Abstract
Background
Primary immunodeficiency disorders are genetically heterogeneous immune disorders with a wide range of infectious and non-infectious manifestations.
Objective
To describe a single-center experience of primary immunodeficiency disorders.
Design
Retrospective analysis from January 2015 to January 2020.
Setting
Tertiary care children’s hospital.
Participants
One hundred and twelve children (<18 years) diagnosed with primary immunodeficiency disorders.
Outcome measure
Diagnostic spectrum, clinical features, and outcome.
Results
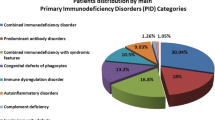
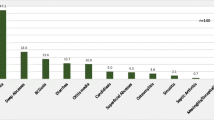
The median (IQR) age of the first clinical manifestation and lag time in diagnosis was 10 (27) and 11 (18) months, respectively. Twenty-seven children (24%) were diagnosed during their first presentation. Thirty-six (32%) children had phagocytic disorders, 20 (17.8%) had combined/cellular defects, 18 (16%) had predominant antibody deficiencies and 17 (15%) had disorders of immune dysregulation. Non-infectious manifestations were seen in 54 (48%). Eight children underwent hematopoietic stem cell transplantation, 44 (39%) children were on antimicrobial prophylaxis and supportive therapy, 36 (32%) were lost to follow-up and 24 (21%) children died.
Conclusion
Congenital defects of phagocyte function, followed by combined/cellular defects are the commonest primary immune deficiencies (PIDs) identified in southern India. Long lag time in diagnosis and high mortality in our cohort emphasizes the need for early diagnosis and early referral.
Similar content being viewed by others
References
McCusker C, Upton J, Warrington R. Primary immunodeficiency. Allergy Asthma Clin Immunol. 2018;14:61.
Abolhassani H, Tavakol M, Chavoshzadeh Z, et al. National Consensus on Diagnosis and Management Guidelines for Primary Immunodeficiency. Immunol Gen J. 2019;2:1–21.
Bousfiha AA, Jeddane L, Ailal F, et al. Primary immunodeficiency diseases worldwide: More common than generally thought. J Clin Immunol. 2013;33:1–7.
Jindal AK, Pilania RK, Rawat A, Singh S. Primary immunodeficiency disorders in India-a situational review. Frontiers in Immunol. 2017;8:714.
Costa-Carvalho BT, Grumach AS, Franco JL, et al. Attending to warning signs of primary immunodeficiency diseases across the range of clinical practice. J Clin Immunol. 2014;34:10–22.
Bousfiha A, Jeddane L, Picard C, et al. The 2017 IUIS Phenotypic Classification for Primary Immunodeficiencies. J Clin Immunol. 2018;38:129–43.
Madkaikar M, Mishra A, Desai M, Gupta M, Mhatre S, Ghosh K. Comprehensive report of primary immunodeficiency disorders from a tertiary care center in India. J Clin Immunol. 2013;33:507–12.
Gupta D, Thakral D, Kumar P, et al. Primary immunodeficiency disorders among north Indian children. Indian J Pediatrics. 2019;86:885–91.
de Silva NR, Gunawardena S, Rathnayake D, Wickramasingha GD. The spectrum of primary immunodeficiency disorders in Sri Lanka. Allergy Asthma Clin Immunol. 2013;9:50.
Ballow M. Primary immunodeficiency disorders: Antibody deficiency. J Allergy Clin Immunol. 2002;109:581–91.
Sorensen RU, Moore C. Antibody deficiency syndromes. Pediatric Clin North Am. 2000;471225-52.
O’Sullivan MD, Cant AJ. The 10 warning signs: time for a change? Curr Opin in Allergy Clin Immunol. 2012;12:588–94.
Reyes SO, Ramirez-Vazquez G, Hernández AC, et al. Clinical features, non-infectious manifestations and survival analysis of 161 children with primary immunodeficiency in Mexico: A single center experience over two decades. J Clin Immunol. 2016;36:56–65.
Arkwright PD, Gennery AR. Ten warning signs of a primary immunodeficiency: A new paradigm is needed for the 21st century. Ann New York Acad Sci. 2011;1238:7–14.
Bousfiha A, Jeddane L, Picard C, et al. Human inborn errors of immunity: 2019 update of the IUIS phenotypical classification. J Clin Immunol. 2020:40;66–81.
Nijman IJ, van Montfrans JM, Hoogstraat M, et al. Targeted next-generation sequencing: A novel diagnostic tool for primary immunodeficiencies. J Allergy Clin Immunol. 2014;133:529–34.
Raje N, Soden S, Swanson D, Ciaccio CE, Kingsmore SF, Dinwiddie DL. The utility of next-generation sequencing in clinical primary immunodeficiencies. Curr Allergy Asthma Rep. 2014;14:468.
Heimall J, Cowan MJ. Long term outcomes of severe combined immunodeficiency: therapy implications. Expert Rev Clin Immunol. 2017;13:1029–40.
Kelly BT, Tam JS, Verbsky JW, Routes JM. Screening for severe combined immunodeficiency in neonates. Clin Epidemiol. 2013;5:363.
Uppuluri R, Jayaraman D, Sivasankaran M, et al. Hematopoietic stem cell transplantation for primary immunodeficiency disorders: Experience from a referral center in India. Indian Pediatr. 2018;55:661–4.
Kapoor N, Raj R. Hematopoietic stem cell transplantation for primary immune deficiency disorders. The Indian Journal of Pediatrics. 2016;83:450–4.
Madkaikar M, Aluri J, Gupta S. Guidelines for Screening, Early Diagnosis, and Management of Severe Combined Immunodeficiency (SCID) in India. Indian J Pediatrics. 2016;83:455–62.
Pilania RK, Chaudhary H, Jindal AK, Rawat A, Singh S. Current status and prospects of primary immunodeficiency diseases in Asia. Genes Diseases. 2020;7:3–11.
Acknowledgements
Dr Bala Ramachandran, Dr Janani Sankar, Dr Lalitha Janakiraman, Dr T. Ravikumar, Dr T Vasanthi, Dr KG Ravikumar, Dr S Sivabalan, Dr S Srinivas and Dr Chandra Kumar, for their support in diagnosis and management. Dr Manisha madkaikar and her team at National Institute of Immuno-Hematology for helping in flow cytometry.
Author information
Authors and Affiliations
Corresponding author
Additional information
Ethical Clearance
Ethucs Committee of KK CHILDS Trust Hsopital and the CHILDS Trust Medical Research Foundation; No. IEC-52/May 2020, dated 8 December, 2020.
Contributors
MS: analyzed the data, outcome assessment and prepared the manuscript; DM: managed the cases and analyzed data; SBS: contributed to patient management, critical analysis of the manuscript and editing; SA, SD, RB: collected and analyzed the data; DK, VK: contributed to the patient management and writing of the manuscript.
Funding
None
Competing interest
None stated.
Rights and permissions
About this article
Cite this article
Sivasankaran, M., Munirathnam, D., Balasubramanian, S. et al. Diagnostic Spectrum and Clinical Profile of Primary Immunodeficiency Disorders at a Tertiary Care Children Hospital in Southern India. Indian Pediatr 58, 246–249 (2021). https://doi.org/10.1007/s13312-021-2164-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13312-021-2164-z