Abstract
Introduction
Migraine is a primary headache disorder, which imposes a major burden on the sufferers. The BECOME study (Burden of migrainE in specialist headache Centers treating patients with prOphylactic treatMent failurE) attempted to characterize and assess the prevalence, burden and healthcare resource utilization of migraine patients presenting in specialized headache centers in Europe and Israel. In this paper, we will describe the patient characteristics of the Belgian headache centers.
Methods
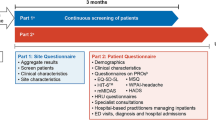
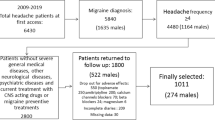
The BECOME study was a prospective, non-interventional, cross-sectional study consisting of two parts. In the first part of the study, data were collected from subjects with a diagnosis of migraine. Subsequently, patients with ≥ 4 monthly migraine days (MMD) and ≥ 1 prior preventive treatment failure (PPTF) filled out validated questionnaires to assess the burden of disease.
Results
In part 1 of the Belgian study population (N = 806), 45% of patients reported ≥ 8 MMD and 25% had failed ≥ 4 preventive treatments. In part 2 (N = 90), more than 90% of patients reported having severe impact of headache on daily life and having severe migraine-related disability. The impact was the highest for patients with ≥ 15 MMD, however, even within the patient population with < 8 MMD, the burden was significant. Almost 40% of the study population suffered from anxiety.
Conclusions
These findings in the Belgian sample of the BECOME study demonstrate the substantial burden and unmet need for the management of difficult-to-treat migraine.

Similar content being viewed by others
Data availability
Data have not been made available publicly.
References
World Health Organization. Headache disorders (2016) http://www.who.int/mediacentre/factsheets/fs277/en/
Steiner TJ et al (2018) Migraine is first cause of disability in under 50s: will health politicians now take notice? J Headache Pain 19:17
Leonardi M et al (2019) A narrative review on the burden of migraine: when the burden is the impact on people’s life. J Headache Pain 20:41
GBD (2016) Headache Collaborators (2018) Global, regional, and national burden of migraine and tension-type headache, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol 17:954–976
Ashina et al (2021) Migraine: epidemiology and systems of care. Lancet 397(10283):1485–1495
Vos T et al (2016) Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the global burden of disease study 2015. Lancet 388:1545–1602
Martelletti P et al (2018) My Migraine Voice survey: a global study of disease burden among individuals with migraine for whom preventive treatments have failed. J Headache Pain 19:115
Buse DC et al (2020) Demographics, headache features, and comorbidity profiles in relation to headache frequency in people with migraine: results of the American Migraine Prevalence and Prevention (AMPP) Study. Headache. https://doi.org/10.1111/head.13966
Andrée C et al (2011) The Eurolight project: the impact of primary headache disorders in Europe. Description of methods. J Headache Pain 12(5):541–549
Blumenfeld AM et al (2011) Disability, HRQoL and resource use among chronic and episodic migraineurs: results from the International Burden of Migraine Study (IBMS). Cephalalgia 31(3):301–315
Schwedt T et al (2021) Headache characteristics and burden from chronic migraine with medication overuse headache: cross-sectional observations from the Medication Overuse Treatment Strategy trial. Headache 61(2):351–362
Pozo-Rosich P et al (2021) Burden of migraine in patients with preventive treatment failure attending European headache specialist centers: real-world evidence from the BECOME study. Pain Ther 10:1691–1708
Herdman M et al (2011) Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res 20:1727–1736
Martin B et al (2000) Validity and reliability of the migraine-specific quality of life questionnaire (MSQ Version 2.1). Headache 40:204–215
Speck R et al (2021) Psychometric validation and meaningful within-patient change of the Migraine-Specific Quality of Life questionnaire version 2.1 electronic patient-reported outcome in patients with episodic and chronic migraine. Headache 61(3):511–526
Reilly MC et al (1993) The validity and reproducibility of a work productivity and activity impairment instrument. Pharmacoeconomics 4(5):353–365
Ford JH et al (2023) Validation and meaningful within-patient change in work productivity and activity impairment questionnaire (WPAI) for episodic or chronic migraine. J Patient Rep Outcomes 7(1):34
Kosinski M et al (2003) A six-item short-form survey for measuring headache impact: the HIT-6. Qual Life Res 12(8):963–974
Yang M et al (2011) Validation of the Headache Impact Test (HIT-6™) across episodic and chronic migraine. Cephalalgia 31(3):357–367
Stewart et al (2001) Development and testing of the Migraine Disability Assessment (MIDAS) questionnaire to assess headache-related disability. Neurology 56(6 Suppl 1):S20–S28
Stewart W et al (1999) An international study to assess reliability of the Migraine Disability Assessment (MIDAS) score. Neurology 53(5):988–994
Amoozegar F et al (2017) The prevalence of depression and the accuracy of depression screening tools in migraine patients. Gen Hosp Psychiatry 48:25–31
Martin M et al (2004) The Short-Form Headache Impact Test (HIT-6) was psychometrically equivalent in nine languages. J Clin Epidemiol 57(12):1271–1278
Bouckaert N et al (2021) An EQ-5D-5L value set for Belgium - how to value health related quality of life? Health Services Research (HSR) Brussels: Belgian Health Care Knowledge Centre (KCE). KCE Reports 342. D/2021/10.273/19.
Bocéréan C et al (2014) A validation study of the Hospital Anxiety and Depression Scale (HADS) in a large sample of French employees. BMC Psychiatry 14:354
Spinhoven P et al (1997) A validation study of the Hospital Anxiety and Depression Scale (HADS) in different groups of Dutch subjects. Psychol Med 27(2):363–370
Lucas C et al (2006) Recognition and therapeutic management of migraine in 2004, in France: results of FRAMIG 3, a French nationwide population-based survey. Headache 46(5):715–725
Lanteri-Minet M et al (2011) Quality of life impairment, disability and economic burden associated with chronic daily headache, focusing on chronic migraine with or without medication overuse: a systematic review. Cephalalgia 31(7):837–850
Park S et al (2022) The disease burden of migraine patients receiving prophylactic treatments in Korea: a population-based claims database analysis. BMC Health Serv Res 22:902
Lampl C et al (2016) Interictal burden attributable to episodic headache: findings from the Eurolight project. J Headache Pain 17:9
Shimizu T et al (2021) Disability, quality of life, productivity impairment and employer costs of migraine in the workplace. J Headache Pain 22(1):29
Korolainen MA et al (2019) Burden of migraine in Finland: health care resource use, sick-leaves and comorbidities in occupational health care. J Headache Pain 20:1–16
Begasse de Dhaem O et al (2022) Migraine in the workplace. eNeurologicalSci 27:100408
Gupta S et al (2016) Understanding the burden of idiopathic generalized epilepsy in the United States, Europe, and Brazil: an analysis from the National Health and Wellness Survey. Epilepsy Behav 55:146–156
Lanteri-Minet M et al (2005) Anxiety and depression associated with migraine: influence on migraine subjects’ disability and quality of life, and acute migraine management. Pain 118(3):319–326
Peña P et al (2009) Driving cost factors in adult outpatients with refractory epilepsy: a daily clinical practice in clinics of neurology in Spain. Epilepsy Res 83(2–3):133–143
Van Wilder L et al (2022) Belgian population norms for the EQ-5D-5L, 2018. Qual Life Res 31:527–537
Wijnen B et al (2018) A comparison of the responsiveness of EQ-5D-5L and the QOLIE-31P and mapping of QOLIE-31P to EQ-5D-5L in epilepsy. Eur J Health Econ 19:861–870
van Hezik-Wester (2022) Burden of illness in people with medically refractory epilepsy who suffer from daily to weekly seizures: 12-month follow-up of participants in the EPISODE study. Front Neurol 13:1012486
Acknowledgements
We thank the BECOME steering committee, who were instrumental in protocol development. Members of the committee: Patricia Pozo-Rosich, Christian Lucas, David P. B. Watson, Charly Gaul, Emma Ramsden and Paolo Martelletti. Principal investigator: P. Pozo-Rosich, Headache Unit, Neurology Department, Vall d’Hebron University Hospital, Barcelona, Spain.
Funding
This study was funded by Novartis Pharma AG, Basel, Switzerland. The study sponsor participated in the study design, data collection, data review, data analysis and writing of the report.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Koen Paemeleire has received personal compensation from Allergan/Abbvie, Amgen/Novartis, Eli Lilly, Lundbeck and Teva for consulting, serving on a scientific advisory board, and/or speaking and is a clinical trial investigator for Amgen/Novartis (erenumab), Eli Lilly (galcanezumab), and Autonomic Technologies Inc. (sphenopalatine ganglion stimulation). Josefin Snellman has received personal compensation from Allergan/Abbvie, Amgen/Novartis, Eli Lilly, Lundbeck, Teva, Cefaly Technology, Autonomic Technologies Inc. and Man & Science for consulting, serving on a scientific advisory board, and/or speaking and is an investigator for Eli Lilly, Novartis, Lundbeck and Teva. Shannon Ritter and Josefin Snellman are full employees of Novartis. Jan Versijpt received personal fees and nonfinancial support from Teva, personal fees from Novartis and Lundbeck, and grants and nonfinancial support from Allergan/Abbvie.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lourens, S., Van Deun, L., Peeters, I. et al. Burden of migraine in patients attending Belgian headache specialists: real-world evidence from the BECOME study. Acta Neurol Belg 123, 1495–1503 (2023). https://doi.org/10.1007/s13760-023-02280-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13760-023-02280-4