 395(10223):507–513
Chollom MN, Rathilal S, Swalaha FM, Bakare BF, Tetteh EK (2020) Removal of antibiotics during the anaerobic digestion of slaughterhouse wastewater. Planning 15(3):335–343
Corman VM, Albarrak AM, Omrani AS, Albarrak MM, Farah ME, Almasri M, Muth D, Sieberg A, Meyer B, Assiri AM, Binger T, Memish ZA (2016) Viral shedding and antibody response in 37 patients with Middle East respiratory syndrome coronavirus infection. Clin Infect Dis 62(4):477–483
Cuerda-Correa EM, Alexandre-Franco MF, Fernández-González C (2020) Advanced oxidation processes for the removal of antibiotics from water. An overview. Water 12(1):102
Cuevas-Ferrando E, Randazzo W, Pérez-Cataluña A, Sánchez G (2020) HEV occurrence in waste and drinking water treatment plants. Front Microbiol 10:2937
Danchin A, Ng TW, Turinici G (2021) A new transmission route for the propagation of the SARS-CoV-2 coronavirus. Biology 10(1):10
Dennis JM, McGovern AP, Vollmer SJ, Mateen BA (2021) Improving survival of critical care patients with coronavirus disease 2019 in England: a national cohort study. Crit care med 49(2):209
Darnell ME, Subbarao K, Feinstone SM, Taylor DR (2004) Inactivation of the coronavirus that induces severe acute respiratory syndrome, SARS-CoV. J Virol Methods 121(1):85–91
Dellanno C, Vega Q, Boesenberg D (2009) The antiviral action of common household disinfectants and antiseptics against murine hepatitis virus, a potential surrogate for SARS coronavirus. Am J Infect Control 37(8):649–652
Dhama K, Khan S, Tiwari R, Sircar S, Bhat S, Malik YS, Singh KP, Chaicumpa W, Bonilla-Aldana DK, Rodriguez-Morales AJ (2020) Coronavirus disease 2019–COVID-19. Clin Microbiol Rev 33(4):e00028-20
Drosten C, Seilmaier M, Corman VM, Hartmann W, Scheible G, Sack S, Guggemos W, Kallies R, Muth D, Junglen S, Müller MA, Wendtner CM (2013) Clinical features and virological analysis of a case of Middle East respiratory syndrome coronavirus infection. Lancet Infect Dis 13(9):745–751
Earth Tech (2005) Available at:https://www.gov.mb.ca/sd/waterstewardship/odw/reginfo/approvals/odw_chlorine_and_alternative_disinfectants.pdf. Accessed on 26 June 2020
Elkayam R, Aharoni A, Vaizel-Ohayon D, Sued O, Katz Y, Negev I, Marano RB, Cytryn E, Shtrasler L, Lev O (2018) Viral and microbial pathogens, indicator microorganisms, microbial source tracking indicators, and antibiotic resistance genes in a confined managed effluent recharge system. J Environ Eng 144(3):05017011
Fears AC, Klimstra WB, Duprex P, Hartman A, Weaver SC, Plante KC, Mirchandani D, Plante JA, Aguilar PV, Fernandez D, Nalca A, Roy CJ (2020) Comparative dynamic aerosol efficiencies of three emergent coronaviruses and the unusual persistence of SARS-CoV-2 in aerosol suspensions. medRxiv
Gehr R, Chen D, Moreau M (2009) Performic acid (PFA): tests on an advanced primary effluent show promising disinfection performance. Water Sci Technol 59(1):89–96
Geller C, Varbanov M, Duval RE (2012) Human coronaviruses: insights into environmental resistance and its influence on the development of new antiseptic strategies. Viruses 4(11):3044–3068
Green H, Wilder M, Middleton FA, Collins M, Fenty A, Gentile K, Zeng T, Middleton FA, Larsen DA (2020) Quantification of SARS-CoV-2 and cross-assembly phage (crAssphage) from wastewater to monitor coronavirus transmission within communities. MedRxiv
Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, Liu L, Shan H, Lei CL, Hui DS, Du B, Zhong NS (2020) Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 382(18):1708–1720
Gundy PM, Gerba CP, Pepper IL (2009) Survival of coronaviruses in water and wastewater. Food Environ Virol 1(1):10–14
Gutierrez L, Nguyen TH (2013) Interactions between rotavirus and natural organic matter isolates with different physicochemical characteristics. Langmuir 29(47):14460–14468
Han MS, Seong MW, Heo EY, Park JH, Kim N, Shin S, Cho SI, Park SS, Choi EH (2020) Sequential analysis of viral load in a neonate and her mother infected with severe acute respiratory syndrome coronavirus 2. Clin Infect Dis 71(16):2236–2239
Harakeh S (1987) The behavior of viruses on disinfection by chlorine dioxide and other disinfectants in effluent. FEMS Microbiol Lett 44(3):335–341
Haramoto E, Malla B, Thakali O, Kitajima M (2020) First environmental surveillance for the presence of SARS-CoV-2 RNA in wastewater and river water in Japan. Sci Total Environ 737:140405
Hart OE, Halden RU (2020) Computational analysis of SARS-CoV-2/COVID-19 surveillance by wastewater-based epidemiology locally and globally: feasibility, economy, opportunities and challenges. Sci Total Environ 730:138875
Hasöksüz M, Kiliç S, Saraç F (2020) Coronaviruses and sars-cov-2. Turk J Med Sci 50(SI-1):549–556
Hata A, Katayama H, Kojima K, Sano S, Kasuga I, Kitajima M, Furumai H (2014) Effects of rainfall events on the occurrence and detection efficiency of viruses in river water impacted by combined sewer overflows. Sci Total Environ 468:757–763
Hata A, Honda R, Hara-Yamamura H, Meuchi Y (2020) Detection of SARS-CoV-2 in wastewater in Japan by multiple molecular assays-implication for wastewater-based epidemiology (WBE). MedRxiv
Hemida MG (2019) Middle East respiratory syndrome coronavirus and the one health concept. PeerJ 7:e7556
Hofer U (2013) Fooling the coronavirus proofreading machinery. Nat Rev Microbiol 11(10):662–663
Hung IFN, Cheng VCC, Wu AKL, Tang BSF, Chan KH, Chu CM, Wong MM, Hui WT, Poon LL, Tse DM, Chan KS, Yuen KY (2004) Viral loads in clinical specimens and SARS manifestations. Emerg Infect Dis 10(9):1550
IWA (2020) COVID-19 and safe water treatment utilities are in the focus 2020 international water association. Accessed on 3 July 2020
Kampf G, Todt D, Pfaender S, Steinmann E (2020) Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J Hosp Infect 104(3):246–251
Kataki S, Chatterjee S, Vairale MG, Sharma S, Dwivedi SK (2020) Concerns and strategies for wastewater treatment during COVID-19 pandemic to stop plausible transmission. Resour Conserv Recycl 164:105156
Kelly S, Sanderson WW (1958) The effect of chlorine in water on enteric viruses. Am J Public Health Nations Health 48(10):1323–1334
Kim J, Shin BH, Song KJ, Kim JR, Kim K (2016) Virucidal effect of gaseous chlorine dioxide on murine coronavirus A59
Kocamemi BA, Kurt H, Sait A, Sarac F, Saatci AM, Pakdemirli B (2020) SARS-CoV-2 detection in Istanbul wastewater treatment plant sludges. medRxiv
Kumar M, Patel AK, Shah AV, Raval J, Rajpara N, Joshi M, Joshi CG (2020) First proof of the capability of wastewater surveillance for COVID-19 in India through detection of genetic material of SARS-CoV-2. Sci Total Environ 746:141326
Kweinor Tetteh E, Opoku Amankwa M, Armah EK, Rathilal S (2020) Fate of COVID-19 occurrences in wastewater systems: emerging detection and treatment technologies—a review. Water 12(10):2680
La Rosa G, Iaconelli M, Mancini P, Bonanno Ferraro G, Veneri C, Bonadonna L, Lucentini L, Suffredini E (2020) First detection of SARS-CoV-2 in untreated wastewaters in Italy. Sci Total Environ 736:139652. https://doi.org/10.1016/j.scitotenv.2020.139652
Lesimple A, Jasim SY, Johnson DJ, Hilal N (2020) The role of wastewater treatment plants as tools for SARS-CoV-2 early detection and removal. J Water Process Eng 38:101544
Liberti L, Lopez A, Notarnicola M (1999) Disinfection with peracetic acid for domestic sewage re-use in agriculture. Water Environ J 13(4):262–269
McDonnell G, Russell AD (1999) Antiseptics and disinfectants: activity, action, and resistance. Clin Microbiol Rev 12(1):147
McDonnell G (2009) The use of hydrogen peroxide for disinfection and sterilization applications. PATAI’S Chemistry of Functional Groups. pp 1–34
McLellan N, Pernitsky D, Umble A (2020) Coronavirus and the water cycle—here is what treatment professionals need to know. Water Online https://www.wateronline.com/doc/coronavirus-and-the-water-cycle-here-is-what-treatment-professionals-need-to-know-0001
Medema G, Heijnen L, Elsinga G, Italiaander R, Brouwer A (2020) Presence of SARS-Coronavirus-2 RNA in sewage and correlation with reported COVID-19 prevalence in the early stage of the epidemic in the Netherlands. Environ Sci Technol Lett 7(7):511–516
Moitra P, Alafeef M, Dighe K, Frieman MB, Pan D (2020) Selective naked-eye detection of SARS-CoV-2 mediated by N gene targeted antisense oligonucleotide capped plasmonic nanoparticles. ACS Nano 14(6):7617–7627. https://doi.org/10.1021/acsnano.0c03822
Naddeo V, Liu H (2020) Editorial perspectives: 2019 novel coronavirus (SARS-CoV-2): what is its fate in urban water cycle and how can the water research community respond? Environ Sci Water Res Technol 6(5):1213–1216
Nemudryi A, Nemudraia A, Surya K, Wiegand T, Buyukyoruk M, Wilkinson R, Wiedenheft B (2020) Temporal detection and phylogenetic assessment of SARS-CoV-2 in municipal wastewater. Medrxiv. https://doi.org/10.1101/2020.04.15.20066746
Nghiem LD, Morgan B, Donner E, Short MD (2020) The COVID-19 pandemic: considerations for the waste and wastewater services sector. Case Stud Chem Environ Eng 1:100006
Or IB, Yaniv K, Shagan M, Ozer E, Erster O, Mendelson E, Mannasse B, Shirazi R, Kushmaro A (2020) Regressing SARS-CoV-2 sewage measurements onto COVID-19 burden in the population: a proof-of-concept for quantitative environmental surveillance. MedRxiv
OSHA (2020) OSHA, standards and directives for COVID-19, United States of America occupational safety and health administration. Available at: https://www.osha.gov/SLTC/covid-19/standards.html
Peccia J, Zulli A, Brackney DE, Grubaugh ND, Kaplan EH, Casanovas-Massana A, Ko AI, Malik AA, Wang D, Wang M, Warren JL, Omer SB (2020a) SARS-CoV-2 RNA concentrations in primary municipal sewage sludge as a leading indicator of COVID-19 outbreak dynamics. MedRxiv
Peccia J, Zulli A, Brackney DE, Grubaugh ND, Kaplan EH, Casanovas-Massana A, Ko AI, Malik AA, Wang D, Wang M, Warren JL, Omer SB (2020b) SARS-CoV-2 RNA concentrations in primary municipal sewage sludge as a leading indicator of COVID-19 outbreak dynamics. MedRxiv
Qiu Y, Lee BE, Neumann N, Ashbolt N, Craik S, Maal-Bared R, Pang XL (2015) Assessment of human virus removal during municipal wastewater treatment in Edmonton, Canada. J Appl Microbiol 119(6):1729–1739
Quilliam RS, Weidmann M, Moresco V, Purshouse H, O'Hara Z, Oliver DM (2020) COVID-19: the environmental implications of shedding SARS-CoV-2 in human faeces. Environ Int
Randazzo W, Truchado P, Cuevas-Ferrando E, Simón P, Allende A, Sánchez G (2020) SARS-CoV-2 RNA in wastewater anticipated COVID-19 occurrence in a low prevalence area. Water Res 181:115942
Rimoldi SG, Stefani F, Gigantiello A, Polesello S, Comandatore F, Mileto D, Maresca M, Longobardi C, Mancon A, Romeri F, Pagani C, Salerno F (2020) Presence and infectivity of SARS-CoV-2 virus in wastewaters and rivers. Sci Total Environ 744:140911
Rutala WA, Weber DJ (2008) Guideline for disinfection and sterilization in healthcare facilities
Sahin AR, Erdogan A, Agaoglu PM, Dineri Y, Cakirci AY, Senel ME, Okyay RA, Tasdogan AM (2020) 2019 novel coronavirus (COVID-19) outbreak: a review of the current literature. EJMO 4(1):1–7
Sanekata T, Fukuda T, Miura T, Morino H, Lee C, Maeda KEN, Araki K, Otake T, Kawahata T, Shibata T, Shibata T (2010) Evaluation of the antiviral activity of chlorine dioxide and sodium hypochlorite against feline calicivirus, human influenza virus, measles virus, canine distemper virus, human herpesvirus, human adenovirus, canine adenovirus and canine parvovirus. Biocontrol Sci 15(2):45–49
Schrank CL, Minbiole KP, Wuest WM (2020) Are quaternary ammonium compounds, the workhorse disinfectants, effective against severe acute respiratory syndrome-Coronavirus-2? ACS Infect Dis 6(7):1553–1557
Sharif S, Ikram A, Khurshid A, Salman M, Mehmood N, Arshad Y, Ali N et al.(2020) Detection of SARS-Coronavirus-2 in wastewater, using the existing environmental surveillance network: an epidemiological gateway to an early warning for COVID-19 in communities. MedRxiv
Sherchan SP, Shahin S, Ward LM, Tandukar S, Aw TG, Schmitz B, Ahmed W, Kitajima M (2020) First detection of SARS-CoV-2 RNA in wastewater in North America: a study in Louisiana, USA. Sci Total Environ 743:140621
Shu Z, Singh A, Klamerth N, McPhedran K, Bolton JR, Belosevic M, El-Din MG (2016) Pilot-scale UV/H2O2 advanced oxidation process for municipal reuse water: assessing micropollutant degradation and estrogenic impacts on goldfish (Carassius auratus L.). Water Res 101:157–166
Su S, Wong G, Shi W, Liu J, Lai AC, Zhou J, Liu W, Bi Y, Gao GF (2016) Epidemiology, genetic recombination, and pathogenesis of coronaviruses. Trends Microbiol 24(6):490–502
Sun J, Zhu A, Li H, Zheng K, Zhuang Z, Chen Z, Shi Y, Zhang Z, Chen SB, Liu X, Dai J, Li YM (2020) Isolation of infectious SARS-CoV-2 from urine of a COVID-19 patient. Emerg Microbes Infect 9(1):991–993
Symons JM (1978) Ozone, chlorine dioxide and chloramines as alternatives to chlorine for disinfection of drinking water. Water Chlorination Environ Impact Health Effects 2
USEPA (2020) List N: disinfectants for use against SARS-CoV. Available at: https://www.epa.gov/pesticide-registration/list-n-disinfectants-use-against-sars-cov-2
Usman M, Farooq M, Hanna K (2020) Existence of SARS-CoV-2 in wastewater: implications for its environmental transmission in developing communities
Wang XW, Li JS, Guo TK, Zhen B, Kong QX, Yi B, Li Z, Song N, Jin M, Wu XM, Xiao WJ, Li JW (2005a) Excretion and detection of SARS coronavirus and its nucleic acid from digestive system. World J Gastroenterol WJG 11(28):4390
Wang XW, Li JS, Jin M, Zhen B, Kong QX, Song N, Li Z, Song N, Jin M, Wu XM, Xiao WJ, Li JW (2005b) Study on the resistance of severe acute respiratory syndrome-associated coronavirus. J Virol Methods 126(1–2):171–177
Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, Wang B, Xiang H, Cheng Z, Xiong Y, Zhao Y, Li Y, Wang X, Peng Z (2020a) Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA 323(11):1061–1069. https://doi.org/10.1001/jama.2020.1585
Wang J, Shen J, Ye D, Yan X, Zhang Y, Yang W, Li X, Wang J, Zhang L, Pan L (2020b) Disinfection technology of hospital wastes and wastewater: Suggestions for disinfection strategy during coronavirus disease 2019 (COVID-19) pandemic in China. Environ Pollut 262:114665
WHO (2020) Novel coronavirus (2019-nCoV)—situation report—22. Situation report—22. Retrieved from https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200211-sitrep-22-ncov.pdf?sfvrsn=fb6d49b1_2
Wigginton KR, Kohn T (2012) Virus disinfection mechanisms: the role of virus composition, structure, and function. Curr Opin Virol 2(1):84–89
Wong K, Fong TT, Bibby K, Molina M (2012) Application of enteric viruses for fecal pollution source tracking in environmental waters. Environ Int 45:151–164
World Health Organization (2004) Manganese in drinking-water: background document for development of WHO guidelines for drinking-Water quality (No. WHO/SDE/WSH/03.04/104). World Health Organization
World Health Organization (2020) Water, sanitation, hygiene and waste management for COVID-19: technical brief, 03 March 2020a (No. WHO/2019-NcOV/IPC_WASH/2020a.1). World Health Organization
Wu F, Zhang J, Xiao A, Gu X, Lee WL, Armas F, Kauffman K, Hanage W, Matus M, Ghaeli N, Endo N, Alm EJ (2020) SARS-CoV-2 titers in wastewater are higher than expected from clinically confirmed cases. Msystems 5(4):e00614-20
Xagoraraki I, O’Brien E (2020) Wastewater-based epidemiology for early detection of viral outbreaks. Women in water quality. Springer, Cham, pp 75–97
Xiao F, Sun J, Xu Y, Li F, Huang X, Li H, Zhao J, Huang J (2020a) Infectious SARS-CoV-2 in feces of patient with severe COVID-19. Emerg Infect Dis 26(8):1920
Xiao F, Tang M, Zheng X, Liu Y, Li X, Shan H (2020b) Evidence for gastrointestinal infection of SARS-CoV-2. Gastroenterology 158(6):1831–1833
Xu D, Zhang Z, Jin L, Chu F, Mao Y, Wang H, Liu M, Wang M, Zhang L, Gao GF, Wang FS (2005) Persistent shedding of viable SARS-CoV in urine and stool of SARS patients during the convalescent phase. Eur J Clin Microbiol Infect Dis 24(3):165–171
Yang X, Yu Y, Xu J, Shu H, Liu H, Wu Y, Zhang L, Yu Z, Fang M, Yu T, Wang Y, Shang Y (2020) Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med 8(5):475–481
Ye Y, Ellenberg RM, Graham KE, Wigginton KR (2016) Survivability, partitioning, and recovery of enveloped viruses in untreated municipal wastewater. Environ Sci Technol 50(10):5077–5085
Ye Y, Chang PH, Hartert J, Wigginton KR (2018) Reactivity of enveloped virus genome, proteins, and lipids with free chlorine and UV254. Environ Sci Technol 52(14):7698–7708
Yeo C, Kaushal S, Yeo D (2020a) Enteric involvement of coronaviruses: is fecal-oral transmission of SARS-CoV-2 possible? Lancet Gastroenterol Hepatol 5(4):335–337
Yeo C, Kaushal S, Yeo D (2020b) Enteric involvement of coronaviruses: is faecal–oral transmission of SARS-CoV-2 possible? Lancet Gastroenterol Hepatol 5(4):335–337
Yu B, Zhou Y, Huang ZW (2014) Research on simple disinfection system for medical wastewater of township hospital. Asian J Chem 26(11)
Zhang CM, Xu LM, Xu PC, Wang XC (2016) Elimination of viruses from domestic wastewater: requirements and technologies. World J Microbiol Biotechnol 32(4):69
Zhang D, Ling H, Huang X, Li J, Li W, Yi C, Zhang T, Jiang Y, He Y, Deng S, Zhang X, Qu J (2020a) Potential spreading risks and disinfection challenges of medical wastewater by the presence of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) viral RNA in septic tanks of Fangcang Hospital. Sci Total Environ 741:140445
Zhang Y, Chen C, Zhu S, Shu C, Wang D, Song J, Song Y, Zhen W, Feng Z, Wu G, Xu J, Xu W (2020b) Isolation of 2019-nCoV from a stool specimen of a laboratory-confirmed case of the coronavirus disease 2019 (COVID-19). China CDC Weekly 2(8):123–124
Zhu L, She ZG, Cheng X, Qin JJ, Zhang XJ, Cai J, Lei F, Wang H, Xie J, Wang W, Li H (2020) Association of blood glucose control and outcomes in patients with COVID-19 and pre-existing type 2 diabetes. Cell Metab 31(6):1068–1077
Acknowledgements
The author Kushneet Kaur Sodhi highly acknowledges the Hansraj college University of Delhi, and Department of Zoology University of Delhi, for their constant support and guidance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No conflicts of interest.
Informed consent
Not applicable.
Human or animals rights
The study does not relate to animals or humans.
Additional information
Editorial responsibility: Samareh Mirkia.
Rights and permissions
About this article
Cite this article
Sodhi, K.K., Singh, C.K. A systematic review on the occurrence, fate, and remediation of SARS-CoV-2 in wastewater. Int. J. Environ. Sci. Technol. 20, 8073–8086 (2023). https://doi.org/10.1007/s13762-022-04326-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13762-022-04326-1