Abstract
Background
Neurological manifestations of Chediak-Higashi syndrome mainly include peripheral neuropathy, ataxia, tremors, cranial nerve palsies, intellectual decline and seizures.
Case Characteristics
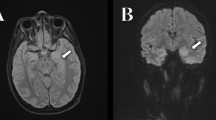
A 2 years 10 month old girl with silvery hair syndrome presented with sub-acute onset behavioral issues, ataxia and multiple type abnormal movements. Cerebrospinal fluid examination was positive for Anti NMDA receptor antibodies. Hair shaft examination and peripheral blood film findings were suggestive of Chediak Higashi syndrome.
Message
Anti NMDA receptor encephalitis may be associated with Chediak Higashi Syndrome.
Similar content being viewed by others
References
Rudramurthy P, Lokanatha H. Chediak-Higashi syndrome: A case series from Karnataka, India. Indian J Dermatol. 2015;60:52.
Kaplan J, De Domenico I, Ward DM. Chediak-Higashi syndrome. Curr Opin Hematol. 2008;15:22–9.
Mathis S, Cintas P, de Saint-Basile G, Magy L, Funalot B, Vallat JM. Motor neuronopathy in Chediak-Higashi syndrome. J Neurol Sci. 2014;15:203–7.
Introne WJ, Westbroek W, Groden CA, Bhambhani V, Golas GA, Baker EH, et al. Neurologic involvement in patients with atypical Chediak-Higashi disease. Neurology. 2017;88:e57–65.
Baizabal-Carvallo JF, Stocco A, Muscal E, Jankovic J. The spectrum of movement disorders in children with anti-NMDA receptor encephalitis. Mov Disord. 2013;28:543–7.
Hacohen Y, Wright S, Waters P, Agrawal S, Carr L, Cross H, et al. Paediatric autoimmune encephalopathies: Clinical features, laboratory investigations and outcomes in patients with or without antibodies to known central nervous system autoantigens. J Neurol Neurosurg Psychiatry. 2013;84:748–55.
Roy A, Kar R, Basu D, Srivani S, Badhe BA. Clinicohematological profile of Chediak-Higashi syndrome: Experience from a tertiary care center in south India. Indian J Pathol Microbiol. 2011;54:547–51.
Meena JP, Seth R, Chakrabarty B, Gulati S, Agrawala S, Naranje P. Neuroblastoma presenting as opsoclonus-myoclonus: A series of six cases and review of literature. J Pediatr Neurosci. 2016;11:373–7.
Khair AM, Ehlayel M, Alshami R, Mohamed K. Autoimmune encephalitis as the sole presentation of common variable immunodeficiency: First report in a child. J Clin Case Rep. 2015;5:665.
Akman CI, Patterson MC, Rubinstein A, Herzog R. Limbic encephalitis associated with anti-GAD antibody and common variable immune deficiency. Dev Med Child Neurol. 2009;51:563–7.
Funding
Funding: None; Competing interest: None stated.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bhardwaj, N., Gowda, V.K., Srinivas, S.M. et al. Association of Anti N-methyl-D-aspartate (NMDA) Receptor Encephalitis with Chediak-Higashi Syndrome. Indian Pediatr 56, 501–503 (2019). https://doi.org/10.1007/s13312-019-1577-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13312-019-1577-4