Abstract
The double-lumen cannula (DLC) is the most critical component of extracorporeal membrane oxygenation (ECMO) because of its narrow cross-section, thereby developing the highest shear stress in the entire ECMO circuit. To measure blood damage in a DLC, the Eulerian approach is generally used without contemplating exposure time or history of blood exposure to shear stresses. Alternatively, Lagrangian approach has also been recently employed for a Newtonian blood flow through a DLC, thereby leaving a research gap on the impact of variable shear rate in case of non-Newtonian blood flow. In the present study, the hemodynamic performance of DLC is investigated using different non-Newtonian models by applying Lagrangian approach. Moreover, the motion of RBC was tracked inside the cannula to predict its behavior during the motion. The results showed that the return lumen had higher pressure, velocity, and shear stress values than other parts of the DLC. In addition, recirculation was observed due to the mixing of blood coming from different inlets and found increase with increasing flow rate of blood. Moreover, it was found that the blood damage increased with increasing flow rate. There was more blood damage in the Newtonian model than in the other non-Newtonian models at higher flow rates. However, the Carreau model showed more blood damage at lower flow rates than the other models. The Cross model showed DLC’s higher efficacy in delivering oxygenated blood to the tricuspid outlet because it showed the least blood damage among all other models. It was also concluded that the efficacy of the DLC to deliver oxygenated blood to the tricuspid outlet decreases with increasing blood flow rate.
























Similar content being viewed by others
Data availability
Data will be made available upon request.
References
Rabah H, Rabah A (2022) Extracorporeal membrane oxygenation (ECMO): what we need to know. Cureus 14(7):e2673
Makdisi G, Wang IW (2015) Extra corporeal membrane oxygenation (ECMO) review of a lifesaving technology. J Thorac Dis 7(7):E166
de Chaves RCF, Filho RR, Timenetsky KT, Moreira FT, da Vilanova LCS, de Bravim BA, Neto AS, Corrêa TD (2019) Extracorporeal membrane oxygenation: a literature review. Rev Bras Ter Intensiva 31(3):410–424
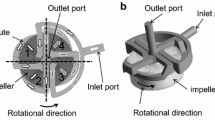
Jamil M, Rezaeimoghaddam M, Cakmak B, Rasooli R, Salihoglu E, Yıldız Y, Pekkan K (2018) Patient-specific atrial hemodynamics of a double lumen neonatal cannula in correct caval position. Artif Organs 42(4):401–409
Rais-Bahrami K, Walton DM, Sell JE, Rivera O, Mikesell GT, Short BL (2002) Improved oxygenation with reduced recirculation during venovenous ECMO: comparison of two catheters. Perfusion 17(6):415–419
Albert AA et al (2002) Is there any impact of the shape of aortic end-hole cannula on stroke occurrence? Clinical evaluation of straight and bent-tip aortic cannulae. Perfusion 17(6):451–456
Myagmar O (2011) Evaluation of CFD based hemolysis prediction methods. Rochester Institute of Technology. https://scholarworks.rit.edu/theses/5822
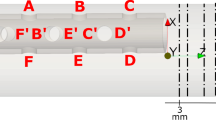
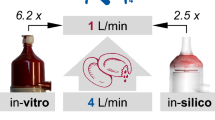
Ahmad F, Cheema TA, Rehman K, Ullah M, Jamil M, Park CW (2023) Hemodynamic performance evaluation of neonatal ECMO double lumen cannula using fluid–structure interaction. Int J Numer Methods Biomed Eng 39(6):e3706
Rasooli R, Jamil M, Rezaeimoghaddam M, Yıldız Y, Salihoglu E, Pekkan K (2021) Hemodynamic performance limits of the neonatal double-lumen cannula. J Biomech 121:110382
Mallik BB, Nanda S, Das B, Saha D, Das DS, Paul K (2013) A non-newtonian fluid model for blood flow using power-law through an atherosclerotic arterial segment having slip velocity. Int J Pharm Chem Biol Sci 3(3):752–760
Hussain MA, Kar S, Puniyani RR (1999) Relationship between power law coefficients and major blood constituents affecting the whole blood viscosity. J Biosci 24(3):329–337
Johnston BM, Johnston PR, Corney S, Kilpatrick D (2004) Non-Newtonian blood flow in human right coronary arteries: steady state simulations. J Biomech 37(5):709–720
Canonsburg TD (2013) ANSYS fluent theory guide, vol 15317. ANSYS Inc., Canonsburg, p 814
Nader E, Skinner S, Romana M, Romain F, Lemonne N, Guillot N, Gauthier A, Jonville SA, Renoux C, Dessources MDH, Stauffer E, Joly P, Bertrand Y, Connes P (2019) Blood rheology: key parameters, impact on blood flow, role in sickle cell disease and effects of exercise. Front Physiol 10:1–14
Cutnell JD, Johnson KW (1998) Physics, 4th edn. Wiley, New York, p 308
Bersten AD, Williams DRG, Phillips GD (1988) Central venous catheter stiffness and its relation to vascular perforation. Anaesth Intensive Care 16(3):342–351
Evans N, Kluckow M (2000) Superior vena cava flow in newborn infants: a novel marker of systemic blood flow. Arch Dis Child Fetal Neonatal Ed 82(3):F182–F187
Shibeshi SS, Collins WE (2005) The rheology of blood flow in a branched arterial system. Appl Rheol 15(6):398–405
Cho YI, Kensey KR (1991) Effects of the non-newtonian viscosity of blood on flows in a diseased arterial vessel. part 1: steady flows. Biorheology 28:241–262
Soulis JV, Giannoglou GD, Chatzizisis YS, Seralidou KV, Parcharidis GE, Louridas GE (2008) Non-Newtonian models for molecular viscosity and wall shear stress in a 3D reconstructed human left coronary artery. Med Eng Phys 30(1):9–19
Evans E, Fung YC (1972) Improved measurements of the erythrocyte geometry. Microvasc Res 4(4):335–347
Ni A, Cheema TA, Park CW (2015) Numerical investigation onthe structural characteristics of multiple RBCs in a stenotic microcapillary under plasma-alcohol solution. Korea Aust Rheol J 27(2):163–171
Rotsch C, Jacobson K, Radmacher M (1999) Dimensional and mechanical dynamics of active and stable edges in motile fibroblasts investigated by using atomic force microscopy. Proc Natl Acad Sci USA 96(3):921–926
Acknowledgements
This work was supported by Pakistan Science Foundation (PSF) under the project No. PSF-TUBITAK/ENG/KP-GIKI (12).
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ullah, M., Cheema, T.A., Aleksey, N. et al. Rheological investigation of neonatal double-lumen cannula with and without deformable erythrocytes. Korea-Aust. Rheol. J. 35, 373–389 (2023). https://doi.org/10.1007/s13367-023-00073-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13367-023-00073-y