Abstract
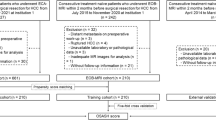
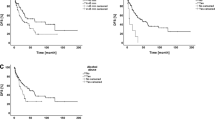
Few studies have assessed the clinical implications of the combination of different prognostic indicators for overall survival (OS) and disease-free survival (DFS) of resected hepatocellular carcinoma (HCC). This study aimed to evaluate the prognostic factors in HCC patients for OS and DFS outcomes and establish a nomogram-based prognostic model to predict the DFS of HCC. A multicenter, retrospective European study was conducted through the collection of data on 413 consecutive treated patients with a first diagnosis of HCC between January 2010 and December 2020. Univariate and multivariate Cox regression analyses were performed to identify all independent risk factors for OS and DFS outcomes. A nomogram prognostic staging model was subsequently established for DFS and its precision was verified internally by the concordance index (C-Index) and externally by calibration curves. For OS, multivariate Cox regression analysis indicated Child–Pugh B7 score (HR 4.29; 95% CI 1.74–10.55; p = 0.002) as an independent prognostic factor, along with Barcelona Clinic Liver Cancer (BCLC) stage ≥ B (HR 1.95; 95% CI 1.07–3.54; p = 0.029), microvascular invasion (MVI) (HR 2.54; 95% CI 1.38–4.67; p = 0.003), R1/R2 resection margin (HR 1.57; 95% CI 0.85–2.90; p = 0.015), and Clavien–Dindo Grade 3 or more (HR 2.73; 95% CI 1.44–5.18; p = 0.002). For DFS, multivariate Cox regression analysis indicated BCLC stage ≥ B (HR 2.15; 95% CI 1.34–3.44; p = 0.002) as an independent prognostic factor, along with multiple nodules (HR 2.04; 95% CI 1.25–3.32; p = 0.004), MVI (HR 1.81; 95% CI 1.19–2.75; p = 0.005), satellite nodules (HR 1.63; 95% CI 1.09–2.45; p = 0.018), and R1/R2 resection margin (HR 3.39; 95% CI 2.19–5.25; < 0.001). The C-Index of the nomogram, tailored based on the previous significant factors, showed good accuracy (0.70). Internal and external calibration curves for the probability of DFS rate showed optimal consistency and fit well between the nomogram-based prediction and actual observations. MVI and R1/R2 resection margins should be considered as significant OS and DFS predictors, while satellite nodules should be included as a significant DFS predictor. The nomogram-based prognostic model for DFS provides a more effective prognosis assessment for resected HCC patients, allowing for individualized treatment plans.





Similar content being viewed by others
Data availability
Data are available on request to the corresponding author.
References
Rawla P, Sunkara T, Muralidharan P, Raj JP (2018) Update in global trends and aetiology of hepatocellular carcinoma. Contemp Oncol (Pozn) 22(3):141–150. https://doi.org/10.5114/wo.2018.78941
Yang JD, Hainaut P, Gores GJ, Amadou A, Plymoth A, Roberts LR (2019) A global view of hepatocellular carcinoma: trends, risk, prevention and management. Nat Rev Gastroenterol Hepatol 16(10):589–604. https://doi.org/10.1038/s41575-019-0186-y
Siegel RL, Miller KD, Jemal A (2018) Cancer statistics, 2018. CA Cancer J Clin 68(1):7–30. https://doi.org/10.3322/caac.21442
Faber W, Sharafi S, Stockmann M et al (2013) Long-term results of liver resection for hepatocellular carcinoma in noncirrhotic liver. Surgery 153(4):510–517. https://doi.org/10.1016/j.surg.2012.09.015
Hanazaki K, Kajikawa S, Shimozawa N et al (2000) Survival and recurrence after hepatic resection of 386 consecutive patients with hepatocellular carcinoma. J Am Coll Surg 191(4):381–388. https://doi.org/10.1016/s1072-7515(00)00700-6
Saito A, Toyoda H, Kobayashi M et al (2021) Prediction of early recurrence of hepatocellular carcinoma after resection using digital pathology images assessed by machine learning. Mod Pathol 34(2):417–425. https://doi.org/10.1038/s41379-020-00671-z
Levy I, Sherman M (2002) Staging of hepatocellular carcinoma: assessment of the CLIP, Okuda, and Child-Pugh staging systems in a cohort of 257 patients in Toronto. Gut 50(6):881. https://doi.org/10.1136/gut.50.6.881
Tokumitsu Y, Nagano H (2016) Current HCC staging systems: their uses and limitations. In: Carr BI (ed) Hepatocellular carcinoma: diagnosis and treatment. Springer International Publishing, pp 425–442
Grieco A, Pompili M, Caminiti G et al (2005) Prognostic factors for survival in patients with early-intermediate hepatocellular carcinoma undergoing non-surgical therapy: comparison of Okuda, CLIP, and BCLC staging systems in a single Italian centre. Gut 54(3):411–418. https://doi.org/10.1136/gut.2004.048124
Reig M, Forner A, Rimola J et al (2022) BCLC strategy for prognosis prediction and treatment recommendation: the 2022 update. J Hepatol 76(3):681–693. https://doi.org/10.1016/j.jhep.2021.11.018
Yi PS, Zhang M, Zhao JT, Xu MQ (2016) Liver resection for intermediate hepatocellular carcinoma. World J Hepatol 8(14):607–615. https://doi.org/10.4254/wjh.v8.i14.607
Kariyama K, Nouso K, Wakuta A et al (2020) Treatment of intermediate-stage hepatocellular carcinoma in Japan: position of curative therapies. Liver Cancer 9(1):41–49. https://doi.org/10.1159/000502479
Han J, Li Z-L, Xing H et al (2019) The impact of resection margin and microvascular invasion on long-term prognosis after curative resection of hepatocellular carcinoma: a multi-institutional study. HPB 21(8):962–971. https://doi.org/10.1016/j.hpb.2018.11.005
Ma L, Deng K, Zhang C et al (2022) Nomograms for predicting hepatocellular carcinoma recurrence and overall postoperative patient survival. Orig Res Front Oncol. https://doi.org/10.3389/fonc.2022.843589
Zhang W, Chen J, Liu L, Wang L, Liu J, Su D (2019) Prognostic value of preoperative computed tomography in HBV-related hepatocellular carcinoma patients after curative resection. Onco Targets Ther 12:3791–3804. https://doi.org/10.2147/ott.S199136
Zhang W, Tan Y, Shen S et al (2017) Prognostic nomogram for hepatocellular carcinoma in adolescent and young adult patients after hepatectomy. Oncotarget 8(63):106393–106404. https://doi.org/10.18632/oncotarget.18192
Vandenbroucke JP, von Elm E, Altman DG et al (2007) Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. Epidemiology 18(6):805–835. https://doi.org/10.1097/EDE.0b013e3181577511
Little JP (1995) Consistency of ASA grading. Anaesthesia 50(7):658–659
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40(5):373–383. https://doi.org/10.1016/0021-9681(87)90171-8
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213. https://doi.org/10.1097/01.sla.0000133083.54934.ae
Malinchoc M, Kamath PS, Gordon FD, Peine CJ, Rank J, ter Borg PCJ (2000) A model to predict poor survival in patients undergoing transjugular intrahepatic portosystemic shunts. Hepatology 31(4):864–871. https://doi.org/10.1053/he.2000.5852
Andreou A, Knitter S, Schmelzle M et al (2021) Recurrence at surgical margin following hepatectomy for colorectal liver metastases is not associated with R1 resection and does not impact survival. Surgery. 169(5):1061–1068. https://doi.org/10.1016/j.surg.2020.11.024
Andreou A, Aloia TA, Brouquet A et al (2013) Margin status remains an important determinant of survival after surgical resection of colorectal liver metastases in the era of modern chemotherapy. Ann Surg 257(6):1079–1088. https://doi.org/10.1097/SLA.0b013e318283a4d1
Govalan R, Lauzon M, Luu M et al (2021) Comparison of surgical resection and systemic treatment for hepatocellular carcinoma with vascular invasion: national cancer database analysis. Liver Cancer 10(5):407–418. https://doi.org/10.1159/000515554
Strasberg SM, Belghiti J, Clavien PA et al (2000) The brisbane 2000 terminology of liver anatomy and resections. HPB. 2(3):333–339. https://doi.org/10.1016/S1365-182X(17)30755-4
Famularo S, Di Sandro S, Giani A et al (2018) Long-term oncologic results of anatomic vs. parenchyma-sparing resection for hepatocellular carcinoma. A propensity score-matching analysis. Eur J Surg Oncol. 44(10):1580–1587. https://doi.org/10.1016/j.ejso.2018.05.018
Famularo S, Giani A, Di Sandro S et al (2018) Does the pringle maneuver affect survival and recurrence following surgical resection for hepatocellular carcinoma? A western series of 441 patients. J Surg Oncol 117(2):198–206. https://doi.org/10.1002/jso.24819
Famularo S, Piardi T, Molfino S et al (2021) Factors affecting local and intra hepatic distant recurrence after surgery for Hcc: an alternative perspective on microvascular invasion and satellitosis—a Western European Multicentre Study. J Gastrointest Surg 25(1):104–111. https://doi.org/10.1007/s11605-019-04503-7
Zhang Z, Kattan MWK (2017) Drawing nomograms with R: applications to categorical outcome and survival data. Ann Transl Med 5(10):9
Wang CY, Li S (2019) Clinical characteristics and prognosis of 2887 patients with hepatocellular carcinoma: a single center 14 years experience from China. Med (Baltim) 98(4):e14070. https://doi.org/10.1097/md.0000000000014070
Xiang Y-J, Wang K, Zheng Y-T et al (2021) Prognostic value of microvascular invasion in eight existing staging systems for hepatocellular carcinoma: a bi-centeric retrospective cohort study. Orig Res Front Oncol. https://doi.org/10.3389/fonc.2021.726569
Portolani N, Coniglio A, Ghidoni S et al (2006) Early and late recurrence after liver resection for hepatocellular carcinoma: prognostic and therapeutic implications. Ann Surg 243(2):229–235. https://doi.org/10.1097/01.sla.0000197706.21803.a1
Zheng J, Chou JF, Gönen M et al (2017) Prediction of hepatocellular carcinoma recurrence beyond milan criteria after resection: validation of a clinical risk score in an international cohort. Ann Surg 266(4):693–701. https://doi.org/10.1097/sla.0000000000002360
Roayaie S, Blume IN, Thung SN et al (2009) A system of classifying microvascular invasion to predict outcome after resection in patients with hepatocellular carcinoma. Gastroenterology 137(3):850–855. https://doi.org/10.1053/j.gastro.2009.06.003
Xu XF, Yu JJ, Xing H, Shen F, Yang T (2017) How to better predict microvascular invasion and recurrence of hepatocellular carcinoma. J Hepatol 67(5):1119–1120. https://doi.org/10.1016/j.jhep.2017.06.034
Sumie S, Kuromatsu R, Okuda K et al (2008) Microvascular invasion in patients with hepatocellular carcinoma and its predictable clinicopathological factors. Ann Surg Oncol 15(5):1375–1382. https://doi.org/10.1245/s10434-008-9846-9
Sumie S, Nakashima O, Okuda K et al (2014) The significance of classifying microvascular invasion in patients with hepatocellular carcinoma. Ann Surg Oncol 21(3):1002–1009. https://doi.org/10.1245/s10434-013-3376-9
Zhang X, Li J, Shen F, Lau WY (2018) Significance of presence of microvascular invasion in specimens obtained after surgical treatment of hepatocellular carcinoma. J Gastroenterol Hepatol 33(2):347–354. https://doi.org/10.1111/jgh.13843
Lim KC, Chow PK, Allen JC et al (2011) Microvascular invasion is a better predictor of tumor recurrence and overall survival following surgical resection for hepatocellular carcinoma compared to the Milan criteria. Ann Surg 254(1):108–113. https://doi.org/10.1097/SLA.0b013e31821ad884
Zhou J, Sun H, Wang Z et al (2020) Guidelines for the diagnosis and treatment of hepatocellular carcinoma (2019 Edition). Liver Cancer. 9(6):682–720. https://doi.org/10.1159/000509424
Huang C, Zhu XD, Ji Y et al (2017) Microvascular invasion has limited clinical values in hepatocellular carcinoma patients at Barcelona Clinic Liver Cancer (BCLC) stages 0 or B. BMC Cancer 17(1):58. https://doi.org/10.1186/s12885-017-3050-x
Shi M, Guo RP, Lin XJ et al (2007) Partial hepatectomy with wide versus narrow resection margin for solitary hepatocellular carcinoma: a prospective randomized trial. Ann Surg 245(1):36–43. https://doi.org/10.1097/01.sla.0000231758.07868.71
Harimoto N, Shirabe K, Ikegami T et al (2015) Postoperative complications are predictive of poor prognosis in hepatocellular carcinoma. J Surg Res 199(2):470–477. https://doi.org/10.1016/j.jss.2015.06.012
Kabir T, Syn NL, Tan ZZX et al (2020) Predictors of post-operative complications after surgical resection of hepatocellular carcinoma and their prognostic effects on outcome and survival: a propensity-score matched and structural equation modelling study. Eur J Surg Oncol 46(9):1756–1765. https://doi.org/10.1016/j.ejso.2020.03.219
Chok KSH, Chan MMY, Dai WC et al (2017) Survival outcomes of hepatocellular carcinoma resection with postoperative complications—a propensity-score-matched analysis. Med (Baltim) 96(12):e6430. https://doi.org/10.1097/md.0000000000006430
Fukuda S, Itamoto T, Amano H et al (2007) Clinicopathologic features of hepatocellular carcinoma patients with compensated cirrhosis surviving more than 10 years after curative hepatectomy. World J Surg 31(2):345–352. https://doi.org/10.1007/s00268-006-0513-7
Li J, Han X, Yu X et al (2018) Clinical applications of liquid biopsy as prognostic and predictive biomarkers in hepatocellular carcinoma: circulating tumor cells and circulating tumor DNA. J Exp Clin Cancer Res. 37(1):213. https://doi.org/10.1186/s13046-018-0893-1
Sun YF, Guo W, Xu Y et al (2018) Circulating tumor cells from different vascular sites exhibit spatial heterogeneity in epithelial and mesenchymal composition and distinct clinical significance in hepatocellular carcinoma. Clin Cancer Res 24(3):547–559. https://doi.org/10.1158/1078-0432.Ccr-17-1063
Plessier A, Codes L, Consigny Y et al (2004) Underestimation of the influence of satellite nodules as a risk factor for post-transplantation recurrence in patients with small hepatocellular carcinoma. Liver Transpl 10(2 Suppl 1):S86-90. https://doi.org/10.1002/lt.20039
Ünal E, İdilman İS, Akata D, Özmen MN, Karçaaltıncaba M (2016) Microvascular invasion in hepatocellular carcinoma. Diagn Interv Radiol 22(2):125–132. https://doi.org/10.5152/dir.2015.15125
Hu H, Qi S, Zeng S et al (2021) Importance of microvascular invasion risk and tumor size on recurrence and survival of hepatocellular carcinoma after anatomical resection and non-anatomical resection. Orig Res Front Oncol. https://doi.org/10.3389/fonc.2021.621622
Yang P, Si A, Yang J et al (2019) A wide-margin liver resection improves long-term outcomes for patients with HBV-related hepatocellular carcinoma with microvascular invasion. Surgery 165(4):721–730. https://doi.org/10.1016/j.surg.2018.09.016
Zhou KQ, Sun YF, Cheng JW et al (2020) Effect of surgical margin on recurrence based on preoperative circulating tumor cell status in hepatocellular carcinoma. EBioMedicine 62:103107. https://doi.org/10.1016/j.ebiom.2020.103107
Liu PH, Hsu CY, Hsia CY et al (2016) Prognosis of hepatocellular carcinoma: assessment of eleven staging systems. J Hepatol 64(3):601–608. https://doi.org/10.1016/j.jhep.2015.10.029
Li J, Tao H-S, Li J et al (2021) Effect of severity of liver cirrhosis on surgical outcomes of hepatocellular carcinoma after liver resection and microwave coagulation. Orig Res Front Oncol. https://doi.org/10.3389/fonc.2021.745615
Yamamoto J, Kosuge T, Takayama T et al (1994) Perioperative blood transfusion promotes recurrence of hepatocellular carcinoma after hepatectomy. Surgery 115(3):303–309
Hsu H-Y, Yu M-C, Lee C-W et al (2017) RAM score is an effective predictor for early mortality and recurrence after hepatectomy for hepatocellular carcinoma. BMC Cancer. 17(1):742. https://doi.org/10.1186/s12885-017-3748-9
Funding
All authors declare no sources of funding for this study.
Author information
Authors and Affiliations
Contributions
Conceptualization, BI; Methodology, YM, MYHX, FB, MP, BI; Validation, PSV, AP, KYX, MDM, BI; Formal Analysis, YM, MYHX, FB; Investigation, YM, MYHX, BI; Resources, YM, MYX, BI; Data Curation, YM, MYHX, FB, PSV, MP, AP, KYX, MDM, FR, SF, CF, GG, TP, DS, LG, SM, GB, BI; Writing—Original Draft Preparation, YM, MY, FB, PSV, MP, AP, BI; Writing—Review and Editing, YM, MYHX, FB, PSV, MP, AP, KYX, MDM, GKPB, TEK, TJY, FR, SF, CF, GG, TP, DS, LG, SM, GB, BI; Visualization, BI; Supervision, BI; Project Administration, YM, MYHX, BI.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no competing interests.
Research involving human participants and/or animals, and Informed consent
The need to obtain informed consent from participants was waived owing to the retrospective nature of the study. The study was conducted in accordance with the Declaration of Helsinki and was conducted and reported in accordance with the STROBE guidelines for cohort studies.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Masuda, Y., Yeo, M., Burdio, F. et al. Factors affecting overall survival and disease-free survival after surgery for hepatocellular carcinoma: a nomogram-based prognostic model—a Western European multicenter study. Updates Surg 76, 57–69 (2024). https://doi.org/10.1007/s13304-023-01656-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-023-01656-8