Abstract
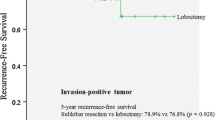
Controversy still exists regarding the staging of non-small cell lung cancer (NSCLC) with adjacent lobe invasion (T-ALI) according to the TNM system in terms of T factor and the appropriate surgical resection method. We performed an analysis to compare the prognosis of T-ALI with T2 and T3 disease and to see the effect of our surgical method for these tumors. Two hundred consecutive patients between January 2012 and November 2020, with anatomical lobectomy for T2 or T3 tumor (Group-1) and non-anatomical lobectomy resection (lobectomy plus wedge resection [LWR]) (Group-2) for T-ALI (T2-ALI and T3-ALI) due to primary NSCLC, who did not have lymph node metastases were analyzed retrospectively. All surgeries were performed by two experienced surgeons who adopted the same surgical technique. Those who underwent additional segmentectomy and bilobectomy due to fissure invasion were excluded from the study. Overall survival rates of all patients were determined and factors affecting survival were evaluated by performing univariate and multivariate analyses. Of the patients with a mean age of 62.2 ± 7.8 years, 175 (87.5%) were male and 25 (12.5%) were female. There were 137 (68.5%) patients in Group 1 and 63 (31.5%) patients in Group 2. The mean tumor size in Group 1 (4.4 ± 1.4 cm) was significantly smaller than that in Group 2 (4.9 ± 1.4 cm) (p = 0.014). When T distribution within the groups was considered, the rate of pathological T3 in Group 1 (33.6%) was significantly lower than that in Group 2 (55.6%) (p = 0.005). While the 5-year overall survival rate was 70.1% in Group 1, it was 50.6% in Group 2 (p = 0.022). When tumors were grouped as T2, T2-ALI, T3, and T3-ALI according to T factor, the 5-year overall survival rates were 71.4% and 67.8% in T2 and T3 tumors, respectively, and 49.2% and 51.5% in T2-ALI and T3-ALI tumors, respectively. In the multivariate analysis of these four groups, the overall survival rates for T2-ALI and T3-ALI were significantly lower than those of T2 tumors (p = 0.046 and p = 0.025, respectively). In the analysis made between the T2 tumor group and the new T3 group (T2-ALI, T3, T3-ALI), which was formed by upgrading T2-ALI tumors to the T3 group, T2 tumors were found to have a significantly better survival rate (p = 0.019). The disease-free survival of pT2 patients and new T3 group patients was statistically significant, 63.7% and 45.7%, respectively (p = 0.050). Our results suggest that LWR for T-ALI can be performed with acceptable oncologic outcomes when compared to anatomical lobectomy. T2-ALI has a worse overall survival than T2 tumor and offers a similar prognosis to T3. Given this situation, it is more appropriate to classify T2-ALI as T3. Further studies based on larger series are needed to confirm these preliminary data.


Similar content being viewed by others
Data availability
Data supporting the findings of this study are available from the corresponding author upon reasonable request.
References
Goldstraw P, Chansky K, Crowley J, Rami-Porta R, Asamura H, Eberhardt WEE et al (2016) The IASLC Lung Cancer Staging Project: proposals for revision of the TNM stage groupings in the forthcoming (eighth) edition of the TNM classification for lung cancer. J Thorac Oncol 11:39–51
Xiao Z, Cao C, Mei J, Liao H, Yan T, Liu L (2016) Should tumor with direct adjacent lobe invasion (Tdali) be assigned to T2 or T3 in non-small cell lung cancer: a metaanalysis. J Thorac Dis 8:1956–1965
Cai JS, Lin QY, Dou XM (2022) Is adjacent lobe invasion an T category upgrade factor for resected non-small cell lung cancer ≤ 5 cm? J Cancer Res Clin Oncol. https://doi.org/10.1007/s00432-022-04102-1
Riquet M, Berna P, Arame A, Mordant P, Pereira JCDN, Foucault C et al (2012) Lung cancer invading the fissure to the adjacent lobe: more a question of spreading mode than a staging problem. Eur J Cardiothorac Surg 41:1047–1051
Kanzaki R, Ikeda N, Okura E, Kitahara N, Shintani Y, Okimura A et al (2012) Surgical results and staging of non-small cell lung cancer with interlobar pleural invasion. Interact Cardiovasc Thorac Surg 14:739–742
Dziedzic D, Rudzinski P, Langfort R, Orlowski T, on behalf of the Polish Lung Cancer Study Group (PLCSG) (2016) Results of surgical treatment and impact on T staging of non-small-cell lung cancer adjacent lobe invasion. Eur J Cardiothorac Surg 50:423–427
Smith SP, Bograd AJ, Levy G, Chang SC, Farivar AS, Aye RW et al (2021) Surgical management of non-small cell lung cancer invading the fissure: less is more? Ann Thorac Surg 111:231–236
Yang HX, Hou X, Lin P, Yang H, Zeng CG, Rong TH et al (2009) Peripheral direct adjacent lobe invasion non-small cell lung cancer has a similar survival to that of parietal pleural invasion T3 disease. J Thorac Oncol 4:1342–1346
Okada M, Tsubota N, Yoshimura M, Miyamoto Y, Matsuoka H (1999) How should interlobar pleural invasion be classified? Prognosis of resected T3 non-small cell lung cancer. Ann Thorac Surg 68:2049–2052
Nonaka M, Kataoka D, Yamamoto S, Horichi N, Ohgiya Y, Kushima M et al (2005) Outcome following surgery for primary lung cancer with interlobar pleural invasion. Surg Today 35:22–27
Haam SJ, Park IK, Paik HC, Kim DJ, Lee DY, Lee JG et al (2012) T-stage of non-small cell lung cancer directly invading an adjacent lobe. Eur J Cardiothorac Surg 42:807–810
Leuzzi G, Cesario A, Cafarotti S, Lococo F, Dall’Armi V, Novellis P, et al (2014) Surgical treatment in patient with non-small-cell lung cancer with fissure involvement: anatomical versus nonanatomical resection. J Thorac Oncol 9:97–108
Demir A, Gunluoglu MZ, Sansar D, Melek H, Dincer SI (2007) Staging and resection of lung cancer with minimal invasion of the adjacent lobe. Eur J Cardiothorac Surg 32:855–858
Andreetti C, Poggi C, Ibrahim M, D’Andrilli A, Maurizi G, Tiracorrendo M et al (2020) Surgical treatment of lung cancer with adjacent lobe invasion in relation to fissure integrity. Thorac Cancer 11:232–242
Miura H, Taira O, Uchida O, Kato H (1998) Invasion beyond interlobar pleura in non-small cell lung cancer. Chest 114:1301–1304
Liu M, Wigle D, Wampfler JA, Dai J, Stoddard SM, Xue Z et al (2017) T category of non-small cell lung cancer invading the fissure to the adjacent lobe. J Thorac Cardiovasc Surg 154:1777–1783
Joshi V, McShane J, Page R, Carr M, Mediratta N, Shackcloth M et al (2011) Clinical upstaging of non-small cell lung cancer that extends across the fissure: implications for non-small cell lung cancer staging. Ann Thorac Surg 91:350–353
Ohtaki Y, Hishida T, Yoshida J, Ishii G, Kawase A, Aokage K et al (2013) The clinical outcome of non-small cell lung cancer patients with adjacent lobe invasion: the optimal classification according to the status of the interlobar pleura at the invasion point. Eur J Cardiothorac Surg 43:302–309
Acknowledgements
None.
Funding
There is no specific funding related to this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Informed consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008. Informed consent was obtained from all participants.
Research involving human participants and/or animals
The ethics committee of our hospital (2020-CREC-139) approved the protocol for the current study. All patients gave written informed consent for surgical treatment and were aware that all information could be used anonymously for scientific purposes only.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ucvet, A., Yazgan, S., Agaoglu Sanli, B. et al. Adjacent lobe invasion of T2 tumor in non-small cell lung cancer has T3 disease-like survival fissure invasion: T2 or T3?. Updates Surg 75, 2017–2025 (2023). https://doi.org/10.1007/s13304-023-01616-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-023-01616-2