Abstract
Introduction
Ready-to-use glucagon represents a significant advancement in the management of severe hypoglycemia for people with diabetes and their caregivers. This indirect treatment comparison (ITC) evaluated the efficacy and safety differences among the three ready-to-use glucagon treatments, Baqsimi® (nasal glucagon), Gvoke® (glucagon injection) and Zegalogue® (dasiglucagon injection), in adults and children with type 1 diabetes (T1D) or type 2 diabetes (T2D).
Methods
A systematic literature review was conducted to identify randomized clinical trials assessing the efficacy and safety of Baqsimi, Gvoke or Zegalogue versus reconstituted, injectable glucagon (IG) in reversing insulin-induced hypoglycemia. Bayesian fixed-effect network meta-analysis was used to perform the ITC. Study endpoints included proportion of participants achieving treatment success, maximum blood glucose achieved, time to achieve treatment success and maximum blood glucose and treatment-emergent adverse events (TEAE).
Results
Ten clinical trials were included in the ITC (four for Baqsimi, three for Gvoke, and three for Zegalogue). All three treatments achieved high proportions of treatment success (> 98%). In adults, the efficacy results from combined T1D and T2D analysis were consistent with the T1D analysis, except statistically significantly faster in achieving treatment success for Baqsimi vs Gvoke in the combined analysis (13.96 vs 14.66 min). The mean maximum blood glucose values were also statistically significantly lower for Baqsimi (168 mg/dl) vs Gvoke (220 mg/dl) and Zegalogue (190 mg/dl). There was a trend towards a lower number of adults experiencing ≥ 1 TEAE with Baqsimi compared to Gvoke or Zegalogue, but no statistical significance was reached.
Conclusion
Baqsimi, Gvoke and Zegalogue had comparable high proportions of treatment success in reversing insulin-induced hypoglycemia. Baqsimi achieved a lower mean maximum blood glucose value, which may have implications for the re-establishment of euglycemia. These findings may help support patients, caregivers and health care providers in their decision-making process when discussing various ready-to-use glucagon treatment options.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Why carry out this study? |
Ready-to-use glucagon represents a significant advancement in the management of severe hypoglycemia and has emerged as an alternative to the conventional injectable glucagon (IG) kit requiring reconstitution |
No head-to-head trials have been conducted to compare the efficacy and safety of three ready-to-use glucagons for the treatment of severe hypoglycemia |
This study aimed to compare the efficacy and safety of Baqsimi® (nasal glucagon), Gvoke® (glucagon injection) and Zegalogue® (dasiglucagon injection) versus conventional, reconstituted IG in reversing insulin-induced hypoglycemia using an indirect treatment comparison methodology |
What was learned from the study? |
In the absence of a head-to-head trial, this study enabled comparison of efficacy and safety of the three ready-to-use glucagon treatments, Baqsimi, Gvoke and Zegalogue, in which all three treatments demonstrated comparable high proportions of patients achieving treatment success and no significant differences in the incidence of TEAEs |
Current treatment guidelines recommend avoiding overtreatment of hypoglycemia to prevent rebound hyperglycemia. In this study, Baqsimi demonstrated a statistically significantly lower maximum blood glucose level compared to Gvoke and Zegalogue in adults, which may have implications for the re-establishment of euglycemia |
These findings may help support discussions among patients, caregivers and healthcare providers as they consider various ready-to-use glucagon treatment options |
Introduction
Severe hypoglycemia, a low blood glucose event characterized by altered mental or physical status requiring assistance for recovery, is a barrier to glycemic control, places a substantial burden on patients and caregivers and is a barrier to management for health care professionals. Severe hypoglycemia is common in clinical practice [1,2,3] and is associated with poorer outcomes, including mortality, cardiovascular disease and cognitive dysfunction [4,5,6]. Prompt administration of rescue therapy is necessary to prevent further cognitive impairment.
Prior to ready-to-use glucagon options becoming available, glucose ingestion and conventional, reconstituted injectable glucagon (IG) were the only options for the treatment of severe hypoglycemia. However, IG administration is prone to error and difficult for non-health care professionals to use successfully [7, 8]. Additionally, parents of children with type 1 diabetes (T1D) have anxiety and fear around glucagon administration [9]. Overall, reconstituted IG is underutilized in people with diabetes with only 1.2% of patients with type 1 or type 2 diabetes (T2D) having filled a prescription for reconstituted IG in 2014 based on claims data [10]. Furthermore, even experiencing a severe hypoglycemic event in the previous year only resulted in 3.5% and 8.1% of glucagon prescriptions being filled for patients with T1D or T2D, respectively [10].
Given the challenges and hesitancy around reconstituted IG use [7], there has been renewed interest in simpler glucagon options. Three ready-to-use glucagon treatment options that do not require reconstitution have recently become available: Baqsimi® [11] (Eli Lilly and Company), Gvoke® [12] (Xeris Pharmaceuticals) and Zegalogue® [13] (Novo Nordisk). Baqsimi is a nasally administered glucagon powder, Gvoke (glucagon injection) is available as a prefilled syringe or an autoinjector, and Zegalogue is a dasiglucagon (glucagon analogue) injection available as an autoinjector.
These ready-to-use glucagon options are important advancements in treatment of severe hypoglycemia for patients and their caregivers. However, no head-to-head studies comparing these next-generation treatments have been conducted. In the absence of any head-to-head comparisons, indirect methods can be used to evaluate interventions.
The aim of this study was to compare the efficacy and safety of the three newly developed, ready-to-use glucagon treatment options in reversing hypoglycemia in adults and children with T1D or T2D. Ultimately, this study may help inform the decision-making process between patients and their health care providers regarding glucagon treatment options.
Methods
Study Design
This was an indirect treatment comparison (ITC) of clinical trials comparing the efficacy and safety of Baqsimi (nasal glucagon), Gvoke (glucagon injection) or Zegalogue (dasiglucagon injection) versus conventional reconstituted IG in patients with T1D or T2D. A systematic literature review was conducted between November 29, 2021, and December 10, 2021. The studies identified in the systematic literature search were included in an indirect treatment comparison analysis. The study was registered at PROSPERO (CRD42022298569).
Systematic Literature Review
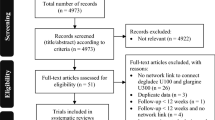
The systematic literature review was conducted using Embase, PubMed, clinicaltrials.gov and EudraCT. The search terms for the literature review are provided in Fig. 1. Any identified duplicate studies were removed from the search results. Two independent reviewers reviewed the titles and abstracts using the pre-defined inclusion and exclusion criteria provided below. Discrepancies were resolved by consensus or a third reviewer. For studies that met the inclusion criteria based on the abstract review, the full article was then reviewed for final inclusion and data extraction in the analysis.
Study Inclusion
Eligible studies were randomized controlled trials in people with diabetes experiencing hypoglycemia. Study participants were adults (≥ 18 years) or children (< 18 years) with T1D or T2D. Eligible studies compared Baqsimi, Gvoke or Zegalogue to reconstituted conventional IG and were published between January 1, 2000, and October 31, 2021, with an abstract written in English.
Studies were excluded if the participants did not have T1D or T2D, the examined glucagon doses were considered ‘micro,’ ‘mini’ or ‘low’ or only a placebo comparator was included.
Indirect Treatment Comparison Analysis
Eligible studies identified from the systematic literature search had data extracted by an independent reviewer. Due to differences in the methodology of the identified studies and to balance the adult populations between trials, only participants whose nadir blood glucose was ≤ 54 mg/dl were included in the analysis. No studies of children with T2D were identified. Therefore, three cohorts were analyzed: (1) adults with T1D, (2) adults with T1D or T2D (pooled) and (3) children with T1D.
Outcome Measures
The outcomes evaluated in this analysis were (1) proportion of participants achieving treatment success, (2) time to achieve treatment success, (3) incidence of treatment-emergent adverse events (TEAEs), (4) maximum blood glucose level and (5) time to reach maximum blood glucose level.
Treatment success was defined as an increase in blood glucose to ≥ 70 mg/dl or an increase of ≥ 20 mg/dl from nadir blood glucose within 30 min after glucagon administration. TEAEs were analyzed among patients experiencing at least one TEAE and patients experiencing headache, nausea and vomiting separately.
Statistical Analysis
Treatment comparisons were conducted among the three glucagon options (Baqsimi versus Gvoke, Baqsimi versus Zegalogue and Gvoke versus Zegalogue). Wald’s method was employed to analyze the difference in the proportion of treatment success at a significance level α of 5%, and the corresponding p value was used to assess the statistical significance of the observed difference. For the indirect treatment comparison, a Bayesian fixed-effect network meta-analysis was conducted for the analysis of maximum blood glucose, time to treatment success, time to maximum blood glucose and TEAEs, and inferences were drawn from the 95% credible intervals, which encompass zero (for differences) or one (for ratios).
Results
Systematic Literature Review Results
Ten trials were eligible and included in the indirect treatment analysis, including four for Baqsimi [14,15,16,17], three for Gvoke [18, 19] and three for Zegalogue [20,21,22] (Fig. 2). The variables explored in the ITC were not reported for every study; the availability of data for each glucagon option is shown in Table 1. Two studies, one Baqsimi and one Zegalogue study, were conducted in children with T1D, but no eligible studies of Gvoke were conducted in children with T1D. Baqsimi was the only ready-to-use glucagon treatment option that had data available from the T2D population. No head-to-head studies comparing these glucagon options were identified.
Efficacy Results
The reported data from eligible studies suggest that the rate of treatment success was > 98% for all three treatment options in all cohorts analyzed. Summary data for adults with T1D or T2D are shown in Figure S1. Using the indirect treatment comparison, no difference in the proportion of adults or children with diabetes achieving treatment success was observed in any cohort when adjusting for reconstituted IG (Table 2).
The time to treatment success was reported using mean values for Baqsimi and Gvoke trials and using median values for Zegalogue studies. Therefore, the difference in mean time to treatment success could only be compared between Baqsimi and Gvoke; analyses including Zegalogue could not be conducted because of these reporting differences. In the pooled population of adults with T1D or T2D, Baqsimi (13.96 min) had a significantly shorter mean time to achieve treatment success compared with Gvoke (14.66 min). The treatment difference was 1.45 min (95% credible interval [0.24, 2.68]) when adjusting for reconstituted IG (Table 2). In adults with T1D, Baqsimi also demonstrated a shorter time to achieve treatment success compared to Gvoke; however, the analysis did not reach statistical significance (treatment difference: 1.04 min, 95% credible interval [− 0.24, 2.34]).
Safety Results
Table 3 presents the summary of TEAEs from Baqsimi, Gvoke and Zegalogue. In adults with T1D, there was a trend towards a lower number of patients experiencing at least one TEAE with Baqsimi compared to Gvoke. However, no statistically significant differences were observed for any cohort (Gvoke vs Baqsimi: odds ratio, 1.40, 95% credible interval, [0.70, 2.52]); Zegalogue vs Baqsimi: 1.37, [0.42, 3.35]) when adjusting for reconstituted IG. Similarly, no statistically significant differences were observed when analyzing the incidence of nausea, vomiting or headache separately. Similar results were shown in adults with T1D or T2D. In children with T1D, there was also a trend towards a decreased number of patients experiencing at least one TEAE with Baqsimi compared to Zegalogue. No statistically significant differences were observed (Zegalogue vs Baqsimi: 1.43, [0.01, 8.02]). Due to the small sample size in the Zegalogue pediatric trial, the odds ratios for nausea, vomiting or headache, separately, are unstable with a wide credible interval. Therefore, no conclusions could be drawn from these data.
Pharmacodynamic Results
The mean maximum blood glucose values for the ready-to-use glucagon options and IG in adults T1D or T2D are shown in Figure S2. When adjusting for IG in the ITC, Baqsimi reached a significantly lower mean maximum blood glucose level compared to Gvoke (treatment difference: 17.32 mg/dl, 95% credible interval [3.94, 30.97]) or compared to Zegalogue (31.76 mg/dl [8.97, 55.60]) in adults with T1D or T2D (Table 4). Similar results were demonstrated for adults with T1D. No difference in the maximum blood glucose values between Zegalogue and Gvoke in adults with T1D was observed. The study conducted with Zegalogue in children with T1D did not report mean maximum blood glucose values.
The time to mean maximum blood glucose values in adults with T1D or T2D are shown in Figure S3. This analysis could not be conducted for Zegalogue versus Baqsimi or versus Gvoke because of the reporting differences (mean versus median) for the time endpoints. Baqsimi had a significantly shorter time to maximum blood glucose level than Gvoke in adults with T1D and in the pooled population of adults with T1D or T2D (Table 4). The treatment differences were 18.46 min (95% credible interval, [9.38, 27.79]) and 19.69 min, [10.72, 28.85], respectively.
Discussion
To our knowledge, this ITC is the first analysis comparing the next-generation ready-to-use glucagon treatments: Baqsimi, Gvoke and Zegalogue. In the absence of a head-to-head trial, this study enabled comparison of efficacy and safety of the glucagon treatments, Baqsimi, Gvoke and Zegalogue, and demonstrated similar efficacy in the treatment of severe hypoglycemia; all three ready-to-use glucagon treatments had success rates > 98% and no significant differences in the incidence of TEAEs. However, Baqsimi did achieve a statistically significantly lower maximum blood glucose level compared to both of the other two glucagon treatments. Additionally, in the pooled analysis, Baqsimi demonstrated a shorter time to achieve treatment success compared to Gvoke.
Current clinical treatment guidelines recommend avoiding overtreatment of hypoglycemia to prevent rebound hyperglycemia, which has the potential to impact cognitive function [23]. Therefore, an effective glucagon rescue treatment must rapidly raise the blood glucose level of a person experiencing severe hypoglycemia to an euglycemic level without resulting in sustained rebound hyperglycemia. A recent analysis of the clinical trial data comparing Baqsimi to reconstituted IG showed that the proportion of participants who experienced hyperglycemia (blood glucose value ≥ 180 mg/dl) after receiving Baqsimi was lower than in those who received IG in response to insulin-induced hypoglycemia [24, 25]. These data indicate that Baqsimi successfully treated the hypoglycemia without resulting in rebound hyperglycemia. Potentially, a lower maximum blood glucose level in response to glucagon treatment may contribute to a lower risk of rebound hyperglycemia and contribute to the safe re-establishment of euglycemia. Additionally, the individual clinical trials included in this ITC did not indicate any rebound hypoglycemia in patients with T1D or T2D.
In addition to the risk of rebound hyperglycemia and hypoglycemia and the time to treatment success, the time required to administer glucagon can play an important role in the overall success of glucagon treatment. Severe hypoglycemia is a life-threatening condition and needs to be treated as quickly and effectively as possible. In previous simulated use studies, the time to administer each ready-to-use glucagon treatment option was shorter when compared to reconstituted IG individually. Specifically, trained users successfully administered Baqsimi in a mean time of 47.3 s, while IG was successfully administered in 81.8 s [8]. Similarly, Gvoke autoinjector was administered in 47.9 s compared to IG in 109 s [26]. Finally, time to administer Zegalogue was 75 s versus 133 s for IG [27].
The efficacy and safety of the available glucagon options are essential factors for patients and healthcare providers to consider when making therapy decisions. To our knowledge, there are no studies directly comparing the preferences of patients for these ready-to-use glucagon options. A previous discrete choice experiment study conducted in Spain compared the attributes associated with Baqsimi to those associated with IG [28]. The results indicated that patients prefer a glucagon treatment with higher success rates, wider storage temperatures and a nasal delivery method when the efficacy of both treatments is similar [28]. However, the differences in availability and cost of these therapies between geographies and insurance programs must also be considered when making treatment decisions.
This study did have some limitations. First, the trials were not all designed or reported in a consistent manner. Therefore, not all variables, namely time variables, could be compared between all groups. Second, the total number of trials that met the inclusion criteria for this analysis was small. Also, the sample of adults with T2D was small and came from one Baqsimi trial. In fact, Baqsimi is the only glucagon option to include T2D in the identified trials. Third, baseline glucose values were not included in this analysis as not all included trials reported this parameter. However, the included trials did target at a baseline glucose value of < 55 mg/dl, and therefore it was reasonable to assume similar baseline glucose values between glucagon options. Finally, the analysis was not a direct comparison, and the results must be interpreted with caution.
While no head-to-head studies have been conducted, the use of an indirect treatment comparison technique provided a robust comparison between medications while adjusting for reconstituted IG. The consistent results demonstrated in this study for the adults with T1D and the pooled T1D and T2D diabetes population strengthened the confidence in the analysis. Moreover, the extensive literature search that was completed ensured the inclusion of all eligible studies. Specifically, including studies of adults with T1D or T2D and children with T1D from a global population allowed the generalization of the results for a broad population. Although the analysis was based on clinical trials conducted up to 2021, it remains current as no subsequent eligible studies meeting the inclusion criteria have been conducted after the study period, ensuring the validity and relevance of the findings within the current research landscape.
Conclusions
All the currently available ready-to-use glucagon treatments represent an important advancement in the treatment of severe hypoglycemia. This study demonstrated that Baqsimi, Gvoke and Zegalogue had comparable efficacy, but Baqsimi achieved a lower maximum blood glucose level and achieved treatment success in a shorter time. A glucagon rescue treatment that achieves treatment success quickly, does not put the patient at increased risk of rebound hyperglycemia and demonstrates an acceptable safety profile is important for patients and health care providers. These findings can support patients, caregivers and health care providers in their decision-making process for the treatment of severe hypoglycemia.
Data Availability
Data are available via corresponding author upon reasonable request.
References
Khunti K, Alsifri S, Aronson R, Cigrovski Berković M, Enters-Weijnen C, Forsén T, et al. Rates and predictors of hypoglycaemia in 27 585 people from 24 countries with insulin-treated type 1 and type 2 diabetes: the global HAT study. Diabetes Obes Metab. 2016;18(9):907–15. https://doi.org/10.1111/dom.12689.
Snoek FJ, Spaepen E, Nambu BA, Child CJ, Bajpai S, Balantac Z, et al. Conversations and reactions around severe hypoglycemia (CRASH) study: results from people with diabetes and caregivers in the United States. Clin Diabetes. 2022;40(4):477–88. https://doi.org/10.2337/cd21-0131.
ElSayed NA, Aleppo G, Aroda VR, Bannuru RR, Brown FM, Bruemmer D, et al. 6. Glycemic targets: standards of care in diabetes—2023. Diabetes Care. 2022;46(Supplement_1):S97–110. https://doi.org/10.2337/dc23-S006.
Yun JS, Ko SH. Risk factors and adverse outcomes of severe hypoglycemia in type 2 diabetes mellitus. Diabetes Metab J. 2016;40(6):423–32. https://doi.org/10.4093/dmj.2016.40.6.423.
Lacy ME, Gilsanz P, Eng C, Beeri MS, Karter AJ, Whitmer RA. Severe hypoglycemia and cognitive function in older adults with type 1 diabetes: the study of longevity in diabetes (SOLID). Diabetes Care. 2020;43(3):541–8. https://doi.org/10.2337/dc19-0906.
McCoy RG, Van Houten HK, Ziegenfuss JY, Shah ND, Wermers RA, Smith SA. Increased mortality of patients with diabetes reporting severe hypoglycemia. Diabetes Care. 2012;35(9):1897–901. https://doi.org/10.2337/dc11-2054.
Yale JF, Dulude H, Egeth M, Piché CA, Lafontaine M, Carballo D, et al. Faster use and fewer failures with needle-free nasal glucagon versus injectable glucagon in severe hypoglycemia rescue: a simulation study. Diabetes Technol Ther. 2017;19(7):423–32. https://doi.org/10.1089/dia.2016.0460.
Settles JA, Gerety GF, Spaepen E, Suico JG, Child CJ. Nasal glucagon delivery is more successful than injectable delivery: a simulated severe hypoglycemia rescue. Endocr Pract. 2020;26(4):407–15. https://doi.org/10.4158/ep-2019-0502.
Muradoğlu S, Yeşiltepe Mutlu G, Gökçe T, Can E, Hatun Ş. An evaluation of glucagon injection anxiety and its association with the fear of hypoglycemia among the parents of children with type 1 diabetes. J Clin Res Pediatr Endocrinol. 2021;13(3):285–92. https://doi.org/10.4274/jcrpe.galenos.2021.2020.0191.
Kahn PA, Liu S, McCoy R, Gabbay RA, Lipska K. Glucagon use by U.S. adults with type 1 and type 2 diabetes. J Diabetes Complications. 2021;35(5):107882. https://doi.org/10.1016/j.jdiacomp.2021.107882.
Baqsimi® (glucagon). U.S. Food and Drug Administration. https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/210134s000lbl.pdf. Accessed 26 Apr 2023.
Gvoke® (glucagon). U.S. Food and Drug Administration. https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/212097s000lbl.pdf. Accessed 26 Apr 2023.
Zegalogue® (dasiglucagon). U.S. Food and Drug Administration. https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/214231s000lbl.pdf. Accessed 26 Apr 2023.
Matsuhisa M, Takita Y, Nasu R, Nagai Y, Ohwaki K, Nagashima H. Nasal glucagon as a viable alternative for treating insulin-induced hypoglycaemia in Japanese patients with type 1 or type 2 diabetes: a phase 3 randomized crossover study. Diabetes Obes Metab. 2020;22(7):1167–75. https://doi.org/10.1111/dom.14019.
Sherr JL, Ruedy KJ, Foster NC, Piché CA, Dulude H, Rickels MR, et al. Glucagon nasal powder: a promising alternative to intramuscular glucagon in youth with type 1 diabetes. Diabetes Care. 2016;39(4):555–62. https://doi.org/10.2337/dc15-1606.
Suico JG, Hövelmann U, Zhang S, Shen T, Bergman B, Sherr J, et al. Glucagon administration by nasal and intramuscular routes in adults with type 1 diabetes during insulin-induced hypoglycaemia: a randomised, open-label, crossover study. Diabetes Ther. 2020;11(7):1591–603. https://doi.org/10.1007/s13300-020-00845-7.
Rickels MR, Ruedy KJ, Foster NC, Piché CA, Dulude H, Sherr JL, et al. Intranasal glucagon for treatment of insulin-induced hypoglycemia in adults with type 1 diabetes: a randomized crossover noninferiority study. Diabetes Care. 2016;39(2):264–70. https://doi.org/10.2337/dc15-1498.
Christiansen MP, Cummins M, Prestrelski S, Close NC, Nguyen A, Junaidi K. Comparison of a ready-to-use liquid glucagon injection administered by autoinjector to glucagon emergency kit for the symptomatic relief of severe hypoglycemia: two randomized crossover non-inferiority studies. BMJ Open Diabetes Res Care. 2021. https://doi.org/10.1136/bmjdrc-2021-002137.
Pieber TR, Aronson R, Christiansen MP, Bode B, Junaidi K, Conoscenti V. Efficacy, safety, tolerability, and noninferiority phase 3 study of glucagon as a ready-to-use room temperature liquid stable formulation versus a lyophilised formulation for the biochemical recovery and symptomatic relief of insulin-induced severe hypoglycaemia in adults with type 1 diabetes. Diabetes Obes Metab. 2022;24(7):1394–7.
Pieber TR, Aronson R, Hövelmann U, Willard J, Plum-Mörschel L, Knudsen KM, et al. Dasiglucagon-a next-generation glucagon analog for rapid and effective treatment of severe hypoglycemia: results of phase 3 randomized double-blind clinical trial. Diabetes Care. 2021;44(6):1361–7. https://doi.org/10.2337/dc20-2995.
Hövelmann U, Bysted BV, Mouritzen U, Macchi F, Lamers D, Kronshage B, et al. Pharmacokinetic and pharmacodynamic characteristics of dasiglucagon, a novel soluble and stable glucagon analog. Diabetes Care. 2018;41(3):531–7. https://doi.org/10.2337/dc17-1402.
Battelino T, Tehranchi R, Bailey T, Dovc K, Melgaard A, Yager Stone J, et al. Dasiglucagon, a next-generation ready-to-use glucagon analog, for treatment of severe hypoglycemia in children and adolescents with type 1 diabetes: results of a phase 3, randomized controlled trial. Pediatr Diabetes. 2021;22(5):734–41. https://doi.org/10.1111/pedi.13220.
Yale JF, Paty B, Senior PA. Hypoglycemia - 2018 clinical practice guidelines. Can J Diabetes. 2018;42(Suppl 1):S104–8. https://doi.org/10.1016/j.jcjd.2017.10.010.
Yan Y, Wang Q, Child CJ, Zhang MX. 1085-P: nasal glucagon was efficacious in reversing insulin-induced hypoglycemia without increasing risk of secondary hyperglycemia. Diabetes. 2020. https://doi.org/10.2337/db20-1085-P.
Giménez M, Yan Y, Wang Q, Child CJ, Zhang M. Nasal glucagon was efficacious in reversing insulin-induced hypoglycaemia without increasing risk of secondary hyperglycaemia. EASD Conference. 2020.
Valentine V, Newswanger B, Prestrelski S, Andre AD, Garibaldi M. Human factors usability and validation studies of a glucagon autoinjector in a simulated severe hypoglycemia rescue situation. Diabetes Technol Ther. 2019;21(9):522–30. https://doi.org/10.1089/dia.2019.0148.
Bailey NC, Dimsits J, Hammer M, Kendall DM, Bailey TS. A comparative study of dasiglucagon ready-to-use autoinjector and glucagon emergency kit during rescue from simulated severe hypoglycemia. Diabetes Technol Ther. 2022;24(4):231–40. https://doi.org/10.1089/dia.2021.0367.
Mitchell BD, Rentz AM, Kummer S, Yan Y, Heidenreich S, Krucien N, et al. People with diabetes and caregivers prefer rescue glucagon treatment with a wider storage temperature range and a nasal administration, when efficacy is similar: a discrete choice experiment in Spain. J Diabetes Sci Technol. 2022. https://doi.org/10.1177/19322968221095882.
Medical Writing, Editorial and Other Assistance
Eli Lilly funded medical writing, editorial and other analytical support for this article, which was provided by Vishali Vijayanagaram (analytical support), Levenia Baker (protocol development support and data collection support), Rebecca Threlkeld (protocol development support) and Mythili Ananth (writing and editorial support).
Funding
This research and Rapid Service and Open Access Fees were funded by Eli Lilly and Company, Indianapolis, IN.
Author information
Authors and Affiliations
Contributions
All authors were involved in the study design; Suresh Chenji, Kristen Syring, and Yu Yan were involved in data collection; Suresh Chenji conducted the statistical analysis; and all authors participated in the interpretation of study results, and in the drafting, critical revision, and approval of the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
Marga Giménez has received lecturing and consulting fees from Eli Lilly and Company, Medtronic Inc., Novo Nordisk, Sanofi-Aventis, and MSD. Munehide Matsuhisa has received honoraria from Eli Lilly Japan, Sanofi, Novo Nordisk Pharma, Abbott Japan, Sumitomo Pharma, Kyowa Kirin, Nippon Boehringer Ingelheim, and Orizuru Therapeutics; research funding from Novo Nordisk Pharma, Sysmex and Nissui. Kamlesh Khunti has acted as a consultant, speaker or received grants for investigator-initiated studies for Abbott, Amgen, AstraZeneca, Bayer, Boehringer Ingelheim, Eli Lilly, MSD, Napp, Novartis, Novo Nordisk, and Sanofi-Aventis. Suresh Chenji, Kristen Syring, and Yu Yan are employees and shareholders of Eli Lilly and Company.
Ethical Approval
This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Giménez, M., Khunti, K., Matsuhisa, M. et al. Systematic Literature Review and Indirect Treatment Comparison of Three Ready-to-Use Glucagon Treatments for Severe Hypoglycemia. Diabetes Ther 14, 1757–1769 (2023). https://doi.org/10.1007/s13300-023-01466-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-023-01466-6