Abstract
Context
Suspecting metabolic liver disease in an infant or young child with acute liver failure, and a protocol-based workup for diagnosis is the need of the hour.
Evidence acquisition
Data over the last 15 years was searched through Pubmed using the keywords “Metabolic liver disease” and “Acute liver failure” with emphasis on Indian perspective. Those published in English language where full text was retrievable were included for this review.
Results
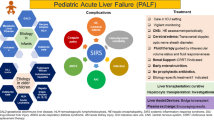
Metabolic liver diseases account for 13-43% cases of acute liver failure in infants and young children. Etiology remains indeterminate in very few cases of liver failure in studies where metabolic liver diseases were recognized in large proportion. Galactosemia, tyrosinemia and mitochondrial disorders in young children and Wilson’s disease in older children are commonly implicated. A high index of suspicion for metabolic liver diseases should be kept when there is strong family history of consanguinity, recurrent abortions or sibling deaths; and history of recurrent diarrhea, vomiting, failure to thrive or developmental delay. Simple dietary modifications and/or specific management can be life-saving if instituted promptly.
Conclusions
A high index of suspicion in presence of red flag symptoms and signs, and a protocol-based approach helps in timely diagnosis and prompt administration of lifesaving therapy.
Similar content being viewed by others
References
Alam S, Lal BB, Khanna R, Sood V, Rawat D. Acute liver failure in infants and young children in a specialized pediatric liver centre in India. Indian J Pediatr. 2015 Jan 6. [Epub ahead of print].
Rajanayagam J, Coman D, Cartwright D, Lewindon PJ. Pediatric acute liver failure: Etiology, outcomes, and the role of serial pediatric end-stage liver disease scores. Pediatr Transplant. 2013;17: 362–8.
Brett A, Pinto C, Carvalho L, Garcia P, Diogo L, Gonçalves I. Acute liver failure in under two year-olds–are there markers of metabolic disease on admission? Ann Hepatol. 2013;12: 791–6.
Sundaram SS, Alonso E, Narkewicz MR, Zhang S, Squires RH and Pediatric Acute Liver Failure Study Group. Characterization and outcome of young infants with acute liver failure. J Pediatr. 2011;159: 813–8.
Dhawan A. Etiology and prognosis of acute liver failure in children. Liver Transplant. 2008;14:S80–S4.
Squires RH, Shneider BL, Bucuvalas J, Alonso E, Sokol RJ, Narkewicz MR, et al. Acute liver failure in children: The first 348 patients in pediatric acute liver failure study group. J Pediatr. 2006;148: 652–8.
Durand P, Debray D, Mandel R, Baujard C, Branchereau S, Gauthier F, et al. Acute liver failure in infancy: A 14-year experience of a pediatric liver transplantation center. J Pediatr. 2001;139: 871–6.
Kaur S, Kumar P, Kumar V, Sarin SK, Kumar A. Etiology and prognostic factors of acute liver failure in children. Indian Pediatr. 2013;50: 677–9.
Lee WS, McKiernan P, Kelly DA. Etiology, outcome and prognostic indicators of childhood fulminant hepatic failure in the United Kingdom. J Pediatr Gastroenterol Nutr. 2005;40: 575–81.
Shanmugam NP, Bansal S, Greenough A, Verma A, Dhawan A. Neonatal liver failure-etiologies and management-state of the art. Eur J Pediatr. 2011;170: 573–81.
Narkewicz MR, DellOlio D, Karpen SJ, Murray KF, Schwarz K, Yazigi N, et al. Pattern of diagnostic evaluation for the causes of pediatric acute liver failure: an opportunity for quality improvement. J Pediatr. 2009;155: 801–6.
Poddar U, Thapa BR, Prasad A, Sharma AK, Singh K. Natural history and risk factors in fulminant hepatic failure. Arch Dis Child. 2002;87: 54–6.
Boles RG, Buck EA, Blitzer MG, Platt MS, Cowan TM, Martin SK, et al. Retrospective biochemical screening of fatty acid oxidation disorders in postmortem livers of 418 cases of sudden death in the first year of life. J Pediatr. 1998;132: 924–33.
Dimmock DP, Zhang Q, Dionisi-Vici C, Carrozzo R, Shieh J, Tang LY, et al. Clinical and molecular features of mitochondrial DNA depletion due to mutations in deoxyguanosine kinase. Hum Mutat. 2008;29: 330–1.
Korman JD, Volenberg I, Balko J, Webster J, Schiodt FV, Squires RH, et al. Screening for Wilson disease in acute liver failure: a comparison of currently available diagnostic tests. Hepatology. 2008;48: 1167–74.
Eurpean Association for Study of Liver. EASL Clinical Practice Guidelines: Wilson’s disease. J Hepatol. 2012;56: 671–85.
Rahimi RS, Singal AG, Cuthbert JA, Rockey DC. Lactulose vs polyethylene glycol 3350–electrolyte solution for treatment of overt hepatic encephalopathy: The HELP randomized clinical trial. JAMA Intern Med. 2014;174: 1727–33.
Als-Nielsen B, Gluud LL, Gluud C. Non-absorbable disaccharides for hepatic encephalopathy: Systematic review of randomised trials. BMJ. 2004;328: 1046.
Leise MD, Poterucha JJ, Kamath PS, Kim WR. Management of hepatic encephalopathy in the hospital. Mayo Clin Proc. 2014;89: 241–53.
Alba L, Hay JE, Angulo P, Lee WM. Lactulose therapy in acute liver failure. J Hepatol. 2002;36: 33A.
Sushma S, Dasarathy S, Tandon RK, Jain S, Gupta S, Bhist MS. Sodium benzoate in the treatment of acute hepatic encephalopathy: A double-blind randomized trial. Hepatology. 1992;16: 138–44.
Batshaw ML, Brusilow S, Waber L, Blom W, Brubakk AM, Burton BK, et al. Treatment of inborn errors of urea synthesis: activation of alternative pathways of waste nitrogen synthesis and excretion. N Engl J Med. 1982;306: 1387–92.
Schaefer B, Schaefer F, Engelmann G, Meyburg J, Heckert KH, Zorn M, et al. Comparison of Molecular Adsorbents Recirculating System (MARS) dialysis with combined plasma exchange and haemodialysis in children with acute liver failure. Nephrol Dial Transplant. 2011;26: 3633–9.
Liu JP, Gluud LL, Als-Nielsen B, Gluud C. Artificial and bioartificial support systems for liver failure. Cochrane Database Syst Rev. 2004;1:CD003628.
Bourgoin P, Merouani A, Phan V, Litalien C, Lallier M, Alvarez F, et al. Molecular absorbent recirculating system therapy (MARS) in pediatric acute liver failure: A single center experience. Pediatr Nephrol. 2014;29: 901–8.
Lai YC, Huang HP, Tsai IJ, Tsau YK. High-volume continuous venovenous hemofiltration as an effective therapy for acute management of inborn errors of metabolism in young children. Blood Purif. 2007;25: 303–8.
Westrope C, Morris K, Burford D, Morrison G. Continuous hemofiltration in the control of neonatal hyperammonemia: A 10-year experience. Pediatr Nephrol. 2010;25: 1725–30.
Mazariegos G, Shneider B, Burton B, Fox IJ, Hadzic N, Kishnani P, et al. Liver transplantation for pediatric metabolic diseases. Mol Genet Metab. 2014;111: 418–27.
Arnon R, Kerkar N, Davis MK, Anand R, Yin W, González-Peralta RP, et al. Liver transplantation in children with metabolic diseases: The studies of pediatric liver transplantation experience. Pediatr Transplant. 2010;14: 796–805
Stevenson T, Millan MT, Wayman K, Berquist WE, Sarwal M, Johnston EE, et al. Long-term outcome following pediatric liver transplantation for metabolic disorders. Pediatr Transplant. 2010;14: 268–75.
Dhawan A, Taylor RM, Cheeseman P, De Silva P, Katsiyiannakis L, Mieli-Vergani G. Wilson’s disease in children: 37-year experience and revised King’s score for liver transplantation. Liver Transplant. 2005;11: 441–8.
Devarbhavi H, Singh R, Adarsh CK, Sheth K, Kiran R, Patil M. Factors that predict mortality in children with Wilson disease associated acute liver failure and comparison of Wilson disease specific prognostic indices. J Gastroenterol Hepatol. 2014;29: 380–6.
Fischer RT, Soltys KA, Squires RH, Jaffe R, Mazariegos GV, Shneider BL. Prognostic scoring indices in Wilson disease: A case series and cautionary tale. J Pediatr Gastroenterol Nutr. 2011;52: 466–9.
Hughes RD, Mitry RR, Dhawan A. Current status of hepatocyte transplantation. Transplantation. 2012;93: 342–7.
Sokal EM. Treating inborn errors of liver metabolism with stem cells: Current clinical development. J Inherit Metab Dis. 2014;37: 535–9.
Cantz T, Sharma AD, Ott M. Concise review: Cell therapies for hereditary metabolic liver diseases -concepts, clinical results and future developments. Stem Cells. 2015;33: 1055–62.
De-Laet C, Dionisi-Vici C, Leonard JV, McKiernan P, Mitchell G, Monti L, et al. Recommendations for the management of tyrosinemia type 1. Orphanet J Rare Dis. 2013; 8:8.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Alam, S., Lal, B.B. Metabolic liver diseases presenting as acute liver failure in children. Indian Pediatr 53, 695–701 (2016). https://doi.org/10.1007/s13312-016-0913-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13312-016-0913-1