Abstract
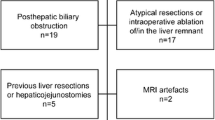
Post hepatectomy liver failure (PHLF) could occur even though an adequate liver volume is preserved. Liver function is not strictly related to the volume and the necessity to pre-operatively predict the future liver remnant (FLR) function is emerging, together with the wide spreading of techniques, aiming to optimize the FLR. The aim of this study was to systematically review all the available tests, to pre-operatively assess the liver function and to estimate the risk of PHLF. A systematic literature research of Medline, Embase, Scopus was performed in accordance to the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines, to identify all the studies available for pre-operative liver function tests to assess the risk of PHLF and/or complications. From the 1122 references retrieved, 79 were included in the review. Dynamic functional tests, such as indocyanine green test (ICG), could evaluate only global liver function, with no definition of functional capacity of the remnant. Magnetic resonance imaging (MRI) with liver-specific contrast agents enables both liver function and volume evaluation; the absence of ionizing radiation showed a better patient’s compliance. Nuclear imaging studies as hepatobiliary scintigraphy (HBS) present the unique ability to allow a precise evaluation of the segmental liver function of the remnant liver. Liver volume could overestimate liver function. Several liver function tests are available to evaluate the risk of PHLF in the pre-operative setting. However, no single test alone could accurately predict PHLF. Pre-operative combination between a dynamic quantitative test, such as ICG, with MRI or HBS, should enable a more complete functional evaluation. Functional tests to predict PHLF should be chosen according to patient’s characteristics, disease, and center experience.

Similar content being viewed by others
References
Bennink RJ, Dinant S, Erdogan D, Heijnen BH, Straatsburg IH, van Vliet AK, van Gulik TM (2004) Preoperative assessment of postoperative remnant liver function using hepatobiliary scintigraphy. J Nucl Med 45(6):965–971
Tomassini F, D'Asseler Y, Giglio MC, Lecluyse C, Lambert B, Sainz-Barriga M, Van Dorpe J, Hoorens A, Geboes K, Troisi RI (2019) Hemodynamic changes in ALPPS influence liver regeneration and function: results from a prospective study. HPB Off J Int Hepato Pancreato Biliary Assoc 21(5):557–565. https://doi.org/10.1016/j.hpb.2018.09.005
Chapelle T, Op de Beeck B, Driessen A, Roeyen G, Bracke B, Hartman V, Huyghe I, Morrison S, Ysebaert D, Francque S (2017) Estimation of the future remnant liver function is a better tool to predict post-hepatectomy liver failure than platelet-based liver scores. Eur J Surg Oncol 43(12):2277–2284. https://doi.org/10.1016/j.ejso.2017.08.009
Olthof PB, Coelen RJS, Bennink RJ, Heger M, Lam MF, Besselink MG, Busch OR, van Lienden KP, van Gulik TM (2017) (99m)Tc-mebrofenin hepatobiliary scintigraphy predicts liver failure following major liver resection for perihilar cholangiocarcinoma. HPB Off J Int Hepato Pancreato Biliary Assoc 19(10):850–858. https://doi.org/10.1016/j.hpb.2017.05.007
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2010) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg 8(5):336–341. https://doi.org/10.1016/j.ijsu.2010.02.007
Wagener G (2013) Assessment of hepatic function, operative candidacy, and medical management after liver resection in the patient with underlying liver disease. Semin Liver Dis 33(3):204–212. https://doi.org/10.1055/s-0033-1351777
Mizuguchi T, Kawamoto M, Meguro M, Hui TT, Hirata K (2014) Preoperative liver function assessments to estimate the prognosis and safety of liver resections. Surg Today 44(1):1–10. https://doi.org/10.1007/s00595-013-0534-4
Ge PL, Du SD, Mao YL (2014) Advances in preoperative assessment of liver function. Hepatobiliary Pancreat Dis Int 13(4):361–370. https://doi.org/10.1016/s1499-3872(14)60267-8
de Graaf W, Bennink RJ, Vetelainen R, van Gulik TM (2010) Nuclear imaging techniques for the assessment of hepatic function in liver surgery and transplantation. J Nucl Med 51(5):742–752. https://doi.org/10.2967/jnumed.109.069435
Rassam F, Olthof PB, Bennink RJ, van Gulik TM (2017) Current modalities for the assessment of future remnant liver function. Visc Med 33(6):442–448. https://doi.org/10.1159/000480385
Ba-Ssalamah A, Bastati N, Wibmer A, Fragner R, Hodge JC, Trauner M, Herold CJ, Bashir MR, Van Beers BE (2017) Hepatic gadoxetic acid uptake as a measure of diffuse liver disease: Where are we? J Magn Reson Imaging 45(3):646–659. https://doi.org/10.1002/jmri.25518
Cieslak KP, Runge JH, Heger M, Stoker J, Bennink RJ, van Gulik TM (2014) New perspectives in the assessment of future remnant liver. Dig Surg 31(4–5):255–268. https://doi.org/10.1159/000364836
Ren Z, Xu Y, Zhu S (2012) Indocyanine green retention test avoiding liver failure after hepatectomy for hepatolithiasis. Hepatogastroenterology 59(115):782–784. https://doi.org/10.5754/hge11453
Uchiyama K, Mori K, Tabuse K, Ueno M, Ozawa S, Nakase T, Kawai M, Tani M, Tanimura H, Yamaue H (2008) Assessment of liver function for successful hepatectomy in patients with hepatocellular carcinoma with impaired hepatic function. J Hepato-Biliary-Pancreat Surg 15(6):596–602. https://doi.org/10.1007/s00534-007-1326-2
Sugimoto H, Okochi O, Hirota M, Kanazumi N, Nomoto S, Inoue S, Takeda S, Nakao A (2006) Early detection of liver failure after hepatectomy by indocyanine green elimination rate measured by pulse dye-densitometry. J Hepato-Biliary-Pancreat Surg y 13(6):543–548. https://doi.org/10.1007/s00534-006-1114-4
Wakabayashi H, Yachida S, Maeba T, Maeta H (2002) Evaluation of liver function for the application of preoperative portal vein embolization on major hepatic resection. Hepatogastroenterology 49(46):1048–1052
Fan ST (2002) Methods and related drawbacks in the estimation of surgical risks in cirrhotic patients undergoing hepatectomy. Hepatogastroenterology 49(43):17–20
Lam CM, Fan ST, Lo CM, Wong J (1999) Major hepatectomy for hepatocellular carcinoma in patients with an unsatisfactory indocyanine green clearance test. Br J Surg 86(8):1012–1017. https://doi.org/10.1046/j.1365-2168.1999.01204.x
Torzilli G, Makuuchi M, Inoue K, Takayama T, Sakamoto Y, Sugawara Y, Kubota K, Zucchi A (1999) No-mortality liver resection for hepatocellular carcinoma in cirrhotic and noncirrhotic patients: is there a way? A prospective analysis of our approach. Arch Surg 134(9):984–992. https://doi.org/10.1001/archsurg.134.9.984
Lau H, Man K, Fan ST, Yu WC, Lo CM, Wong J (1997) Evaluation of preoperative hepatic function in patients with hepatocellular carcinoma undergoing hepatectomy. Br J Surg 84(9):1255–1259
Okamoto E, Kyo A, Yamanaka N, Tanaka N, Kuwata K (1984) Prediction of the safe limits of hepatectomy by combined volumetric and functional measurements in patients with impaired hepatic function. Surgery 95(5):586–592
Mizumoto R, Kawarada Y, Noguchi T (1979) Preoperative estimation of operative risk in liver surgery, with special reference to functional reserve of the remnant liver following major hepatic resection. Jpn J Surg 9(4):343–349. https://doi.org/10.1007/bf02468635
Le Roy B, Gregoire E, Cosse C, Serji B, Golse N, Adam R, Cherqui D, Mabrut JY, Le Treut YP, Vibert E (2018) Indocyanine green retention rates at 15 min predicted hepatic decompensation in a western population. World J Surg 42(8):2570–2578. https://doi.org/10.1007/s00268-018-4464-6
Ibis C, Albayrak D, Sahiner T, Soytas Y, Gurtekin B, Sivrikoz N (2017) Value of preoperative indocyanine green clearance test for predicting post-hepatectomy liver failure in noncirrhotic patients. Med Sci Monit 23:4973–4980. https://doi.org/10.12659/msm.907306
Derpapas MK, Contis J, Fragulidis GP, Lykoudis PM, Polymeneas G, Ntourakis S, Voros D (2013) Correlation of the ICG test with risk factors and postoperative outcomes following hepatic resection. J Balkan Union Oncol 18(3):703–707
Greco E, Nanji S, Bromberg IL, Shah S, Wei AC, Moulton CA, Greig PD, Gallinger S, Cleary SP (2011) Predictors of peri-operative morbidity and liver dysfunction after hepatic resection in patients with chronic liver disease. HPB 13(8):559–565. https://doi.org/10.1111/j.1477-2574.2011.00329.x
Scheingraber S, Richter S, Igna D, Flesch S, Kopp B, Schilling MK (2008) Indocyanine green disappearance rate is the most useful marker for liver resection. Hepatogastroenterology 55(85):1394–1399
Zoedler T, Ebener C, Becker H, Roeher HD (1995) Evaluation of liver function tests to predict operative risk in liver surgery. HPB Surg 9(1):13–18. https://doi.org/10.1155/1995/47538
de Liguori CN, O'Reilly DA, Dajani K, Ghaneh P, Poston GJ, Wu AV (2009) Perioperative use of the LiMON method of indocyanine green elimination measurement for the prediction and early detection of post-hepatectomy liver failure. Eur J Surg Oncol 35(9):957–962. https://doi.org/10.1016/j.ejso.2009.02.003
Thomas MN, Weninger E, Angele M, Bosch F, Pratschke S, Andrassy J, Rentsch M, Stangl M, Hartwig W, Werner J, Guba M (2015) Intraoperative simulation of remnant liver function during anatomic liver resection with indocyanine green clearance (LiMON) measurements. HPB 17(6):471–476. https://doi.org/10.1111/hpb.12380
Weinberg L, Robinson C, Goh SK, Muralidharan V (2018) Use of indocyanine green dye clearance in a patient with liver cirrhosis undergoing hepatectomy: a clinical image. BMJ Case Rep. https://doi.org/10.1136/bcr-2018-225503
Okochi O, Kaneko T, Sugimoto H, Inoue S, Takeda S, Nakao A (2002) ICG pulse spectrophotometry for perioperative liver function in hepatectomy. J Surg Res 103(1):109–113. https://doi.org/10.1006/jsre.2001.6328
Kambakamba P, Stocker D, Reiner CS, Nguyen-Kim TD, Linecker M, Eshmuminov D, Petrowsky H, Clavien PA, Lesurtel M (2016) Liver kinetic growth rate predicts postoperative liver failure after ALPPS. HPB 18(10):800–805. https://doi.org/10.1016/j.hpb.2016.07.005
Yokoyama Y, Ebata T, Igami T, Sugawara G, Mizuno T, Yamaguchi J, Nagino M (2016) The predictive value of indocyanine green clearance in future liver remnant for posthepatectomy liver failure following hepatectomy with extrahepatic bile duct resection. World J Surg 40(6):1440–1447. https://doi.org/10.1007/s00268-016-3441-1
Miyagawa S, Makuuchi M, Kawasaki S, Kakazu T (1995) Criteria for safe hepatic resection. Am J Surg 169(6):589–594. https://doi.org/10.1016/s0002-9610(99)80227-x
Wang YY, Zhao XH, Ma L, Ye JZ, Wu FX, Tang J, You XM, Xiang BD, Li LQ (2018) Comparison of the ability of Child–Pugh score, MELD score, and ICG-R15 to assess preoperative hepatic functional reserve in patients with hepatocellular carcinoma. J Surg Oncol 118(3):440–445. https://doi.org/10.1002/jso.25184
Yokoyama Y, Nishio H, Ebata T, Igami T, Sugawara G, Nagino M (2010) Value of indocyanine green clearance of the future liver remnant in predicting outcome after resection for biliary cancer. Br J Surg 97(8):1260–1268. https://doi.org/10.1002/bjs.7084
Kim HJ, Kim CY, Park EK, Hur YH, Koh YS, Kim HJ, Cho CK (2015) Volumetric analysis and indocyanine green retention rate at 15 min as predictors of post-hepatectomy liver failure. HPB 17(2):159–167. https://doi.org/10.1111/hpb.12295
Maruyama M, Yoshizako T, Araki H, Yoshida R, Ando S, Nakamura M, Kitagaki H (2018) Future liver remnant indocyanine green plasma clearance rate as a predictor of post-hepatectomy liver failure after portal vein embolization. Cardiovasc Intervent Radiol 41(12):1877–1884. https://doi.org/10.1007/s00270-018-2065-2
Hwang S, Ha TY, Song GW, Jung DH, Ahn CS, Moon DB, Kim KH, Lee YJ, Lee SG (2015) Quantified risk assessment for major hepatectomy via the indocyanine green clearance rate and liver volumetry combined with standard liver volume. J Gastrointest Surg 19(7):1305–1314. https://doi.org/10.1007/s11605-015-2846-8
Yada K, Morine Y, Ishibashi H, Mori H, Shimada M (2018) Treatment strategy for successful hepatic resection of icteric liver. J Med Investig 65(1.2):37–42. https://doi.org/10.2152/jmi.65.37
Vos JJ, Wietasch JK, Absalom AR, Hendriks HG, Scheeren TW (2014) Green light for liver function monitoring using indocyanine green? An overview of current clinical applications. Anaesthesia 69(12):1364–1376. https://doi.org/10.1111/anae.12755
Kokudo T, Hasegawa K, Amikura K, Uldry E, Shirata C, Yamaguchi T, Arita J, Kaneko J, Akamatsu N, Sakamoto Y, Takahashi A, Sakamoto H, Makuuchi M, Matsuyama Y, Demartines N, Malago M, Kokudo N, Halkic N (2016) Assessment of preoperative liver function in patients with hepatocellular carcinoma—the albumin-indocyanine green evaluation (ALICE) grade. PLoS ONE 11(7):e0159530. https://doi.org/10.1371/journal.pone.0159530
Russolillo N, Forchino F, Conci S, Mele C, Langella S, Ruzzenente A, Scoleri I, Giuliante F, Guglielmi A, Ferrero A (2019) Validation of the albumin-indocyanine green evaluation model in patients with resected hepatocellular carcinoma and comparison with the albumin-bilirubin score. J Hepato-Biliary-Pancreat Sci 26(1):51–57. https://doi.org/10.1002/jhbp.597
Miyazaki Y, Kokudo T, Amikura K, Takahashi A, Ohkohchi N, Sakamoto H (2019) Albumin-indocyanine green evaluation grading system predicts post-hepatectomy liver failure for biliary tract cancer. Dig Surg 36(1):13–19. https://doi.org/10.1159/000486142
Stockmann M, Lock JF, Riecke B, Heyne K, Martus P, Fricke M, Lehmann S, Niehues SM, Schwabe M, Lemke AJ, Neuhaus P (2009) Prediction of postoperative outcome after hepatectomy with a new bedside test for maximal liver function capacity. Ann Surg 250(1):119–125. https://doi.org/10.1097/SLA.0b013e3181ad85b5
Stockmann M, Lock JF, Malinowski M, Niehues SM, Seehofer D, Neuhaus P (2010) The LiMAx test: a new liver function test for predicting postoperative outcome in liver surgery. HPB 12(2):139–146. https://doi.org/10.1111/j.1477-2574.2009.00151.x
Lodewick TM, Alizai PH, van Dam RM, Roeth AAJ, Schmeding M, Heidenhain C, Andert A, Gassler N, Dejong CHC, Neumann UP (2017) Effect of age on liver function in patients undergoing partial hepatectomy. Dig Surg 34(3):233–240. https://doi.org/10.1159/000452494
Lock JF, Reinhold T, Malinowski M, Pratschke J, Neuhaus P, Stockmann M (2009) The costs of postoperative liver failure and the economic impact of liver function capacity after extended liver resection—a single-center experience. Langenbeck's Arch Surg 394(6):1047–1056. https://doi.org/10.1007/s00423-009-0518-4
Malinowski M, Lock JF, Seehofer D, Gebauer B, Schulz A, Demirel L, Bednarsch J, Stary V, Neuhaus P, Stockmann M (2016) Preliminary study on liver function changes after trisectionectomy with versus without prior portal vein embolization. Surg Today 46(9):1053–1061. https://doi.org/10.1007/s00595-015-1293-1
Morris-Stiff G, Gomez D, Prasad R (2009) Quantitative assessment of hepatic function and its relevance to the liver surgeon. J Gastrointest Surg 13(2):374–385. https://doi.org/10.1007/s11605-008-0564-1
Garcea G, Ong SL, Maddern GJ (2009) Predicting liver failure following major hepatectomy. Dig Liver Dis 41(11):798–806. https://doi.org/10.1016/j.dld.2009.01.015
Lorf T, Schnitzbauer AA, Schaefers SK, Scherer MN, Schlitt HJ, Oellerich M, Becker H, Obed A (2008) Prognostic value of the monoethylglycinexylidide (MEGX)-test prior to liver resection. Hepatogastroenterology 55(82–83):539–543
Wibmer A, Prusa AM, Nolz R, Gruenberger T, Schindl M, Ba-Ssalamah A (2013) Liver failure after major liver resection: risk assessment by using preoperative Gadoxetic acid-enhanced 3-T MR imaging. Radiology 269(3):777–786. https://doi.org/10.1148/radiol.13130210
Sato Y, Matsushima S, Inaba Y, Sano T, Yamaura H, Kato M, Shimizu Y, Senda Y, Ishiguchi T (2015) Preoperative estimation of future remnant liver function following portal vein embolization using relative enhancement on gadoxetic acid disodium-enhanced magnetic resonance imaging. Korean J Radiol 16(3):523–530. https://doi.org/10.3348/kjr.2015.16.3.523
Barth BK, Fischer MA, Kambakamba P, Lesurtel M, Reiner CS (2016) Liver-fat and liver-function indices derived from Gd-EOB-DTPA-enhanced liver MRI for prediction of future liver remnant growth after portal vein occlusion. Eur J Radiol 85(4):843–849. https://doi.org/10.1016/j.ejrad.2016.02.008
Asenbaum U, Kaczirek K, Ba-Ssalamah A, Ringl H, Schwarz C, Waneck F, Fitschek F, Loewe C, Nolz R (2018) Post-hepatectomy liver failure after major hepatic surgery: not only size matters. Eur Radiol 28(11):4748–4756. https://doi.org/10.1007/s00330-018-5487-y
Costa AF, Tremblay St-Germain A, Abdolell M, Smoot RL, Cleary S, Jhaveri KS (2017) Can contrast-enhanced MRI with gadoxetic acid predict liver failure and other complications after major hepatic resection? Clin Radiol 72(7):598–605. https://doi.org/10.1016/j.crad.2017.02.004
Cho SH, Kang UR, Kim JD, Han YS, Choi DL (2011) The value of gadoxetate disodium-enhanced MR imaging for predicting posthepatectomy liver failure after major hepatic resection: a preliminary study. Eur J Radiol 80(2):e195–200. https://doi.org/10.1016/j.ejrad.2011.08.008
Kim DK, Choi JI, Choi MH, Park MY, Lee YJ, Rha SE, Jung SE (2018) Prediction of posthepatectomy liver failure: MRI with hepatocyte-specific contrast agent versus indocyanine green clearance test. AJR Am J Roentgenol 211(3):580–587. https://doi.org/10.2214/AJR.17.19206
Yoon JH, Choi JI, Jeong YY, Schenk A, Chen L, Laue H, Kim SY, Lee JM (2016) Pre-treatment estimation of future remnant liver function using gadoxetic acid MRI in patients with HCC. J Hepatol 65(6):1155–1162. https://doi.org/10.1016/j.jhep.2016.07.024
Hwang EH, Taki J, Shuke N, Nakajima K, Kinuya S, Konishi S, Michigishi T, Aburano T, Tonami N (1999) Preoperative assessment of residual hepatic functional reserve using 99mTc-DTPA-galactosyl-human serum albumin dynamic SPECT. J Nucl Med 40(10):1644–1651
Tanoue Y, Nanashima A, Yano K, Fujii Y, Hiyoshi M, Imamura N, Hamada T, Ikenoue M, Wada T, Mizutani Y, Hirai T (2019) Significance of the preoperative regional maximal removal rate of technetium-99m-galactosyl human serum albumin in the future remnant liver: a sequential study of regional maximal removal rate of technetium-99m-galactosyl human serum albumin in the whole liver. Nucl Med Commun 40(2):145–152. https://doi.org/10.1097/MNM.0000000000000950
Nanashima A, Tobinaga S, Abo T, Nonaka T, Takeshita H, Hidaka S, Sawai T, Nagayasu T (2010) Reducing the incidence of post-hepatectomy hepatic complications by preoperatively applying parameters predictive of liver function. J Hepato-Biliary-Pancreat Sci 17(6):871–878. https://doi.org/10.1007/s00534-010-0281-5
Kaibori M, Ha-Kawa SK, Ishizaki M, Matsui K, Saito T, Kwon AH, Kamiyama Y (2008) HA/GSA-Rmax ratio as a predictor of postoperative liver failure. World J Surg 32(11):2410–2418. https://doi.org/10.1007/s00268-008-9725-3
Kokudo N, Vera DR, Tada K, Koizumi M, Seki M, Matsubara T, Ohta H, Yamaguchi T, Takahashi T, Nakajima T, Muto T (2002) Predictors of successful hepatic resection: prognostic usefulness of hepatic asialoglycoprotein receptor analysis. World J Surg 26(11):1342–1347. https://doi.org/10.1007/s00268-002-6262-3
Mizutani Y, Hirai T, Nagamachi S, Nanashima A, Yano K, Kondo K, Hiyoshi M, Imamura N, Terada T (2018) Prediction of posthepatectomy liver failure proposed by the international study group of liver surgery: residual liver function estimation with 99mTc-galactosyl human serum albumin scintigraphy. Clin Nucl Med 43(2):77–81. https://doi.org/10.1097/RLU.0000000000001913
Yoshida M, Shiraishi S, Sakamoto F, Beppu T, Utsunomiya D, Okabe H, Tomiguchi S, Baba H, Yamashita Y (2014) Assessment of hepatic functional regeneration after hepatectomy using (99m)Tc-GSA SPECT/CT fused imaging. Ann Nucl Med 28(8):780–788. https://doi.org/10.1007/s12149-014-0872-3
Mao Y, Du S, Ba J, Li F, Yang H, Lu X, Sang X, Li S, Che L, Tong J, Xu Y, Xu H, Zhao H, Chi T, Liu F, Du Y, Zhang X, Wang X, Dong J, Zhong S, Huang J, Yu Y, Wang J (2015) Using dynamic 99mT c-GSA SPECT/CT fusion images for hepatectomy planning and postoperative liver failure prediction. Ann Surg Oncol 22(4):1301–1307. https://doi.org/10.1245/s10434-014-4117-4
Hayashi H, Beppu T, Okabe H, Kuroki H, Nakagawa S, Imai K, Nitta H, Chikamoto A, Ishiko T, Baba H (2015) Functional assessment versus conventional volumetric assessment in the prediction of operative outcomes after major hepatectomy. Surgery 157(1):20–26. https://doi.org/10.1016/j.surg.2014.06.013
Tatsumi H, Masuda Y, Imaizumi H, Yoshida S, Goto K, Yama N, Mizuguchi T, Hirata K (2013) Asialoglycoprotein receptor scintigraphy with 99mTc-galactosyl human serum albumin (99mTc-GSA) as an early predictor of survival in acute liver failure. Anaesth Intensive Care 41(4):523–528. https://doi.org/10.1177/0310057X1304100414
Nanashima A, Abo T, Arai J, Matsumoto H, Kudo T, Nagayasu T (2013) Functional liver reserve parameters predictive for posthepatectomy complications. J Surg Res 185(1):127–135. https://doi.org/10.1016/j.jss.2013.05.021
Sumiyoshi T, Shima Y, Okabayashi T, Kozuki A, Hata Y, Noda Y, Kouno M, Miyagawa K, Tokorodani R, Saisaka Y, Tokumaru T, Nakamura T, Morita S (2016) Liver function assessment using 99mTc-GSA single-photon emission computed tomography (SPECT)/CT fusion imaging in hilar bile duct cancer: a retrospective study. Surgery 160(1):118–126. https://doi.org/10.1016/j.surg.2016.02.009
Okabayashi T, Shima Y, Morita S, Shimada Y, Sumiyoshi T, Sui K, Iwata J, Iiyama T (2017) Liver function assessment using technetium 99m-galactosyl single-photon emission computed tomography/CT fusion imaging: a prospective trial. J Am Coll Surg 225(6):789–797. https://doi.org/10.1016/j.jamcollsurg.2017.08.021
Sumiyoshi T, Okabayashi T, Negoro Y, Hata Y, Noda Y, Sui K, Iwata J, Matsumoto M (2018) (99m)Tc-GSA SPECT/CT fusion imaging for hepatectomy candidates with extremely deteriorated ICG value. Jpn J Radiol 36(9):537–543. https://doi.org/10.1007/s11604-018-0753-0
Yoshida M, Beppu T, Shiraishi S, Tsuda N, Sakamoto F, Kuramoto K, Okabe H, Nitta H, Imai K, Tomiguchi S, Baba H, Yamashita Y (2018) Liver function in areas of hepatic venous congestion after hepatectomy for liver cancer: (99m)Tc-GSA SPECT/CT fused imaging study. Anticancer Res 38(5):3089–3095. https://doi.org/10.21873/anticanres.12567
Nakamura I, Iimuro Y, Hai S, Kondo Y, Hatano E, Fujimoto J (2018) Impaired value of 99m Tc-GSA scintigraphy as an independent risk factor for posthepatectomy liver failure in patients with hepatocellular carcinoma. Eur Surg Res 59(1–2):12–22. https://doi.org/10.1159/000484044
Yumoto Y, Yagi T, Sato S, Nouso K, Kobayashi Y, Ohmoto M, Yumoto E, Nagaya I, Nakatsukasa H (2010) Preoperative estimation of remnant hepatic function using fusion images obtained by (99m)Tc-labelled galactosyl-human serum albumin liver scintigraphy and computed tomography. Br J Surg 97(6):934–944. https://doi.org/10.1002/bjs.7025
Chiba N, Yokozuka K, Ochiai S, Gunji T, Okihara M, Sano T, Tomita K, Tsutsui R, Kawachi S (2018) The diagnostic value of 99m-Tc GSA scintigraphy for liver function and remnant liver volume in hepatic surgery: a retrospective observational cohort study in 27 patients. Patient Saf Surg 12:15. https://doi.org/10.1186/s13037-018-0161-5
Nishiyama Y, Yamamoto Y, Hino I, Satoh K, Wakabayashi H, Ohkawa M (2003) 99mTc galactosyl human serum albumin liver dynamic SPET for pre-operative assessment of hepatectomy in relation to percutaneous transhepatic portal embolization. Nucl Med Commun 24(7):809–817. https://doi.org/10.1097/00006231-200307000-00011
Yano K, Nanashima A, Fujii Y, Hiyoshi M, Imamura N, Hamada T, Tsuchimochi Y, Wada T, Mizutani Y, Hirai T (2017) Preoperative regional maximal removal rate of technetium-99m-galactosyl human serum albumin is correlated with liver functional parameters, but did not predict postoperative morbidity. Nucl Med Commun 38(8):701–707. https://doi.org/10.1097/MNM.0000000000000702
Kwon AH, Ha-Kawa SK, Uetsuji S, Inoue T, Matsui Y, Kamiyama Y (1997) Preoperative determination of the surgical procedure for hepatectomy using technetium-99m-galactosyl human serum albumin (99mTc-GSA) liver scintigraphy. Hepatology 25(2):426–429. https://doi.org/10.1002/hep.510250228
Kwon AH, Matsui Y, Kaibori M, Ha-Kawa SK (2006) Preoperative regional maximal removal rate of technetium-99m-galactosyl human serum albumin (GSA-Rmax) is useful for judging the safety of hepatic resection. Surgery 140(3):379–386. https://doi.org/10.1016/j.surg.2006.02.011
Kobayashi K, Hattori N, Manabe O, Hirata K, Magota K, Shimamura T, Tamaki N (2015) Postoperative assessment of hepatic asialoglycoprotein receptor function with Tc-99m GSA: the safety margin of resection size in living donor liver transplantation. Ann Transplant 20:51–58. https://doi.org/10.12659/AOT.892490
Geisel D, Ludemann L, Froling V, Malinowski M, Stockmann M, Baron A, Gebauer B, Seehofer D, Prasad V, Denecke T (2015) Imaging-based evaluation of liver function: comparison of (9)(9)mTc-mebrofenin hepatobiliary scintigraphy and Gd-EOB-DTPA-enhanced MRI. Eur Radiol 25(5):1384–1391. https://doi.org/10.1007/s00330-014-3536-8
de Graaf W, van Lienden KP, Dinant S, Roelofs JJ, Busch OR, Gouma DJ, Bennink RJ, van Gulik TM (2010) Assessment of future remnant liver function using hepatobiliary scintigraphy in patients undergoing major liver resection. J Gastrointest Surg 14(2):369–378. https://doi.org/10.1007/s11605-009-1085-2
Rassam F, Olthof PB, Richardson H, van Gulik TM, Bennink RJ (2019) Practical guidelines for the use of technetium-99m mebrofenin hepatobiliary scintigraphy in the quantitative assessment of liver function. Nucl Med Commun 40(4):297–307. https://doi.org/10.1097/MNM.0000000000000973
Hoekstra LT, de Graaf W, Nibourg GA, Heger M, Bennink RJ, Stieger B, van Gulik TM (2013) Physiological and biochemical basis of clinical liver function tests: a review. Ann Surg 257(1):27–36. https://doi.org/10.1097/SLA.0b013e31825d5d47
Tomassini F, D'Asseler Y, Linecker M, Giglio MC, Castro-Benitez C, Truant S, Axelsson R, Olthof PB, Montalti R, Serenari M, Chapelle T, Lucidi V, Sparrelid E, Adam R, Van Gulik T, Pruvot FR, Clavien PA, Bruzzese D, Geboes K, Troisi RI (2020) Hepatobiliary scintigraphy and kinetic growth rate predict liver failure after ALPPS: a multi-institutional study. HPB. https://doi.org/10.1016/j.hpb.2020.01.010
Cieslak KP, Bennink RJ, de Graaf W, van Lienden KP, Besselink MG, Busch OR, Gouma DJ, van Gulik TM (2016) Measurement of liver function using hepatobiliary scintigraphy improves risk assessment in patients undergoing major liver resection. HPB 18(9):773–780. https://doi.org/10.1016/j.hpb.2016.06.006
Chapelle T, Op De Beeck B, Huyghe I, Francque S, Driessen A, Roeyen G, Ysebaert D, De Greef K (2016) Future remnant liver function estimated by combining liver volumetry on magnetic resonance imaging with total liver function on (99m)Tc-mebrofenin hepatobiliary scintigraphy: can this tool predict post-hepatectomy liver failure? HPB 18(6):494–503. https://doi.org/10.1016/j.hpb.2015.08.002
Chapelle T, Op de Beeck B, Roeyen G, Bracke B, Hartman V, De Greef K, Huyghe I, Van der Zijden T, Morrison S, Francque S, Ysebaert D (2017) Measuring future liver remnant function prior to hepatectomy may guide the indication for portal vein occlusion and avoid posthepatectomy liver failure: a prospective interventional study. HPB 19(2):108–117. https://doi.org/10.1016/j.hpb.2016.11.005
Olthof PB, Tomassini F, Huespe PE, Truant S, Pruvot FR, Troisi RI, Castro C, Schadde E, Axelsson R, Sparrelid E, Bennink RJ, Adam R, van Gulik TM, de Santibanes E (2017) Hepatobiliary scintigraphy to evaluate liver function in associating liver partition and portal vein ligation for staged hepatectomy: Liver volume overestimates liver function. Surgery 162(4):775–783. https://doi.org/10.1016/j.surg.2017.05.022
Sparrelid E, Jonas E, Tzortzakakis A, Dahlen U, Murquist G, Brismar T, Axelsson R, Isaksson B (2017) Dynamic evaluation of liver volume and function in associating liver partition and portal vein ligation for staged hepatectomy. J Gastrointest Surg 21(6):967–974. https://doi.org/10.1007/s11605-017-3389-y
Truant S, Baillet C, Deshorgue AC, El Amrani M, Huglo D, Pruvot FR (2017) Contribution of hepatobiliary scintigraphy in assessing ALPPS most suited timing. Updates Surg 69(3):411–419. https://doi.org/10.1007/s13304-017-0481-5
de Graaf W, van Lienden KP, van den Esschert JW, Bennink RJ, van Gulik TM (2011) Increase in future remnant liver function after preoperative portal vein embolization. Br J Surg 98(6):825–834. https://doi.org/10.1002/bjs.7456
Truant S, Baillet C, Fulbert M, Olivier A, Sergent G, Turpin A, Boleslawski E, El Amrani M, Huglo D, Pruvot FR (2019) Asymmetric kinetics of volume and function of the remnant liver after major hepatectomy as a key for postoperative outcome—a case-matched study. HPB. https://doi.org/10.1016/j.hpb.2019.10.008
Cieslak KP, Huisman F, Bais T, Bennink RJ, van Lienden KP, Verheij J, Besselink MG, Busch ORC, van Gulik TM (2017) Future remnant liver function as predictive factor for the hypertrophy response after portal vein embolization. Surgery 162(1):37–47. https://doi.org/10.1016/j.surg.2016.12.031
Serenari M, Pettinato C, Bonatti C, Zanoni L, Odaldi F, Cucchetti A, Ravaioli M, Fanti S, Pinna AD, Cescon M (2019) Hepatobiliary scintigraphy in the preoperative evaluation of potential living liver donors. Transpl Proc 51(1):167–170. https://doi.org/10.1016/j.transproceed.2018.04.087
Makuuchi M, Hasegawa H, Yamazaki S (1986) Indication for hepatectomy in patients with hepatocellular carcinoma and cirrhosis. Shindan Chiryo 74:1225–1230
Takasaki K (1986) Selection of operative procedure for primary hepatocellular carcinoma, complicated with live cirrhosis—criteria on control of volume in hepatic resection in consideration of security radicality and new deloped anatomically systemized hepatic resection. Jpn J Gastroenterol Surg 19:1881–1889
Narasaki H, Noji T, Wada H, Ebihara Y, Tsuchikawa T, Okamura K, Tanaka E, Shichinohe T, Hirano S (2017) Intraoperative real-time assessment of liver function with near-infrared fluorescence imaging. Eur Surg Res 58(5–6):235–245. https://doi.org/10.1159/000477347
Funding
The authors received no funding for this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing financial interest.
Research involving human participants and/or animals
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tomassini, F., Giglio, M.C., De Simone, G. et al. Hepatic function assessment to predict post-hepatectomy liver failure: what can we trust? A systematic review. Updates Surg 72, 925–938 (2020). https://doi.org/10.1007/s13304-020-00859-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-020-00859-7