Abstract
Background
HDAC6, a structurally and functionally distinct member of the HDAC family, is an integral part of multiple cellular functions such as cell proliferation, apoptosis, senescence, DNA damage and genomic stability, all of which when deregulated contribute to carcinogenesis. Among several HDAC family members known so far, HDAC6 holds a unique position. It differs from the other HDAC family members not only in terms of its subcellular localization, but also in terms of its substrate repertoire and hence cellular functions. Recent findings have considerably expanded the research related to the substrate pool, biological functions and regulation of HDAC6. Studies in HDAC6 knockout mice highlighted the importance of HDAC6 as a cell survival player in stressful situations, making it an important anticancer target. There is ample evidence stressing the importance of HDAC6 as an anti-cancer synergistic partner of many chemotherapeutic drugs. HDAC6 inhibitors have been found to enhance the effectiveness of conventional chemotherapeutic drugs such as DNA damaging agents, proteasome inhibitors and microtubule inhibitors, thereby highlighting the importance of combination therapies involving HDAC6 inhibitors and other anti-cancer agents.
Conclusions
Here, we present a review on HDAC6 with emphasis on its role as a critical regulator of specific physiological cellular pathways which when deregulated contribute to tumorigenesis, thereby highlighting the importance of HDAC6 inhibitors as important anticancer agents alone and in combination with other chemotherapeutic drugs. We also discuss the synergistic anticancer effect of combination therapies of HDAC6 inhibitors with conventional chemotherapeutic drugs.











Similar content being viewed by others
Data availability
Not applicable.
Abbreviations
- αTAT:
-
α Tubulin acetyltransferases
- ADR:
-
Adriamycin
- Adv:
-
Adavosertib
- ALCL:
-
Anaplastic large cell lymphoma
- ALL:
-
Acute lymphoblastic leukemia
- AML:
-
Acute myeloid leukemia
- AR:
-
Androgen receptor
- BTK:
-
Bruton's tyrosine kinase
- BTZ:
-
Bortezomib
- CBP:
-
CREB-binding protein
- CC:
-
Cholangiocarcinoma
- CDK1:
-
Cyclin-dependent kinase 1
- CDKi:
-
Cyclin-dependent kinase inhibitor
- CRD-1:
-
Cell cycle regulatory domain 1
- CHK:
-
Checkpoint kinase
- CLL:
-
Chronic Lymphoid Leukemia
- COX-2:
-
Cyclooxygenase– 2
- CYLD:
-
Cylindromatosis
- DHT:
-
Dihydrotestosterone
- DLBCL:
-
Diffuse large B cell lymphoma
- ECs:
-
Endothelial cells
- EGF:
-
Epidermal growth factor
- EGFR:
-
Epidermal growth factor receptor
- ER:
-
Estrogen Receptor
- ERKs:
-
Extracellular signal-regulated kinases
- FOXP3:
-
Forkhead boxp3
- GC:
-
Gynecological cancer
- Gli1:
-
Glioma-associated oncogene homolog 1
- GPCRs:
-
G protein coupled receptors
- GR:
-
Glucocorticoid receptor
- GRK2:
-
G protein-coupled receptor kinase
- GRP:
-
Glucose-regulated protein
- GSCs:
-
Glioma stem cells
- GSK3b:
-
Glycogen synthase kinase 3
- G3BP1:
-
GTPase activating protein SH3 domain binding protein 1
- HATs:
-
Histone acetyltransferases
- HCC:
-
Hepatocellular carcinoma
- HDAC6i:
-
HDAC6 inhibitors
- HDACs:
-
Histone deacetylases
- HEK:
-
Human embryonic kidney cells
- HIF-1:
-
Hypoxia-inducible factor
- HO-1:
-
Hemeoxygenase 1
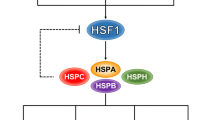
- HSF1:
-
Heat-shock factor 1
- Hsp90:
-
Heat shock protein 90
- IBC:
-
Inflammatory breast cancer
- IIp:
-
Invasion inhibitory protein
- IMiDs:
-
Immunomodulatory drugs
- MAPK:
-
Microtubule associated protein kinase
- MBC:
-
Metastatic breast cancer
- MCL:
-
Mantle cell lymphoma
- MEFs:
-
Mouse embryonic fibroblast
- MLH1:
-
MutL homolog 1
- MM:
-
Multiple myeloma
- MMP9:
-
Matrix metallopeptidase 9
- MMR:
-
Mismatch repair
- MPT0G413:
-
N-hydroxy-4-((5-(4-methoxybenzoyl)- 1H-indol-1-yl)methyl)benzamide
- MSCs:
-
Mesenchymal stem cells
- MT:
-
Microtubule
- MTOC:
-
Microtubule-organizing center
- Mtor:
-
Mammalian target of rapamycin
- NAD:
-
Nicotinamide adenine dinucleotide
- NES:
-
Nuclear export signal
- NHL:
-
Non-Hodgkin lymphoma
- NLS:
-
Nuclear localization signal
- Nrf-2:
-
Nuclear factor erythroid 2–related factor 2
- NSCLC:
-
Non-Small Cell Lung Cancer
- PCAF:
-
p300/CBP associated factor
- PDGF:
-
Platelet-derived growth factor
- PI3K:
-
Phosphoinositide 3-kinases
- Pkc:
-
Protein kinase C
- PKCz:
-
Protein kinase C isoform z
- PrEC:
-
Prostate epithelial cells
- PTEN:
-
Phosphatase and tensin homolog
- PTPN1:
-
Tyrosine-protein phosphatase non-receptor type 1
- RMS:
-
Rhabdomyosarcoma
- ROCK:
-
Rho-associated coiled-coil kinase
- ROS:
-
Reactive oxygen species
- RUNX2:
-
Runt-related transcription factor 2
- SAHA:
-
Suberoylanilidehydroxamic acid
- SIRT:
-
Sirtuins
- TMZ:
-
Temozolomide
- TPPP/p25:
-
Tubulin polymerization-promoting protein/p25
- UPR:
-
Unfolded protein response
- VEGF:
-
Vascular endothelial growth factor
- XIAP:
-
X-linked inhibitor of apoptosis
References
A. Drazic, L.M. Myklebust, R. Ree, T. Arnesen, The world of protein acetylation. Biochem Biophys Acta BBA - Proteins Proteomics 1864, 1372–1401 (2016)
C. Choudhary, C. Kumar, F. Gnad, M.L. Nielsen, M. Rehman, T.C. Walther, J.V. Olsen, M. Mann, Lysine acetylation targets protein complexes and co-regulates major cellular functions. Science 325, 834–840 (2009)
Y.C. Wang, S.E. Peterson, J.F. Loring, Protein post-translational modifications and regulation of pluripotency in human stem cells. Cell Res. 24, 143–160 (2014)
C. Seidel, M. Schnekenburger, M. Dicato, M. Diederich, Antiproliferative and proapoptotic activities of 4-hydroxybenzoic acid-based inhibitors of histone deacetylases. Cancer Lett. 343, 134–146 (2014)
S. Spange, T. Wagner, T. Heinzel, O.H. Krämer, Acetylation of non-histone proteins modulates cellular signalling at multiple levels. Int. J. Biochem. Cell Biol. 41, 185–198 (2009)
A.J. de Ruijter, A.H. van Gennip, H.N. Caron, S. Kemp, A.B. van Kuilenburg, Histone deacetylases (HDACs): characterization of the classical HDAC family. Biochem. J. 370, 737–749 (2003)
E.A. Olsen, Y.H. Kim, T.M. Kuzel, T.R. Pacheco, F.M. Foss, S. Parker, S.R. Frankel, C. Chen, J.L. Ricker, J.M. Arduino, M. Duvic, Phase IIb multicenter trial of vorinostat in patients with persistent, progressive, or treatment refractory cutaneous T-cell lymphoma. J. Clin. Oncol. 25, 3109–3115 (2007)
R.L. Piekarz, R. Frye, M. Turner, J.J. Wright, S.L. Allen, M.H. Kirschbaum, J. Zain, H.M. Prince, J.P. Leonard, L.J. Geskin, C. Reeder, D. Joske, W.D. Figg, E.R. Gardner, S.M. Steinberg, E.S. Jaffe, M. Stetler-Stevenson, S. Lade, A.T. Fojo, S.E. Bates, Phase II multi-institutional trial of the histone deacetylase inhibitor romidepsin as monotherapy for patients with cutaneous T-cell lymphoma. J. Clin. Oncol. 27, 5410–5117 (2009)
P.A. Marks, R. Breslow, Dimethyl sulfoxide to vorinostat: development of this histone deacetylase inhibitor as an anticancer drug. Nat. Biotechnol. 25, 84–90 (2007)
C. Campas-Moya, Romidepsin for the treatment of cutaneous T-cell lymphoma. Drugs Today Barc. 45, 787–795 (2009)
P.G. Richardson, R.L. Schlossman, M. Alsina, D.M. Weber, S.E. Coutre, C. Gasparetto, S. Mukhopadhyay, M.S. Ondovik, M. Khan, C.S. Paley, S. Lonial, PANORAMA 2: panobinostat in combination with bortezomib and dexamethasone in patients with relapsed and bortezomib refractory myeloma. Blood 122, 2331–2337 (2013)
C. Seidel, M. Schnekenburger, M. Dicato, M. Diesderich, Histone deacetylase 6 in health and disease. Epigenomics 7, 103–108 (2015)
S.N. Batchu, A.S. Brijmohan, A. Advani, The therapeutic hope for HDAC6 inhibitors in malignancy and chronic disease. Clin. Sci. 130, 987–1003 (2016)
Y. Liu, L. Peng, E. Seto, S. Huang, Y. Qiu, Modulation of histone deacetylase 6 (HDAC6) nuclear import and tubulin deacetylase activity through acetylation. J. Biol. Chem. 287, 29168–29174 (2012)
H. Zou, Y. Wu, M. Navre, B.C. Sang, Characterization of the two catalytic domains in histone deacetylase 6. Biochem. Biophys. Res. Commun. 341, 45–50 (2006)
C.M. Grozinger, C.A. Hassig, S.L. Schreiber, Three proteins define a class of human histone deacetylases related to yeast Hda1p. Proc. Natl. Acad. Sci. U.S.A. 96, 4868–4873 (1999)
Y. Zhang, B. Gilquin, S. Khochbin, P. Matthias, Two catalytic domains are required for protein deacetylation. J. Biol. Chem. 281, 2401–2404 (2006)
Z. Kutil, L. Skultetyova, D. Rauh, M. Meleshin, I. Snajdr, Z. Novakova, J. Mikesova, J. Pavlicek, M. Hadzima, P. Baranova, B. Havlinova, P. Majer, M. Schutkowski, C. Barinka, The unraveling of substrate specificity of histone deacetylase 6 domains using acetylome peptide microarrays and peptide libraries. FASEB J. 33, 4035–4045 (2019)
J.-Y. Wu, S. Xiang, M. Zhang, B. Fang, H. Huang, O.K. Kwon, Y. Zhao, Z. Yang, W. Bai, G. Bepler, X.M. Zhang, Histone deacetylase 6 (HDAC6) deacetylates extracellular signal-regulated kinase 1 (ERK1) and thereby stimulates ERK1 activity. J. Biol. Chem. 293, 1976–1993 (2018)
K.A. Williams, M. Zhang, S. Xiang, C. Hu, J.Y. Wu, S. Zhang, M. Ryan, A.D. Cox, C.J. Der, B. Fang, J. Koomen, E. Haura, G. Bepler, S.V. Nicosia, P. Matthias, C. Wang, W. Bai, X. Zhang, Extracellular signal-regulated kinase (ERK) phosphorylates histone deacetylase 6 (HDAC6) at serine 1035 to stimulate cell migration. J. Biol. Chem. 288, 33156–33170 (2013)
M.L. Selenica, L. Benner, S.B. Housley, B. Manchec, D.C. Lee, K.R. Nash, J. Kalin, J.A. Bergman, A. Kozikowski, M.N. Gordon, D. Morgan, Histone deacetylase 6 inhibition improves memory and reduces total tau levels in a mouse model of tau deposition. Alzheimers Res. Ther. 6, 12 (2014)
L. Zhang, S. Sheng, C. Qin, The role of HDAC6 in Alzheimer’s disease. J. Alzheimers Dis. 33, 283–295 (2013)
Y.S. Gao, C.C. Hubbert, T.P. Yao, The microtubule-associated histone deacetylase 6 (HDAC6) regulates epidermal growth factor receptor (EGFR) endocytic trafficking and degradation. J. Biol. Chem. 285, 11219–11226 (2010)
W. Liu, L.X. Fan, X. Zhou, W.E. Sweeney, E.D. Avner, X. Li, HDAC6 regulates epidermal growth factor receptor (EGFR) endocytic trafficking and degradation in renal epithelial cells. PLoS ONE 7, e49418 (2012)
Y. L. Deribe, P. Wild, A. Chandrashaker, J. Curak, M. H. H. Schmidt, Y. Kalaidzidis, N. Milutinovic, I. Kratchmarova, L. Buerkle, M. J. Fetchko, P. Schmidt, S. Kittanakom, K. R. Brown, I. Jurisica, B. Blagoev, M. Zerial, I. Stagljar, and I. Dikic, Regulation of epidermal growth factor receptor trafficking by lysine deacetylase HDAC6. Sci. Signal 2, ra84 (2009)
Y. Li, X. Zhang, R.D. Polakiewicz, T.P. Yao, M.J. Comb, HDAC6 is required for epidermal growth factor-induced beta-catenin nuclear localization. J. Biol. Chem. 283, 12686–12690 (2008)
J. Gu, D. Wang, J. Zhang, Y. Zhu, Y. Li, H. Chen, M. Shi, X. Wang, B. Shen, X. Deng, Q. Zhan, G. Wei, C. Peng, GFRα2 prompts cell growth and chemoresistance through down-regulating tumor suppressor gene PTEN via Mir-17-5p in pancreatic cancer. Cancer Lett. 380, 434–431 (2016)
Z. Meng, L.F. Jia, Y.H. Gan, PTEN activation through K163 acetylation by inhibiting HDAC6 contributes to tumour inhibition. Oncogene 35, 2333–2344 (2016)
M. Tesio, A. Trinquand, E. Macintyre, V. Asnafi, Oncogenic PTEN functions and models in T-cell malignancies. Oncogene 35, 3887–3896 (2016)
Y. Zheng, X. Yang, C. Wang, S. Zhang, Z. Wang, M. Li, Y. Wang, X. Wang, HDAC6, modulated by miR-206, promotes endometrial cancer progression through the PTEN/AKT/mTOR pathway. Sci. Rep. 10, 3576 (2020)
S.A. Wickström, K.C. Masoumi, S. Khochbin, R. Fässler, R. Massoumi, CYLD negatively regulates cell-cycle progression by inactivating HDAC6 and increasing the levels of acetylated tubulin. EMBO J. 29, 131–144 (2010)
G.I. Aldana-Masangkay, K.M. Sakamoto, The role of HDAC6 in cancer. J. Biomed. Biotechnol. 2011, 875824 (2011)
Y. Ishikawa, K. Tsunoda, M. Shibazaki, K. Takahashi, T. Akasaka, T. Masuda, C. Maesawa, Downregulation of cylindromatosis gene, CYLD, confers a growth advantage on malignant melanoma cells while negatively regulating their migration activity. Int. J. Oncol. 41, 53–60 (2012)
S.J. Haggarty, K.M. Koeller, J.C. Wong, C.M. Grozinger, S.L. Schreiber, Domain-selective small-molecule inhibitor of histone deacetylase 6 (HDAC6)-mediated tubulin deacetylation. Proc. Natl. Acad. Sci. U.S.A. 100, 4389–4394 (2003)
R. Massoumi, K. Chmielarska, K. Hennecke, A. Pfeifer, R. Fässler, Cyld inhibits tumor cell proliferation by blocking Bcl-3-dependent NF-kappaB signaling. Cell 125, 665–677 (2006)
M.J. Chuang, S.T. Wu, S.H. Tang, X.M. Lai, H.C. Lai, K.H. Hsu, K.H. Sun, G.H. Sun, S.Y. Chang, D.S. Yu, P.W. Hsiao, S.M. Huang, T.L. Cha, The HDAC inhibitor LBH589 induces ERK-dependent prometaphase arrest in prostate cancer via HDAC6 inactivation and down-regulation. PLoS ONE 8, e73401 (2013)
C. Hubbert, A. Guardiola, R. Shao, Y. Kawaguchi, A. Ito, A. Nixon, M. Yoshida, X.F. Wang, T.P. Yao, HDAC6 is a microtubule-associated deacetylase. Nature 417, 455–458 (2002)
A. Matsuyama, T. Shimazu, Y. Sumida, A. Saito, Y. Yoshimatsu, D. Seigneurin-Berny, H. Osada, Y. Komatsu, N. Nishino, S. Khochbin, S. Horinouchi, M. Yoshida, In vivo destabilization of dynamic microtubules by HDAC6-mediated deacetylation. EMBO J. 21, 6820–6831 (2002)
Y. Zhang, N. Li, C. Caron, G. Matthias, D. Hess, S. Khochbin, P. Matthias, HDAC-6 interacts with and deacetylates tubulin and microtubules in vivo. EMBO J. 22, 1168–1179 (2003)
M. Conacci-Sorrell, C. Ngouenet, R.N. Eisenman, Myc-nick: a cytoplasmic cleavage product of Myc that promotes alpha-tubulin acetylation and cell differentiation. Cell 142, 480–493 (2010)
C. Creppe, L. Malinouskaya, M.L. Volvert, M. Gillard, P. Close, O. Malaise, S. Laguesse, I. Cornez, S. Rahmouni, S. Ormenese, S. Belachew, B. Malgrange, J.P. Chapelle, U. Siebenlist, G. Moonen, A. Chariot, L. Nguyen, Elongator controls the migration and differentiation of cortical neurons through acetylation of alpha-tubulin. Cell 136, 551–564 (2009)
S.W. L’Hernault, J.L. Rosenbaum, Chlamydomonas alpha-tubulin is posttranslationally modified in the flagella during flagellar assembly. J. Cell Biol. 97, 258–263 (1983)
N. Ohkawa, S. Sugisaki, E. Tokunaga, K. Fujitani, T. Hayasaka, M. Setou, K. Inokuchi, N-acetyltransferase ARD1-NAT1 regulates neuronal dendritic development. Genes Cells 13, 1171–1183 (2008)
X. Zhang, Z. Yuan, Y. Zhang, S. Yong, A. Salas-Burgos, J. Koomen, N. Olashaw, J.T. Parsons, X.J. Yang, S.R. Dent, T.P. Yao, W.S. Lane, E. Seto, HDAC6 modulates cell motility by altering the acetylation level of cortactin. Mol. Cell 27, 197–213 (2007)
H. Wu, J.T. Parsons, Cortactin, an 80/85-kilodalton pp60src substrate, is a filamentous actin-binding protein enriched in the cell cortex. J. Cell Biol. 120, 1417–1426 (1993)
N.S. Bryce, E.S. Clark, J.L. Leysath, J.D. Currie, D.J. Webb, A.M. Weaver, Cortactin promotes cell motility by enhancing lamellipodial persistence. Curr. Biol. 15, 1276–1285 (2005)
D. Kaluza, J. Kroll, S. Gesierich, T.P. Yao, R.A. Boon, E. Hergenreider, M. Tjwa, L. Rössig, E. Seto, H.G. Augustin, A.M. Zeiher, S. Dimmeler, C. Urbich, Class IIb HDAC6 regulates endothelial cell migration and angiogenesis by deacetylation of cortactin. EMBO J. 30, 4142–4156 (2011)
V. Lafarga, I. Aymerich, O. Tapia, F. Mayor, P. Penela, A novel GRK2/HDAC6 interaction modulates cell spreading and motility. EMBO J. 31, 856–869 (2012)
P. Penela, V. Lafarga, O. Tapia, V. Rivas, L. Nogués, E. Lucas, R. Vila-Bedmar, C. Murga, and F. Mayor, Roles of GRK2 in cell signaling beyond GPCR desensitization: GRK2-HDAC6 interaction modulates cell spreading and motility. Sci. Signal 5, pt3 (2012)
H.H. Chuang, M.S. Huang, P.H. Wang, Y.P. Liu, M. Hsiao, C.J. Yang, Pin1 Is Involved in HDAC6-mediated Cancer Cell Motility. Int. J. Med. Sci. 15, 1573–1581 (2018)
H.H. Chuang, J.F. Hsu, H.L. Chang, P.H. Wang, P.J. Wei, D.W. Wu, M.S. Huang, M. Hsiao, C.J. Yang, Pin1 coordinates HDAC6 upregulation with cell migration in lung cancer cells. Int. J. Med. Sci. 17, 2635–2643 (2020)
J. Liu, W. Luan, Y. Zhang, J. Gu, Y. Shi, Y. Yang, Z. Feng, F. Qi, HDAC6 interacts with PTPN1 to enhance melanoma cells progression. Biochem. Biophys. Res. Commun. 495, 2630–2636 (2018)
C. Featherstone, S.P. Jackson, Ku, a DNA repair protein with multiple cellular functions? Mutat. Res. 434, 3–15 (1999)
H.Y. Cohen, S. Lavu, K.J. Bitterman, B. Hekking, T.A. Imahiyerobo, C. Miller, R. Frye, H. Ploegh, B.M. Kessler, D.A. Sinclair, Acetylation of the C terminus of Ku70 by CBP and PCAF controls Bax-mediated apoptosis. Mol. Cell 13, 627–638 (2004)
C. Subramanian, J.A. Jarzembowski, A.W. Opipari, V.P. Castle, R.P. Kwok, HDAC6 deacetylates Ku70 and regulates Ku70-Bax binding in neuroblastoma. Neoplasia 13, 726–734 (2011)
E. Kerr, C. Holohan, K.M. McLaughlin, J. Majkut, S. Dolan, K. Redmond, J. Riley, K. McLaughlin, I. Stasik, M. Crudden, S. Van Schaeybroeck, C. Fenning, R. O’Connor, P. Kiely, M. Sgobba, D. Haigh, P.G. Johnston, D.B. Longley, Identification of an acetylation-dependant Ku70/FLIP complex that regulates FLIP expression and HDAC inhibitor-induced apoptosis. Cell Death Differ. 19, 1317–1327 (2012)
H. Wang, M.P. Holloway, L. Ma, Z.A. Cooper, M. Riolo, A. Samkari, K.S. Elenitoba-Johnson, Y.E. Chin, R.A. Altura, Acetylation directs survivin nuclear localization to repress STAT3 oncogenic activity. J. Biol. Chem. 285, 36129–36137 (2010)
M.T. Riolo, Z.A. Cooper, M.P. Holloway, Y. Cheng, C. Bianchi, E. Yakirevich, L. Ma, Y.E. Chin, R.A. Altura, Histone deacetylase 6 (HDAC6) deacetylates survivin for its nuclear export in breast cancer. J. Biol. Chem. 287, 10885–10893 (2012)
C. Boyault, Y. Zhang, S. Fritah, C. Caron, B. Gilquin, S. H. Kwon, C. Garrido, T. P. Yao, C. Vourc’h, P. Matthias, and S. Khochbin, HDAC6 controls major cell response pathways to cytotoxic accumulation of protein aggregates. Genes Dev. 21, 2172–2181 (2007)
Y. Kawaguchi, J.J. Kovacs, A. McLaurin, J.M. Vance, A. Ito, T.P. Yao, The deacetylase HDAC6 regulates aggresome formation and cell viability in response to misfolded protein stress. Cell 115, 727–738 (2003)
C. Boyault, B. Gilquin, Y. Zhang, V. Rybin, E. Garman, W. Meyer-Klaucke, P. Matthias, C.W. Müller, S. Khochbin, HDAC6-p97/VCP controlled polyubiquitin chain turnover. EMBO J. 25, 3357–3366 (2006)
A. Iwata, B.E. Riley, J.A. Johnston, R.R. Kopito, HDAC6 and microtubules are required for autophagic degradation of aggregated huntingtin. J. Biol. Chem. 280, 40282–40292 (2005)
J.A. Olzmann, L.S. Chin, Parkin-mediated K63-linked polyubiquitination: a signal for targeting misfolded proteins to the aggresome-autophagy pathway. Autophagy 4, 85–87 (2008)
K.P. Liu, D. Zhou, D.Y. Ouyang, L.H. Xu, Y. Wang, L.X. Wang, H. Pan, X.H. He, LC3B-II deacetylation by histone deacetylase 6 is involved in serum-starvation-induced autophagic degradation. Biochem. Biophys. Res. Commun. 441, 970–975 (2013)
S. Pankiv, T.H. Clausen, T. Lamark, A. Brech, J.A. Bruun, H. Outzen, A. Øvervatn, G. Bjørkøy, T. Johansen, p62/SQSTM1 binds directly to Atg8/LC3 to facilitate degradation of ubiquitinated protein aggregates by autophagy. J. Biol. Chem. 282, 24131–24145 (2007)
C. Fusco, L. Micale, M. Egorov, M. Monti, E.V. D’Addetta, B. Augello, F. Cozzolino, A. Calcagnì, A. Fontana, R.S. Polishchuk, G. Didelot, A. Reymond, P. Pucci, G. Merla, The E3-ubiquitin ligase TRIM50 interacts with HDAC6 and p62, and promotes the sequestration and clearance of ubiquitinated proteins into the aggresome. PLoS ONE 7, e40440 (2012)
J.Y. Lee, H. Koga, Y. Kawaguchi, W. Tang, E. Wong, Y.S. Gao, U.B. Pandey, S. Kaushik, E. Tresse, J. Lu, J.P. Taylor, A.M. Cuervo, T.P. Yao, HDAC6 controls autophagosome maturation essential for ubiquitin-selective quality-control autophagy. EMBO J. 29, 969–980 (2010)
W.J. Liu, L. Ye, W.F. Huang, L.J. Guo, Z.G. Xu, H.L. Wu, C. Yang, H.F. Liu, p62 links the autophagy pathway and the ubiqutin-proteasome system upon ubiquitinated protein degradation. Cell Mol. Biol. Lett. 21, 29 (2016)
G. Bjørkøy, T. Lamark, A. Brech, H. Outzen, M. Perander, A. Overvatn, H. Stenmark, T. Johansen, p62/SQSTM1 forms protein aggregates degraded by autophagy and has a protective effect on huntingtin-induced cell death. J. Cell Biol. 171, 603–614 (2005)
M.L. Seibenhener, J.R. Babu, T. Geetha, H.C. Wong, N.R. Krishna, M.W. Wooten, Sequestosome 1/p62 is a polyubiquitin chain binding protein involved in ubiquitin proteasome degradation. Mol. Cell Biol. 24, 8055–8068 (2004)
C. Dai, L. Whitesell, A.B. Rogers, S. Lindquist, Heat shock factor 1 is a powerful multifaceted modifier of carcinogenesis. Cell 130, 1005–1018 (2007)
P. Bali, M. Pranpat, J. Bradner, M. Balasis, W. Fiskus, F. Guo, K. Rocha, S. Kumaraswamy, S. Boyapalle, P. Atadja, E. Seto, K. Bhalla, Inhibition of histone deacetylase 6 acetylates and disrupts the chaperone function of heat shock protein 90: a novel basis for antileukemia activity of histone deacetylase inhibitors. J. Biol. Chem. 280, 26729–26734 (2005)
B.T. Scroggins, K. Robzyk, D. Wang, M.G. Marcu, S. Tsutsumi, K. Beebe, R.J. Cotter, S. Felts, D. Toft, L. Karnitz, N. Rosen, L. Neckers, An acetylation site in the middle domain of Hsp90 regulates chaperone function. Mol. Cell 25, 151–159 (2007)
J.J. Kovacs, P.J. Murphy, S. Gaillard, X. Zhao, J.T. Wu, C.V. Nicchitta, M. Yoshida, D.O. Toft, W.B. Pratt, T.P. Yao, HDAC6 regulates Hsp90 acetylation and chaperone-dependent activation of glucocorticoid receptor. Mol. Cell 18, 601–607 (2005)
P.J. Murphy, Y. Morishima, J.J. Kovacs, T.P. Yao, W.B. Pratt, Regulation of the dynamics of hsp90 action on the glucocorticoid receptor by acetylation/deacetylation of the chaperone. J. Biol. Chem. 280, 33792–33799 (2005)
C. Caron, C. Boyault, S. Khochbin, Regulatory cross-talk between lysine acetylation and ubiquitination: role in the control of protein stability. BioEssays 27, 408–415 (2005)
D.R. Hurst, A. Mehta, B.P. Moore, P.A. Phadke, W.J. Meehan, M.A. Accavitti, L.A. Shevde, J.E. Hopper, Y. Xie, D.R. Welch, R.S. Samant, Breast cancer metastasis suppressor 1 (BRMS1) is stabilized by the Hsp90 chaperone. Biochem. Biophys. Res. Commun. 348, 1429–1435 (2006)
X. Kong, Z. Lin, D. Liang, D. Fath, N. Sang, J. Caro, Histone deacetylase inhibitors induce VHL and ubiquitin-independent proteasomal degradation of hypoxia-inducible factor 1alpha. Mol. Cell Biol. 26, 2019–2028 (2006)
J.J. Westendorf, S.K. Zaidi, J.E. Cascino, R. Kahler, A.J. van Wijnen, J.B. Lian, M. Yoshida, G.S. Stein, X. Li, Runx2 (Cbfa1, AML-3) interacts with histone deacetylase 6 and represses the p21(CIP1/WAF1) promoter. Mol. Cell Biol. 22, 7982–7992 (2002)
Z. Yu, W. Zhang, B.C. Kone, Histone deacetylases augment cytokine induction of the iNOS gene. J. Am. Soc. Nephrol. 13, 2009–2017 (2002)
D. Girdwood, D. Bumpass, O.A. Vaughan, A. Thain, L.A. Anderson, A.W. Snowden, E. Garcia-Wilson, N.D. Perkins, R.T. Hay, P300 transcriptional repression is mediated by SUMO modification. Mol. Cell 11, 1043 (2003)
L. Ling, P.E. Lobie, RhoA/ROCK activation by growth hormone abrogates p300/histone deacetylase 6 repression of Stat5-mediated transcription. J. Biol. Chem. 279, 32737 (2004)
H. Ma, C. Nguyen, K.S. Lee, M. Kahn, Differential roles for the coactivators CBP and p300 on TCF/beta-catenin-mediated survivin gene expression. Oncogene 24, 3619–3631 (2005)
Y. Han, H.M. Jeong, Y.H. Jin, Y.J. Kim, H.G. Jeong, C.Y. Yeo, K.Y. Lee, Acetylation of histone deacetylase 6 by p300 attenuates its deacetylase activity. Biochem. Biophys. Res. Commun. 383, 88–92 (2009)
I. Fernandes, Y. Bastien, T. Wai, K. Nygard, R. Lin, O. Cormier, H.S. Lee, F. Eng, N.R. Bertos, N. Pelletier, S. Mader, V.K. Han, X.J. Yang, J.H. White, Ligand-dependent nuclear receptor corepressor LCoR functions by histone deacetylase-dependent and -independent mechanisms. Mol. Cell 11, 139–150 (2003)
J.M. Amann, J. Nip, D.K. Strom, B. Lutterbach, H. Harada, N. Lenny, J.R. Downing, S. Meyers, S.W. Hiebert, ETO, a target of t(8;21) in acute leukemia, makes distinct contacts with multiple histone deacetylases and binds mSin3A through its oligomerization domain. Mol. Cell Biol. 21, 6470–6483 (2001)
A. Palijan, I. Fernandes, Y. Bastien, L. Tang, M. Verway, M. Kourelis, L.E. Tavera-Mendoza, Z. Li, V. Bourdeau, S. Mader, X.J. Yang, J.H. White, Function of histone deacetylase 6 as a cofactor of nuclear receptor coregulator LCoR. J. Biol. Chem. 284, 30264–30274 (2009)
R. Winkler, V. Benz, M. Clemenz, M. Bloch, A. Foryst-Ludwig, S. Wardat, N. Witte, M. Trappiel, P. Namsolleck, K. Mai, J. Spranger, G. Matthias, T. Roloff, O. Truee, K. Kappert, M. Schupp, P. Matthias, U. Kintscher, Histone deacetylase 6 (HDAC6) is an essential modifier of glucocorticoid-induced hepatic gluconeogenesis. Diabetes 61, 513–523 (2012)
J.M. Solomon, R. Pasupuleti, L. Xu, T. McDonagh, R. Curtis, P.S. DiStefano, L.J. Huber, Inhibition of SIRT1 catalytic activity increases p53 acetylation but does not alter cell survival following DNA damage. Mol. Cell Biol. 26, 28–38 (2006)
C. Blackburn, C. Barrett, J. Chin, K. Garcia, K. Gigstad, A. Gould, J. Gutierrez, S. Harrison, K. Hoar, C. Lynch, R.S. Rowland, C. Tsu, J. Ringeling, H. Xu, Potent histone deacetylase inhibitors derived from 4-(aminomethyl)-N-hydroxybenzamide with high selectivity for the HDAC6 isoform. J. Med. Chem. 56, 7201–7211 (2013)
S.-Y. Park, S. Phorl, S. Jung, K. Sovannarith, S. Lee, S. Noh, M. Han, R. Naskar, J.-Y. Kim, Y.-J. Choi, J.-Y. Lee, HDAC6 deficiency induces apoptosis in mesenchymal stem cells through p53 K120 acetylation. Biochem. Biophys. Res. Commun. 494, 51–56 (2017)
M. Zhang, C. Hu, N. Moses, J. Haakenson, S. Xiang, D. Quan, B. Fang, Z. Yang, W. Bai, G. Bepler, G.M. Li, X.M. Zhang, HDAC6 regulates DNA damage response via deacetylating MLH1. J. Biol. Chem. 294, 5813–5826 (2019)
T. Ozaki, D. Wu, H. Sugimoto, H. Nagase, A. Nakagawara, Runt-related transcription factor 2 (RUNX2) inhibits p53-dependent apoptosis through the collaboration with HDAC6 in response to DNA damage. Cell Death Dis. 4, e610 (2013)
W. Yang, Y. Liu, R. Gao, H. Yu, T. Sun, HDAC6 inhibition induces glioma stem cells differentiation and enhances cellular radiation sensitivity through the SHH/Gli1 signaling pathway. Cancer Lett. 415, 164–176 (2018)
G.W. Kim, D.H. Lee, S.K. Yeon, Y.H. Jeon, J. Yoo, S.W. Lee, S.H. Kwon, Temozolomide-resistant Glioblastoma Depends on HDAC6 Activity Through Regulation of DNA Mismatch Repair. Anticancer Res. 39, 6731–6741 (2019)
O.H. Krämer, S. Mahboobi, A. Sellmer, Drugging the HDAC6-HSP90 interplay in malignant cells. Trends Pharmacol. Sci. 35, 501–509 (2014)
Y. Wu, S.W. Song, J. Sun, J.M. Bruner, G.N. Fuller, W. Zhang, IIp45 inhibits cell migration through inhibition of HDAC6. J. Biol. Chem. 285, 3554–3560 (2010)
N. Tokési, A. Lehotzky, I. Horváth, B. Szabó, J. Oláh, P. Lau, J. Ovádi, Drugging the HDAC6-HSP90 interplay in malignant cells. J. Biol. Chem. 285, 17896–17906 (2010)
J. Zhou, C.C. Vos, A. Gjyrezi, M. Yoshida, F.R. Khuri, F. Tamanoi, P. Giannakakou, The protein farnesyltransferase regulates HDAC6 activity in a microtubule-dependent manner. J. Biol. Chem. 284, 9648–9655 (2009)
S. Chen, G.C. Owens, H. Makarenkova, D.B. Edelman, HDAC6 regulates mitochondrial transport in hippocampal neurons. PLoS ONE 5, e10848 (2010)
K. Leroy, Z. Yilmaz, J.P. Brion, Increased level of active GSK-3beta in Alzheimer’s disease and accumulation in argyrophilic grains and in neurones at different stages of neurofibrillary degeneration. Neuropathol. Appl. Neurobiol. 33, 43–55 (2007)
E.N. Pugacheva, S.A. Jablonski, T.R. Hartman, E.P. Henske, E.A. Golemis, HEF1-dependent Aurora A activation induces disassembly of the primary cilium. Cell 129, 1351–1363 (2007)
M. Watabe, T. Nakaki, Protein kinase CK2 regulates the formation and clearance of aggresomes in response to stress. J. Cell Sci. 124, 1519–1532 (2011)
J. Zhu, C.B. Coyne, S.N. Sarkar, PKC alpha regulates Sendai virus-mediated interferon induction through HDAC6 and β-catenin. EMBO J. 30, 4838–4849 (2011)
Y. Du, M.L. Seibenhener, J. Yan, J. Jiang, M.C. Wooten, aPKC phosphorylation of HDAC6 results in increased deacetylation activity. PLoS ONE 10, e0123191 (2015)
A.V. Schofield, C. Gamell, R. Suryadinata, B. Sarcevic, O. Bernard, Tubulin polymerization promoting protein 1 (Tppp1) phosphorylation by Rho-associated coiled-coil kinase (rock) and cyclin-dependent kinase 1 (Cdk1) inhibits microtubule dynamics to increase cell proliferation. J. Biol. Chem. 288, 7907–7917 (2013)
A.V. Schofield, C. Gamell, O. Bernard, Tubulin polymerization promoting protein 1 (TPPP1) increases β-catenin expression through inhibition of HDAC6 activity in U2OS osteosarcoma cells. Biochem. Biophys. Res. Commun. 436, 571–577 (2013)
N.O. Deakin, C.E. Turner, Paxillin inhibits HDAC6 to regulate microtubule acetylation, Golgi structure, and polarized migration. J. Cell Biol. 206, 395–413 (2014)
N. Kasai, A. Kadeer, M. Kajita, S. Saitoh, S. Ishikawa, T. Maruyama, Y. Fujita, The paxillin-plectin-EPLIN complex promotes apical elimination of RasV12-transformed cells by modulating HDAC6-regulated tubulin acetylation. Sci. Rep. 8, 2097 (2018)
Tala, X. Sun, J. Chen, L. Zhang, N. Liu, J. Zhou, D. Li, and M. Liu, Microtubule stabilization by Mdp3 is partially attributed to its modulation of HDAC6 in addition to its association with tubulin and microtubules. PLoS One 9, e90932 (2014)
L.M. Salemi, A.W. Almawi, K.J. Lefebvre, C. Schild-Poulter, Aggresome formation is regulated by RanBPM through an interaction with HDAC6. Biol. Open 3, 418–430 (2014)
A. P. Mansini, M. J. Lorenzo Pisarello, K. M. Thelen, M. Cruz-Reyes, E. Peixoto, S. Jin, B. N. Howard, C. E. Trussoni, G. B. Gajdos, N. F. LaRusso, M. J. Perugorria, J. M. Banales, and S. A. Gradilone, MicroRNA (miR)-433 and miR-22 dysregulations induce histone-deacetylase-6 overexpression and ciliary loss in cholangiocarcinoma. Hepatol. Baltim. Md. 68, 561–573 (2018)
T. Lwin, X. Zhao, F. Cheng, X. Zhang, A. Huang, B. Shah, Y. Zhang, L.C. Moscinski, Y.S. Choi, A.P. Kozikowski, J.E. Bradner, W.S. Dalton, E. Sotomayor, J. Tao, A microenvironment-mediated c-Myc/miR-548m/HDAC6 amplification loop in non-Hodgkin B cell lymphomas. J. Clin. Invest. 123, 4612–4626 (2013)
K. Okuda, A. Ito, T. Uehara, Regulation of histone deacetylase 6 activity via S-nitrosylation. Biol. Pharm. Bull. 38, 1434–1437 (2015)
C.A. Bradbury, F.L. Khanim, R. Hayden, C.M. Bunce, D.A. White, M.T. Drayson, C. Craddock, B.M. Turner, Histone deacetylases in acute myeloid leukaemia show a distinctive pattern of expression that changes selectively in response to deacetylase inhibitors. Leukemia 19, 1751–1759 (2005)
B. Hackanson, L. Rimmele, M. Benkißer, M. Abdelkarim, M. Fliegauf, M. Jung, M. Lübbert, HDAC6 as a target for antileukemic drugs in acute myeloid leukemia. Leuk. Res. 36, 1055–1062 (2012)
S.L. Zhang, H.Y. Zhu, B.Y. Zhou, Y. Chu, J.R. Huo, Y.Y. Tan, D.L. Liu, Histone deacetylase 6 is overexpressed and promotes tumor growth of colon cancer through regulation of the MAPK/ERK signal pathway. Onco. Targets Ther. 12, 2409–2419 (2019)
S. Saji, M. Kawakami, S. Hayashi, N. Yoshida, M. Hirose, S. Horiguchi, A. Itoh, N. Funata, S.L. Schreiber, M. Yoshida, M. Toi, Significance of HDAC6 regulation via estrogen signaling for cell motility and prognosis in estrogen receptor-positive breast cancer. Oncogene 24, 4531–4539 (2005)
T. Sakuma, K. Uzawa, T. Onda, M. Shiiba, H. Yokoe, T. Shibahara, H. Tanzawa, Aberrant expression of histone deacetylase 6 in oral squamous cell carcinoma. Int. J. Oncol. 29, 117–124 (2006)
Y.S. Lee, K.H. Lim, X. Guo, Y. Kawaguchi, Y. Gao, T. Barrientos, P. Ordentlich, X.F. Wang, C.M. Counter, T.P. Yao, The cytoplasmic deacetylase HDAC6 is required for efficient oncogenic tumorigenesis. Cancer Res. 68, 7561–7569 (2008)
P. Putcha, J. Yu, R. Rodriguez-Barrueco, L. Saucedo-Cuevas, P. Villagrasa, E. Murga-Penas, S.N. Quayle, M. Yang, V. Castro, D. Llobet-Navas, D. Birnbaum, P. Finetti, W.A. Woodward, F. Bertucci, M.L. Alpaugh, A. Califano, J. Silva, HDAC6 activity is a non-oncogene addiction hub for inflammatory breast cancers. Breast Cancer Res. 17, 149 (2015)
A. Keremu, A. Aimaiti, Z. Liang, X. Zou, Role of the HDAC6/STAT3 pathway in regulating PD-L1 expression in osteosarcoma cell lines. Cancer Chemother. Pharmacol. 83, 255–264 (2019)
C.S. Chen, S.C. Weng, P.H. Tseng, H.P. Lin, Histone acetylation-independent effect of histone deacetylase inhibitors on Akt through the reshuffling of protein phosphatase 1 complexes. J. Biol. Chem. 280, 38879–38887 (2005)
I.A. Kim, M. No, J.M. Lee, J.H. Shin, J.S. Oh, E.J. Choi, I.H. Kim, P. Atadja, E.J. Bernhard, Epigenetic modulation of radiation response in human cancer cells with activated EGFR or HER-2 signaling: potential role of histone deacetylase 6. Radiother. Oncol. 92, 125–132 (2009)
S.C. Tien, Z.F. Chang, Oncogenic Shp2 disturbs microtubule regulation to cause HDAC6-dependent ERK hyperactivation. Oncogene 33, 2938–2946 (2014)
Q.Y. Zhu, Z. Wang, C. Ji, L. Cheng, Y.L. Yang, J. Ren, Y.H. Jin, Q.J. Wang, X.J. Gu, Z.G. Bi, G. Hu, Y. Yang, C6-ceramide synergistically potentiates the anti-tumor effects of histone deacetylase inhibitors via AKT dephosphorylation and α-tubulin hyperacetylation both in vitro and in vivo. Cell Death Dis. 2, e117 (2011)
S. Aoyagi, T.K. Archer, Modulating molecular chaperone Hsp90 functions through reversible acetylation. Trends Cell Biol. 15, 565–567 (2005)
S. Tsutsumi, K. Beebe, L. Neckers, Impact of heat-shock protein 90 on cancer metastasis. Future Oncol. 5, 679–688 (2009)
Y.Z. Gu, Q. Xue, Y.J. Chen, G.H. Yu, M.D. Qing, Y. Shen, M.Y. Wang, Q. Shi, X.G. Zhang, Different roles of PD-L1 and FasL in immunomodulation mediated by human placenta-derived mesenchymal stem cells. Hum. Immunol. 74, 267–276 (2013)
J. Wen, J. Fu, Y. Ling, W. Zhang, MIIP accelerates epidermal growth factor receptor protein turnover and attenuates proliferation in non-small cell lung cancer. Oncotarget 7, 9118–9134 (2016)
S.L. Zhang, X. Du, L.N. Tan, F.H. Deng, B.Y. Zhou, H.J. Zhou, H.Y. Zhu, Y. Chu, D.L. Liu, Y.Y. Tan, SET7 interacts with HDAC6 and suppresses the development of colon cancer through inactivation of HDAC6. Am. J. Transl. Res. 12, 602–611 (2020)
F. Ikeda, I. Dikic, CYLD in ubiquitin signaling and tumor pathogenesis. Cell 125, 643–645 (2006)
M. Bazzaro, Z. Lin, A. Santillan, M.K. Lee, M.C. Wang, K.C. Chan, R.E. Bristow, R. Mazitschek, J. Bradner, R.B. Roden, Ubiquitin proteasome system stress underlies synergistic killing of ovarian cancer cells by bortezomib and a novel HDAC6 inhibitor. Clin. Cancer Res. 14, 7340–7347 (2008)
Y. Zilberman, C. Ballestrem, L. Carramusa, R. Mazitschek, S. Khochbin, A. Bershadsky, Regulation of microtubule dynamics by inhibition of the tubulin deacetylase HDAC6. J. Cell Sci. 122, 3531–3541 (2009)
L. Zhang, N. Liu, S. Xie, X. He, J. Zhou, M. Liu, D. Li, HDAC6 regulates neuroblastoma cell migration and may play a role in the invasion process. Cancer Biol. Ther. 15, 1561–1570 (2014)
M. Rey, M. Irondelle, F. Waharte, F. Lizarraga, P. Chavrier, HDAC6 is required for invadopodia activity and invasion by breast tumor cells. Eur. J. Cell Biol. 90, 128–135 (2011)
G.P. Gupta, J. Massagué, Cancer metastasis: building a framework. Cell 127, 679–695 (2006)
K. Kanno, S. Kanno, H. Nitta, N. Uesugi, T. Sugai, T. Masuda, G. Wakabayashi, C. Maesawa, Overexpression of histone deacetylase 6 contributes to accelerated migration and invasion activity of hepatocellular carcinoma cells. Oncol. Rep. 28, 867–873 (2012)
K. Azuma, T. Urano, K. Horie-Inoue, S. Hayashi, R. Sakai, Y. Ouchi, S. Inoue, Association of estrogen receptor alpha and histone deacetylase 6 causes rapid deacetylation of tubulin in breast cancer cells. Cancer Res. 69, 2935–2940 (2009)
T.Q. Pham, K. Robinson, L. Xu, M.N. Pavlova, S.X. Skapek, E.Y. Chen, HDAC6 promotes growth, migration/invasion, and self-renewal of rhabdomyosarcoma. Oncogene 40, 578–591 (2021)
D. Li, S. Xie, Y. Ren, L. Huo, J. Gao, D. Cui, M. Liu, J. Zhou, Microtubule-associated deacetylase HDAC6 promotes angiogenesis by regulating cell migration in an EB1-dependent manner. Protein Cell 2, 150–160 (2011)
J.H. Park, S.H. Kim, M.C. Choi, J. Lee, D.Y. Oh, S.A. Im, Y.J. Bang, T.Y. Kim, Class II histone deacetylases play pivotal roles in heat shock protein 90-mediated proteasomal degradation of vascular endothelial growth factor receptors. Biochem. Biophys. Res. Commun. 368, 318–322 (2008)
D.Z. Qian, S.K. Kachhap, S.J. Collis, H.M. Verheul, M.A. Carducci, P. Atadja, R. Pili, Class II histone deacetylases are associated with VHL-independent regulation of hypoxia-inducible factor 1 alpha. Cancer Res. 66, 8814–8821 (2006)
H.W. Ryu, H.R. Won, D.H. Lee, S.H. Kwon, HDAC6 regulates sensitivity to cell death in response to stress and post-stress recovery. Cell Stress Chaperones 22, 253–261 (2017)
Z. Lv, X. Weng, C. Du, C. Zhang, H. Xiao, X. Cai, S. Ye, J. Cheng, C. Ding, H. Xie, L. Zhou, J. Wu, S. Zheng, Downregulation of HDAC6 promotes angiogenesis in hepatocellular carcinoma cells and predicts poor prognosis in liver transplantation patients. Mol. Carcinog. 55, 1024–1033 (2016)
M. Sharma, P. Jha, P. Verma, M. Chopra, Combined comparative molecular field analysis, comparative molecular similarity indices analysis, molecular docking and molecular dynamics studies of histone deacetylase 6 inhibitors. Chem. Biol. Drug Des. 93, 910–925 (2019)
J. Jochems, J. Boulden, B.G. Lee, J.A. Blendy, M. Jarpe, R. Mazitschek, J.H. Van Duzer, S. Jones, O. Berton, Antidepressant-like properties of novel HDAC6-selective inhibitors with improved brain bioavailability. Neuropsychopharmacol. Off. Publ. Am. Coll. Neuropsychopharmacol. 39, 389–400 (2014)
J.-H. Lee, A. Mahendran, Y. Yao, L. Ngo, G. Venta-Perez, M.L. Choy, N. Kim, W.-S. Ham, R. Breslow, P.A. Marks, Development of a histone deacetylase 6 inhibitor and its biological effects. Proc. Natl. Acad. Sci. U. S. A. 110, 15704–15709 (2013)
J.H. Kalin, J.A. Bergman, Development and therapeutic implications of selective histone deacetylase 6 inhibitors. J. Med. Chem. 56, 6297–6313 (2013)
D.V. Smil, S. Manku, Y.A. Chantigny, S. Leit, A. Wahhab, T.P. Yan, M. Fournel, C. Maroun, Z. Li, A.-M. Lemieux, A. Nicolescu, J. Rahil, S. Lefebvre, A. Panetta, J.M. Besterman, R. Déziel, Novel HDAC6 isoform selective chiral small molecule histone deacetylase inhibitors. Bioorg. Med. Chem. Lett. 19, 688–692 (2009)
Y. Chen, M. Lopez-Sanchez, D.N. Savoy, D.D. Billadeau, G.S. Dow, A.P. Kozikowski, A series of potent and selective, triazolylphenyl-based histone deacetylases inhibitors with activity against pancreatic cancer cells and Plasmodium falciparum. J. Med. Chem. 51, 3437–3448 (2008)
A.P. Kozikowski, S. Tapadar, D.N. Luchini, K.H. Kim, D.D. Billadeau, Use of the nitrile oxide cycloaddition (NOC) reaction for molecular probe generation: a new class of enzyme selective histone deacetylase inhibitors (HDACIs) showing picomolar activity at HDAC6. J. Med. Chem. 51, 4370–4373 (2008)
E.S. Inks, B.J. Josey, S.R. Jesinkey, C.J. Chou, A novel class of small molecule inhibitors of HDAC6. ACS Chem. Biol. 7, 331–339 (2012)
C.-W. Yu, P.-T. Chang, L.-W. Hsin, J.-W. Chern, Quinazolin-4-one derivatives as selective histone deacetylase-6 inhibitors for the treatment of Alzheimer’s disease. J. Med. Chem. 56, 6775–6791 (2013)
V. Zuco, M. De Cesare, R. Cincinelli, R. Nannei, C. Pisano, N. Zaffaroni, F. Zunino, Synergistic Antitumor Effects of Novel HDAC Inhibitors and Paclitaxel In Vitro and In Vivo. PLoS ONE 6, e29085 (2011)
A. M. Tsimberidou, P. A. Beer, C. A. Cartwright, C. Haymaker, H. H. Vo, S. Kiany, A. R. L. Cecil, J. Dow, K. Haque, F. A. Silva, L. Coe, H. Berryman, E. A. Bone, G. M. Nogueras-Gonzalez, D. Vining, H. McElwaine-Johnn, and I. I. Wistuba, Preclinical development and First-in-human study of KA2507, a selective and potent inhibitor of histone deacetylase 6, for patients with refractory solid tumors. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 27, 3584–3594 (2021)
H. Song, X. Niu, J. Quan, Y. Li, L. Yuan, J. Wang, C. Ma, E. Ma, Discovery of specific HDAC6 inhibitor with anti-metastatic effects in pancreatic cancer cells through virtual screening and biological evaluation. Bioorganic Chem. 97, 103679 (2020)
P. Linciano, L. Pinzi, S. Belluti, U. Chianese, R. Benedetti, D. Moi, L. Altucci, S. Franchini, C. Imbriano, C. Sorbi, G. Rastelli, Inhibitors of histone deacetylase 6 based on a novel 3-hydroxy-isoxazole zinc binding group. J. Enzyme Inhib. Med. Chem. 36, 2080–2086 (2021)
N. Relitti, A.P. Saraswati, G. Chemi, M. Brindisi, S. Brogi, D. Herp, K. Schmidtkunz, F. Saccoccia, G. Ruberti, C. Ulivieri, F. Vanni, F. Sarno, L. Altucci, S. Lamponi, M. Jung, S. Gemma, S. Butini, G. Campiani, Synthesis, molecular modeling studies and biological investigation. Eur. J. Med. Chem. 212, 112998 (2021)
T. Liang, J. Xue, Z. Yao, Y. Ye, X. Yang, X. Hou, H. Fang, Design, synthesis and biological evaluation of 3, 4-disubstituted-imidazolidine-2, 5-dione derivatives as HDAC6 selective inhibitors. Eur. J. Med. Chem. 221, 113526 (2021)
Y. Li, J. Quan, H. Song, D. Li, E. Ma, Y. Wang, C. Ma, Novel pyrrolo[2,1-c][1,4]benzodiazepine-3,11-dione (PBD) derivatives as selective HDAC6 inhibitors to suppress tumor metastasis and invasion in vitro and in vivo. Bioorganic Chem. 114, 105081 (2021)
S. Li, C. Zhao, G. Zhang, Q. Xu, Q. Liu, W. Zhao, C. James Chou, Y. Zhang, Development of selective HDAC6 inhibitors with in vitro and in vivo anti-multiple myeloma activity. Bioorganic Chem. 116, 105278 (2021)
C. Sharma, Y.J. Oh, B. Park, S. Lee, C.-H. Jeong, S. Lee, J.H. Seo, Y.H. Seo, Development of Thiazolidinedione-Based HDAC6 Inhibitors to Overcome Methamphetamine Addiction. Int. J. Mol. Sci. 20, 6213 (2019)
Y. Song, J. Lim, Y.H. Seo, A novel class of anthraquinone-based HDAC6 inhibitors. Eur. J. Med. Chem. 164, 263–272 (2019)
L. Goracci, N. Deschamps, G.M. Randazzo, C. Petit, C. Dos Santos Passos, P.-A. Carrupt, C. Simões-Pires, A. Nurisso, A Rational Approach for the Identification of Non-Hydroxamate HDAC6-Selective Inhibitors. Sci. Rep. 6, 29086 (2016)
X.-H. Zhang, H.-Q. Kang, Y.-Y. Tao, Y.-H. Li, J.-R. Zhao, Ya-Gao, L.-Y. Ma, H.-M. Liu, Identification of novel 1,3-diaryl-1,2,4-triazole-capped histone deacetylase 6 inhibitors with potential anti-gastric cancer activity. Eur. J. Med. Chem. 218, 113392 (2021)
C. Seidel, M. Schnekenburger, A. Mazumder, M.-H. Teiten, G. Kirsch, M. Dicato, M. Diederich, 4-Hydroxybenzoic acid derivatives as HDAC6-specific inhibitors modulating microtubular structure and HSP90α chaperone activity against prostate cancer. Biochem. Pharmacol. 99, 31–52 (2016)
M. Leonhardt, A. Sellmer, O.H. Krämer, S. Dove, S. Elz, B. Kraus, M. Beyer, S. Mahboobi, Design and biological evaluation of tetrahydro-β-carboline derivatives as highly potent histone deacetylase 6 (HDAC6) inhibitors. Eur. J. Med. Chem. 152, 329–357 (2018)
H.-Y. Lee, A.-C. Tsai, M.-C. Chen, P.-J. Shen, Y.-C. Cheng, C.-C. Kuo, S.-L. Pan, Y.-M. Liu, J.-F. Liu, T.-K. Yeh, J.-C. Wang, C.-Y. Chang, J.-Y. Chang, J.-P. Liou, Azaindolylsulfonamides, with a more selective inhibitory effect on histone deacetylase 6 activity, exhibit antitumor activity in colorectal cancer HCT116 cells. J. Med. Chem. 57, 4009–4022 (2014)
Y.-M. Liu, H.-Y. Lee, M.-J. Lai, S.-L. Pan, H.-L. Huang, F.-C. Kuo, M.-C. Chen, J.-P. Liou, Pyrimidinedione-mediated selective histone deacetylase 6 inhibitors with antitumor activity in colorectal cancer HCT116 cells. Org. Biomol. Chem. 13, 10226–10235 (2015)
M. Kaliszczak, S. Trousil, O. Åberg, M. Perumal, Q.-D. Nguyen, E.O. Aboagye, A novel small molecule hydroxamate preferentially inhibits HDAC6 activity and tumour growth. Br. J. Cancer 108, 342–350 (2013)
K. Nepali, H.-Y. Lee, M.-J. Lai, R. Ojha, T.-Y. Wu, G.-X. Wu, M.-C. Chen, J.-P. Liou, Ring-opened tetrahydro-γ-carbolines display cytotoxicity and selectivity with histone deacetylase isoforms. Eur. J. Med. Chem. 127, 115–127 (2017)
M.-C. Chen, Y.-C. Lin, Y.-H. Liao, J.-P. Liou, C.-H. Chen, MPT0G612, a novel HDAC6 inhibitor, induces apoptosis and suppresses IFN-γ-induced programmed death-ligand 1 in human colorectal carcinoma cells. Cancers 11, 1617 (2019)
H.-Y. Lee, K. Nepali, F.-I. Huang, C.-Y. Chang, M.-J. Lai, Y.-H. Li, H.-L. Huang, C.-R. Yang, J.-P. Liou, (N-Hydroxycarbonylbenylamino)quinolines as selective histone deacetylase 6 inhibitors suppress growth of multiple myeloma in vitro and in vivo. J. Med. Chem. 61, 905–917 (2018)
H.-W. Ryu, D.-H. Lee, D.-H. Shin, S.H. Kim, S.H. Kwon, Aceroside VIII is a new natural selective HDAC6 inhibitor that synergistically enhances the anticancer activity of HDAC inhibitor in HT29 cells. Planta Med. 81, 222–227 (2015)
C.-W. Yu, P.-Y. Hung, H.-T. Yang, Y.-H. Ho, H.-Y. Lai, Y.-S. Cheng, J.-W. Chern, Quinazolin-2,4-dione-based hydroxamic acids as selective histone deacetylase-6 inhibitors for treatment of non-small cell lung cancer. J. Med. Chem. 62, 857–874 (2019)
S. Noonepalle, S. Shen, J. Ptáček, M.T. Tavares, G. Zhang, J. Stránský, J. Pavlíček, G.M. Ferreira, M. Hadley, G. Pelaez, C. Bařinka, A.P. Kozikowski, A. Villagra, Rational design of suprastat: A novel selective histone deacetylase 6 inhibitor with the ability to potentiate immunotherapy in melanoma models. J. Med. Chem. 63, 10246–10262 (2020)
X. Chen, X. Chen, R.R. Steimbach, T. Wu, H. Li, W. Dan, P. Shi, C. Cao, D. Li, A.K. Miller, Z. Qiu, J. Gao, Y. Zhu, Novel 2, 5-diketopiperazine derivatives as potent selective histone deacetylase 6 inhibitors: Rational design, synthesis and antiproliferative activity. Eur. J. Med. Chem. 187, 111950 (2020)
M. Pérez-Salvia, E. Aldaba, Y. Vara, M. Fabre, C. Ferrer, C. Masdeu, A. Zubia, E.S. Sebastian, D. Otaegui, P. Llinàs-Arias, M. Rosselló-Tortella, M. Berdasco, C. Moutinho, F. Setien, A. Villanueva, E. González-Barca, J. Muncunill, J.-T. Navarro, M.A. Piris, F.P. Cossio, M. Esteller, In vitro and in vivo activity of a new small-molecule inhibitor of HDAC6 in mantle cell lymphoma. Haematologica 103, e537–e540 (2018)
J. Sun, W. Wu, X. Tang, F. Zhang, C. Ju, R. Liu, Y. Liang, B. Yu, B. Lv, Y. Guo, D. Zeng, X. Tao, M. Wang, Z. Zhang, C. Zhang, and X.-B. Lv, HDAC6 inhibitor WT161 performs anti-tumor effect on osteosarcoma and synergistically interacts with 5-FU. Biosci. Rep. 41, BSR20203905 (2021)
F. Wang, L. Zheng, Y. Yi, Z. Yang, Q. Qiu, X. Wang, W. Yan, P. Bai, J. Yang, D. Li, H. Pei, T. Niu, H. Ye, C. Nie, Y. Hu, S. Yang, Y. Wei, L. Chen, SKLB-23bb, A HDAC6-Selective Inhibitor, Exhibits Superior and Broad-Spectrum Antitumor Activity via Additionally Targeting Microtubules. Mol. Cancer Ther. 17, 763–775 (2018)
M.K. Ediriweera, N.B. To, Y. Lim, S.K. Cho, Odd-chain fatty acids as novel histone deacetylase 6 (HDAC6) inhibitors. Biochimie 186, 147–156 (2021)
Y.W. Song, Y. Lim, S.K. Cho, 2,4-Di-tert-butylphenol, a potential HDAC6 inhibitor, induces senescence and mitotic catastrophe in human gastric adenocarcinoma AGS cells. Biochem. Biophys. Acta BBA - Mol. Cell Res. 1865, 675–683 (2018)
J. Dong, N. Zheng, X. Wang, C. Tang, P. Yan, H. Zhou, J. Huang, A novel HDAC6 inhibitor exerts an anti-cancer effect by triggering cell cycle arrest and apoptosis in gastric cancer. Eur. J. Pharmacol. 828, 67–79 (2018)
G. Yan, D. Li, X. Zhong, G. Liu, X. Wang, Y. Lu, F. Qin, Y. Guo, S. Duan, D. Li, Identification of HDAC6 selective inhibitors: pharmacophore based virtual screening, molecular docking and molecular dynamics simulation. J. Biomol. Struct. Dyn. 39, 1928–1939 (2021)
C. Zhao, J. Gao, L. Zhang, L. Su, Y. Luan, Novel HDAC6 selective inhibitors with 4-aminopiperidine-1- carboxamide as the core structure enhanced growth inhibitory activity of bortezomib in MCF-7 cells. Biosci. Trends 13, 91–97 (2019)
M. Dawood, M. Elbadawi, M. Böckers, G. Bringmann, T. Efferth, Molecular docking-based virtual drug screening revealing an oxofluorenyl benzamide and a bromonaphthalene sulfonamido hydroxybenzoic acid as HDAC6 inhibitors with cytotoxicity against leukemia cells. Biomed. Pharmacother. 129, 110454 (2020)
L. Wasim, M. Chopra, Panobinostat induces apoptosis via production of reactive oxygen species and synergizes with topoisomerase inhibitors in cervical cancer cells. Biomed. Pharmacother. 84, 1393–1405 (2016)
L. Wasim, M. Chopra, Synergistic anticancer effect of panobinostat and topoisomerase inhibitors through ROS generation and intrinsic apoptotic pathway induction in cervical cancer cells. Cell. Oncol. Dordr. 41, 201–212 (2018)
L. Hontecillas-Prieto, R. Flores-Campos, A. Silver, E. de Álava, N. Hajji, D.J. García-Domínguez, Synergistic enhancement of cancer therapy using HDAC inhibitors: opportunity for clinical trials. Front. Genet. 11, 578011 (2020)
J. E. Amengual, J. K. Lue, H. Ma, R. Lichtenstein, B. Shah, S. Cremers, S. Jones, and A. Sawas, First-in-class selective HDAC6 inhibitor (ACY-1215) Has a highly favorable safety profile in patients with relapsed and refractory lymphoma. Oncologist 26, 184 (3)
R. Mazroui, S. Di Marco, R.J. Kaufman, I.E. Gallouzi, Inhibition of the ubiquitin-proteasome system induces stress granule formation. Mol. Biol. Cell 18, 2603–2618 (2007)
S. Kwon, Y. Zhang, P. Matthias, The deacetylase HDAC6 is a novel critical component of stress granules involved in the stress response. Genes Dev. 21, 3381–3394 (2007)
M. Kästle, E. Woschee, T. Grune, Histone deacetylase 6 (HDAC6) plays a crucial role in p38MAPK-dependent induction of heme oxygenase-1 (HO-1) in response to proteasome inhibition. Free Radic. Biol. Med. 53, 2092–2101 (2012)
T. Hideshima, J.E. Bradner, J. Wong, D. Chauhan, P. Richardson, S.L. Schreiber, K.C. Anderson, Small-molecule inhibition of proteasome and aggresome function induces synergistic antitumor activity in multiple myeloma. Proc. Natl. Acad. Sci. U.S.A. 102, 8567–8572 (2005)
S.W. Lee, S.-K. Yeon, G.W. Kim, D.H. Lee, Y.H. Jeon, J. Yoo, S.Y. Kim, S.H. Kwon, HDAC6-selective inhibitor overcomes bortezomib resistance in multiple myeloma. Int. J. Mol. Sci. 22, 1341 (2021)
X. Sun, Y. Xie, X. Sun, Y. Yao, H. Li, Z. Li, R. Yao, and K. Xu, The selective HDAC6 inhibitor Nexturastat A induces apoptosis, overcomes drug resistance and inhibits tumor growth in multiple myeloma. Biosci. Rep. 39, BSR20181916 (2019)
F.I. Huang, Y.W. Wu, T.Y. Sung, J.P. Liou, M.H. Lin, S.L. Pan, C.R. Yang, MPT0G413, A novel HDAC6-selective inhibitor, and bortezomib synergistically exert anti-tumor activity in multiple myeloma cells. Front. Oncol. 9, 249 (2019)
J.E. Amengual, P. Johannet, M. Lombardo, K. Zullo, D. Hoehn, G. Bhagat, L. Scotto, X. Jirau-Serrano, D. Radeski, J. Heinen, H. Jiang, S. Cremers, Y. Zhang, S. Jones, O.A. O’Connor, Dual targeting of protein degradation pathways with the selective HDAC6 inhibitor ACY-1215 and bortezomib is synergistic in lymphoma. Clin. Cancer Res. 21, 4663–4675 (2015)
L. Santo, T. Hideshima, A.L. Kung, J.C. Tseng, D. Tamang, M. Yang, M. Jarpe, J.H. van Duzer, R. Mazitschek, W.C. Ogier, D. Cirstea, S. Rodig, H. Eda, T. Scullen, M. Canavese, J. Bradner, K.C. Anderson, S.S. Jones, N. Raje, Preclinical activity, pharmacodynamic, and pharmacokinetic properties of a selective HDAC6 inhibitor, ACY-1215, in combination with bortezomib in multiple myeloma. Blood 119, 2579–2589 (2012)
S.T. Nawrocki, J.S. Carew, M.S. Pino, R.A. Highshaw, R.H. Andtbacka, K. Dunner, A. Pal, W.G. Bornmann, P.J. Chiao, P. Huang, H. Xiong, J.L. Abbruzzese, D.J. McConkey, Aggresome disruption: a novel strategy to enhance bortezomib-induced apoptosis in pancreatic cancer cells. Cancer Res. 66, 3773–3781 (2006)
Y. Mishima, L. Santo, H. Eda, D. Cirstea, N. Nemani, A.J. Yee, E. O’Donnell, M.K. Selig, S.N. Quayle, S. Arastu-Kapur, C. Kirk, L.H. Boise, S.S. Jones, N. Raje, Ricolinostat (ACY-1215) induced inhibition of aggresome formation accelerates carfilzomib-induced multiple myeloma cell death. Br. J. Haematol. 169, 423–434 (2015)
R.A. Stanton, K.M. Gernert, J.H. Nettles, R. Aneja, Drugs that target dynamic microtubules: a new molecular perspective. Med. Res. Rev. 31, 443–481 (2011)
E. Mukhtar, V.M. Adhami, H. Mukhtar, Targeting microtubules by natural agents for cancer therapy. Mol. Cancer Ther. 13, 275–284 (2014)
J. Asthana, S. Kapoor, R. Mohan, and D. Panda, Inhibition of HDAC6 deacetylase activity increases its binding with microtubules and suppresses microtubule dynamic instability in MCF-7 cells. J. Biol. Chem. 288, 22516–22526–5438 (2013)
Y. Itoh, T. Suzuki, A. Kouketsu, N. Suzuki, S. Maeda, M. Yoshida, H. Nakagawa, N. Miyata, Design, synthesis, structure-selectivity relationship, and effect on human cancer cells of a novel series of histone deacetylase 6-selective inhibitors. J. Med. Chem. 50, 5425–5438 (2007)
J. Yoo, Y.H. Jeon, D.H. Lee, G.W. Kim, S.W. Lee, S.Y. Kim, J. Park, S.H. Kwon, HDAC6-selective inhibitors enhance anticancer effects of paclitaxel in ovarian cancer cells. Oncol. Lett. 21, 201 (2021)
T. Oba, M. Ono, H. Matoba, T. Uehara, Y. Hasegawa, K. Ito, HDAC6 inhibition enhances the anti-tumor effect of eribulin through tubulin acetylation in triple-negative breast cancer cells. Breast Cancer Res. Treat. 186, 37–51 (2021)
H.-J. Tu, Y.-J. Lin, M.-W. Chao, T.-Y. Sung, Y.-W. Wu, Y.-Y. Chen, M.-H. Lin, J.-P. Liou, S.-L. Pan, C.-R. Yang, The anticancer effects of MPT0G211, a novel HDAC6 inhibitor, combined with chemotherapeutic agents in human acute leukemia cells. Clin. Epigenetics 10, 162 (2018)
C. Corno, N. Arrighetti, E. Ciusani, E. Corna, N. Carenini, N. Zaffaroni, L. Gatti, P. Perego, Synergistic interaction of histone deacetylase 6- and MEK-inhibitors in castration-resistant prostate cancer cells. Front. Cell Dev. Biol. 8, 610 (2020)
M. Namdar, G. Perez, L. Ngo, P.A. Marks, Selective inhibition of histone deacetylase 6 (HDAC6) induces DNA damage and sensitizes transformed cells to anticancer agents. Proc. Natl. Acad. Sci. U.S.A. 107, 20003–20008 (2010)
L. Wang, S. Xiang, K.A. Williams, H. Dong, W. Bai, S.V. Nicosia, S. Khochbin, G. Bepler, X. Zhang, Depletion of HDAC6 enhances cisplatin-induced DNA damage and apoptosis in non-small cell lung cancer cells. PLoS ONE 7, e44265 (2012)
A. Bag, A. Schultz, S. Bhimani, O. Stringfield, W. Dominguez, Q. Mo, L. Cen, D. Adeegbe, Coupling the immunomodulatory properties of the HDAC6 inhibitor ACY241 with Oxaliplatin promotes robust anti-tumor response in non-small cell lung cancer. Oncoimmunology 11, 2042065 (2022)
Y. Ruan, L. Wang, Y. Lu, HDAC6 inhibitor, ACY1215 suppress the proliferation and induce apoptosis of gallbladder cancer cells and increased the chemotherapy effect of gemcitabine and oxaliplatin. Drug Dev. Res. 82, 598–604 (2021)
J. Sun, X. Qian, F. Zhang, X. Tang, C. Ju, R. Liu, R. Zhou, Z. Zhang, X.-B. Lv, C. Zhang, G. Huang, HDAC6 inhibitor WT161 induces apoptosis in retinoblastoma cells and synergistically interacts with cisplatin. Transl. Cancer Res. 8, 2759–2768 (2019)
X.-N. Wang, K.-Y. Wang, X.-S. Zhang, C. Yang, X.-Y. Li, 4-Hydroxybenzoic acid (4-HBA) enhances the sensitivity of human breast cancer cells to adriamycin as a specific HDAC6 inhibitor by promoting HIPK2/p53 pathway. Biochem. Biophys. Res. Commun. 504, 812–819 (2018)
H.-R. Won, H.-W. Ryu, D.-H. Shin, S.-K. Yeon, D.H. Lee, S.H. Kwon, A452, an HDAC6-selective inhibitor, synergistically enhances the anticancer activity of chemotherapeutic agents in colorectal cancer cells. Mol. Carcinog. 57, 1383–1395 (2018)
M. Bobrowicz, A. Slusarczyk, J. Domagala, M. Dwojak, D. Ignatova, Y.T. Chang, C. Iselin, N. Miazek-Zapala, K. Marhelava, E. Guenova, M. Winiarska, Selective inhibition of HDAC6 sensitizes cutaneous T-cell lymphoma to PI3K inhibitors. Oncol. Lett. 20, 533–540 (2020)
H. Losson, S.R. Gajulapalli, M. Lernoux, J.-Y. Lee, A. Mazumder, D. Gérard, C. Seidel, H. Hahn, C. Christov, M. Dicato, G. Kirsch, B.W. Han, M. Schnekenburger, M. Diederich, The HDAC6 inhibitor 7b induces BCR-ABL ubiquitination and downregulation and synergizes with imatinib to trigger apoptosis in chronic myeloid leukemia. Pharmacol. Res. 160, 105058 (2020)
Y. Qin, Y. Liang, G. Jiang, Y. Peng, W. Feng, ACY-1215 suppresses the proliferation and induces apoptosis of chronic myeloid leukemia cells via the ROS/PTEN/Akt pathway. Cell Stress Chaperones 27, 383–396 (2022)
D.H. Lee, G.W. Kim, S.H. Kwon, The HDAC6-selective inhibitor is effective against non-Hodgkin lymphoma and synergizes with ibrutinib in follicular lymphoma. Mol. Carcinog. 58, 944–956 (2019)
S.-J. Park, S.H. Joo, N. Lee, W.-J. Jang, J.H. Seo, C.-H. Jeong, ACY-241, an HDAC6 inhibitor, overcomes erlotinib resistance in human pancreatic cancer cells by inducing autophagy. Arch. Pharm. Res. 44, 1062–1075 (2021)
U. Peng, Z. Wang, S. Pei, Y. Ou, P. Hu, W. Liu, J. Song, ACY-1215 accelerates vemurafenib induced cell death of BRAF-mutant melanoma cells via induction of ER stress and inhibition of ERK activation. Oncol. Rep. 37, 1270–1276 (2017)
G. Zhang, Y.H. Gan, Synergistic antitumor effects of the combined treatment with an HDAC6 inhibitor and a COX-2 inhibitor through activation of PTEN. Oncol. Rep. 38, 2657–2666 (2017)
M. Cosenza, M. Civallero, L. Marcheselli, S. Sacchi, S. Pozzi, Ricolinostat, a selective HDAC6 inhibitor, shows anti-lymphoma cell activity alone and in combination with bendamustine. Apoptosis 25, 370–387 (2020)
J.S. Carew, C.M. Espitia, W. Zhao, V. Visconte, F. Anwer, K.R. Kelly, S.T. Nawrocki, Rational cotargeting of HDAC6 and BET proteins yields synergistic antimyeloma activity. Blood Adv. 3, 1318–1329 (2019)
B.J. North, I. Almeciga-Pinto, D. Tamang, M. Yang, S.S. Jones, S.N. Quayle, Enhancement of pomalidomide anti-tumor response with ACY-241, a selective HDAC6 inhibitor. PLoS ONE 12, e0173507 (2017)
K. Miyake, N. Takano, H. Kazama, H. Kikuchi, M. Hiramoto, K. Tsukahara, K. Miyazawa, Ricolinostat enhances adavosertib-induced mitotic catastrophe in TP53-mutated head and neck squamous cell carcinoma cells. Int. J. Oncol. 60, 54 (2022)
D.O. Adeegbe, Y. Liu, P.H. Lizotte, Y. Kamihara, A.R. Aref, C. Almonte, R. Dries, Y. Li, S. Liu, X. Wang, T. Warner-Hatten, J. Castrillon, G.C. Yuan, N. Poudel-Neupane, H. Zhang, J.L. Guerriero, S. Han, M.M. Awad, D.A. Barbie, J. Ritz, S.S. Jones, P.S. Hammerman, J. Bradner, S.N. Quayle, K.K. Wong, Synergistic immunostimulatory effects and therapeutic benefit of combined histone deacetylase and bromodomain inhibition in non-small cell lung cancer. Cancer Discov. 7, 852–867 (2017)
H.Y. Cho, S.W. Lee, Y.H. Jeon, D.H. Lee, G.W. Kim, J. Yoo, S.Y. Kim, S.H. Kwon, Combination of ACY-241 and JQ1 synergistically suppresses metastasis of HNSCC via regulation of MMP-2 and MMP-9. Int. J. Mol. Sci. 21, 6873 (2020)
Y. Liu, Y. Li, S. Liu, D.O. Adeegbe, C.L. Christensen, M.M. Quinn, R. Dries, S. Han, K. Buczkowski, X. Wang, T. Chen, P. Gao, H. Zhang, F. Li, P.S. Hammerman, J.E. Bradner, S.N. Quayle, K.-K. Wong, NK cells mediate synergistic antitumor effects of combined inhibition of HDAC6 and BET in a SCLC preclinical model. Cancer Res. 78, 3709–3717 (2018)
S. Moufarrij, A. Srivastava, S. Gomez, M. Hadley, E. Palmer, P.T. Austin, S. Chisholm, N. Diab, K. Roche, A. Yu, J. Li, W. Zhu, M. Lopez-Acevedo, A. Villagra, K.B. Chiappinelli, Combining DNMT and HDAC6 inhibitors increases anti-tumor immune signaling and decreases tumor burden in ovarian cancer. Sci. Rep. 10, 3470 (2020)
T. Fukumoto, N. Fatkhutdinov, J.A. Zundell, E.N. Tcyganov, T. Nacarelli, S. Karakashev, S. Wu, Q. Liu, D.I. Gabrilovich, R. Zhang, HDAC6 inhibition synergizes with anti-PD-L1 therapy in ARID1A-inactivated ovarian cancer. Cancer Res. 79, 5482–5489 (2019)
G.W. Kim, J. Yoo, H.-R. Won, S.-K. Yeon, S.W. Lee, D.H. Lee, Y.H. Jeon, S.H. Kwon, HDAC6-selective inhibitor synergistically enhances the anticancer activity of immunomodulatory drugs in IMiDs-resistant multiple myeloma. Leuk. Res. 95, 106398 (2020)
Funding
Sumeet Kaur would like to thank the University Grants Commission (UGC), New Delhi, India, for awarding her a UGC fellowship. Prerna Rajoria would like to thank the Department of Biotechnology (DBT), Ministry of Science & Technology, Government of India for awarding her a DBT-JRF fellowship (Grant Number: DBT/2021–22/CBR/1593).
Author information
Authors and Affiliations
Contributions
Madhu Chopra conceptualized the article and critically revised the work. Sumeet Kaur conceptualized the article, performed the literature search, and drafted and critically revised the work. Prerna Rajoria performed the literature search and prepared the figures.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
No ethical approval and consent to participate was required for this study.
Consent for publication
There is no conflict of interest (either financial or personal). All authors and acknowledged contributors have read and approved the manuscript.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kaur, S., Rajoria, P. & Chopra, M. HDAC6: A unique HDAC family member as a cancer target. Cell Oncol. 45, 779–829 (2022). https://doi.org/10.1007/s13402-022-00704-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13402-022-00704-6