Abstract
Introduction
This study aimed to examine the associations of hypoglycemia with health care resource utilization (HCRU) and health care costs among patients with type 2 diabetes mellitus (T2DM) in China.
Methods
This retrospective cohort study was conducted with 23,680 T2DM patients >18 years old who visited the Second Affiliated Hospital of Nanchang University between 1 January 2011 and 31 December 2015. Univariate descriptive statistics were used to relate the HCRU and associated costs to patient characteristics, and regression analysis was used to examine the association between hypoglycemia and HCRU, controlling for other confounding factors.
Results
In the T2DM patients with or without insulin treatment, when compared with nonhypoglycemic patients, hypoglycemia was associated with more medical visits (all T2DM patients 19.48 vs. 10.46, insulin users 23.45 vs. 14.12) and higher diabetes-related medical costs (all T2DM patients ¥5187.54 vs. ¥3525.00, insulin users ¥6948.84 vs. ¥3401.15) and medication costs (T2DM patients ¥1349.40 vs. ¥641.92, insulin users: ¥1363.87 vs. ¥853.96). Controlling for age, gender, and Charlson comorbidity index (CCI) score, hypoglycemia and insulin intake were associated with greater health care resource utilization. As compared to nonhypoglycemic patients, hypoglycemic T2DM patients and those on insulin therapy performed more outpatient visits (proportions of hypoglycemic vs nonhypoglycemic T2DM patients performing 3+ visits: 72.69% vs. 65.49%; proportions of hypoglycemic vs nonhypoglycemic patients on insulin therapy performing 3+ visits: 78.26% vs. 71.73%) and were hospitalized more often (proportions of hypoglycemic vs nonhypoglycemic T2DM patients with 3+ admissions 75.90% vs. 50.24%; proportions of hypoglycemic vs nonhypoglycemic patients on insulin therapy with 3+ admissions: 83.19% vs. 58.51%).
Conclusion
Hypoglycemia in diabetes patients was associated with increased healthcare resource utilization and health-related expenditure, especially for patients on insulin treatment. Insulin treatment regimens should be more individualized and account for hypoglycemia risk.
Similar content being viewed by others
Introduction
Diabetes is currently one of the biggest public health issues worldwide. The World Health Organization states that the prevalence of diabetes has risen continuously from a total of 108 million (4.7%) globally in 1980 to around four times that number (8.5%) in 2014. China, which has the world’s largest population and is undergoing sustained economic growth, is currently facing a serious diabetes epidemic: nearly 12% (114 million) of Chinese adults are diabetic (Dr. Margaret Chan at the 47th Meeting of the National Academy of Medicine, 2016). Adults living with diabetes suffer from a long-term economic burden and are at high risk of blindness, kidney failure, lower limb amputation, and several other long-term consequences that impact significantly on their quality of life [1].
Most (80–90%) cases of diabetes mellitus are of type 2 (T2DM), which is a progressive disease that affects glucose regulation [2, 3]. In recent years, the main goal of T2DM treatment has been to achieve good glycemic control [3] through a combination of diet, physical activity, and—if necessary—medication. Insulin therapy is an effective medication for achieving a common target of T2DM treatment: a glycated hemoglobin (HbA1c) level of below 7% [4, 5]. However, insulin therapy is a risk factor for iatrogenic hypoglycemia [6–9]. Diabetes-related hypoglycemia can cause complications such as pronounced effects on the cardiovascular (CV) system, atherosclerosis, patient depression, and even death [9–14]. Hypoglycemia can also significantly affect the quality of life of elderly patients due to their increased potential for dysrhythmias, accidents, falls, and neurological symptoms [15, 16]. All of these substantially influence healthcare utilization by and the burden of healthcare costs for diabetic patients [15, 17].
International studies have indicated that even though hypoglycemia prevalence varies markedly from country to country, the prevalence of hypoglycemia in each country is generally underestimated [17, 18]. In some recent Chinese studies it was found that the level of monitoring of glucose control outcomes varies among regions, but that the usage of insulin therapy is commonly high and is continuously increasing [19–22].
Given the increasing rate of hypoglycemia, the objective of this study of a subgroup of insulin users was to examine health care resource utilization (HCRU) by and health-related costs for Chinese T2DM patients with or without hypoglycemia.
Methods
Data Sources
This retrospective cohort study was conducted with 23,680 patients with type 2 diabetes who were selected from 1,477,727 patients who were over 18 years old and visited the Second Affiliated Hospital of Nanchang University (SAHNU) between 1 January 2011 and 31 December 2015. All of the patients in this study were required to be alive and to visit the SAHNU at least once a year during the 4-year period. At visits to the SAHNU, patients were required to provide venous blood after fasting for >8 h overnight. Serum was separated from the venous blood and stored at − 80 °C before inspection. The electronic medical records from the Second Affiliated Hospital of Nanchang University database were processed using the da Vinci S® system (provided by HEBTA, Pearland, TX, USA). The records included admission, diagnosis, medication, testing, surgical, nursing, and cost data as well as images, and the database contained all of the clinical data for the hospital. We calculated the HCRU associated with diabetes complications in both the hypoglycemic and nonhypoglycemic cohorts.
Variables
Type 2 diabetes mellitus was identified in this study based on the ICD-10 codes E11, E11.901, and E11.902. The date of first recorded T2DM diagnosis was defined as the index date. Pre-index-date patient information was used to derive baseline data on demographic and illness characteristics. Hypoglycemia after the index date was identified based on the ICD-10 codes E16.01, E16.001, E16.101, and E16.201, or a laboratory-measured glucose level of ≤ 3.9 mmol/L. Post-index-date diabetes-specific HCRU variables included number of medical visits and hospitalization. Post-index-date health care costs included medical costs and prescription drug costs.
Statistical Methods
Univariate descriptive statistics were used to describe the patient diabetes-specific HCRU and associated costs. Continuous data were reported as mean values and standard deviations (SD), and categorical data were reported as percentages. T2DM patients and patients on insulin therapy with or without hypoglycemia were compared in terms of the number of visits to a physician, the percentage of patients who performed 3+ outpatient visits, the percentage of patients who underwent 3+ hospitalizations, and associated medical costs.
Binary logistic regression analysis was used to estimate the likelihood of an outpatient visit and the likelihood of hospitalization in the diabetes patients, and then groups of patients were compared based on an independent variable: either age group (19–64 years old, 65–74 years old, or ≥ 75 years old), gender, Charlson comorbidity index (CCI) score (0–4, 5–10, or 11–14), hypoglycemic/nonhypoglycemic, and insulin use.
To further probe the relationship between HCRU and hypoglycemia, two multiple regression analyses controlling for baseline characteristics were conducted: a linear regression analysis of the number of outpatient visits and a Poisson regression analysis of number of hospitalizations. All statistical data were analyzed using the SPSS19.0 software package.
Compliance with Ethics Guidelines
This article is based on previously conducted studies of de-identified medical records and does not contain any studies with human participants or animals performed by any of the authors.
Results
Among 23,680 patients with type 2 diabetes mellitus, 3.29% reported hypoglycemia (54.87% male, mean age 69.02 years old). Among the insulin users (n = 8187), 4.21% suffered from hypoglycemia (57.39% male, mean age 69.11 years old) (Table 1). As shown in Table 2, the CCI scores for T2DM patients and for patients on insulin therapy were higher when the patients were hypoglycemic than when they were not (4.62 vs. 3.66 and 4.77 vs. 3.83).
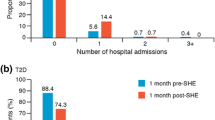
In T2DM patients, as compared with patients who did not report hypoglycemia, the patients with hypoglycemia had a higher number of medical visits (19.48 vs. 10.46) (Table 2), as well as higher diabetes-related medical costs (¥5187.54 per visit vs. ¥3525.00 per visit) and prescription drug costs (¥1349.40 per visit vs. ¥641.92 per visit). As shown in Table 2, among the patients who received insulin therapy, the patients with hypoglycemia had a higher number of medical visits (23.45 vs. 14.12). Among T2DM patients, the proportion with 3+ outpatient visits was 72.69% for the hypoglycemic group vs. 65.49% for the nonhypoglycemic group, while the corresponding proportions with 3+ hospitalizations were 75.90% and 50.24%, respectively. In a similar manner, among the patients taking insulin, the proportion with a mean number of outpatient visits of 3+ was 78.26% for hypoglycemic patients vs. 71.73% for nonhypoglycemic patients, while the corresponding proportions with 3+ admissions were 83.19% and 58.51%, respectively.
Table 3 shows effects of various patient characteristics on the likelihood of outpatient visits and hospital admissions. Compared with males, females had a lower risk of outpatient visits [OR 0.79 (0.73–0.84)] but a higher hospitalization risk [OR 1.15 (1.08–1.22)]. Patients aged 65–74 years and patients older than 74 years showed an increased frequency of hospitalization compared to those aged less than 65 years [OR 1.80 (1.64–1.98) and 2.73 (2.43–3.06), respectively]. Patients aged 65–74 years had a lower risk of outpatient visits than patients younger than 65 years old [OR 0.90 (0.82–0.98)] and patients older than 74 years [OR 0.82 (0.74–0.91)]. When the 65–74 year-old group was used as the reference, the risk for patients older than 74 was 1.51 times that for the reference group. Sicker T2DM patients had a higher hospitalization risk than healthier ones, as the OR for a CCI score of 5–10 vs. 0–4 was 3.03 (2.72–3.37) and the OR for a CCI score of 11–14 vs. 0–4 was 8.31 (2.63–26.28). The risk of outpatient visits [OR 1.50 (1.36–1.66)] or hospitalization [OR 6.40 (4.52–9.05)] was higher in hypoglycemic patients than in nonhypoglycemic patients. Patients on insulin were at a higher risk of walk-in visits than those who were not on insulin [OR 1.11 (1.04–1.18)].
Table 4 presents the results of multivariable linear regression analysis for outpatient visits and Poisson regression for hospitalization. CCI [regression coefficient: 4.37 (3.98–4.76)], hypoglycemia [regression coefficient: 19.07 (17.60–20.54)], and insulin use [regression coefficient: 5.52 (4.63–6.41)] were positively correlated with the number of outpatient visits. The number of hospitalizations was positively associated with gender, CCI, hypoglycemia, and insulin use [regression coefficients of 0.08 (0.05–0.12), 0.17 (0.15–0.19), 0.75 (0.70–0.79), and 0.17 (0.14–0.20), respectively]. Nevertheless, when the 19–64 year-old group was selected as the reference, the regression coefficient of the 65–74 year-old group was − 0.19 [− 0.22 to − 0.15] and that of the over 74 year-old group was 0.20 (0.16–0.23), meaning that the frequency of hospitalization was lowest in the 65–74 year-old group and highest in patients older than 74 years.
Discussion
To the best of our knowledge, our study is one of the first to use electronic medical records from a hospital to examine diabetes management in China. Hypoglycemia is commonly drug-induced in T2DM patients, while the most common cause of severe hypoglycemia is insufficient food intake [10]. Among the T2DM patients on insulin in our study, those who reported hypoglycemia performed more visits to the physician, were admitted to hospital more, and presented a greater economic burden (especially in terms of diabetes drugs) than those who did not report hypoglycemia. These findings are consistent with previous research showing that hypoglycemia significantly influences productivity and health care resource utilization and negatively affects patient quality of life [10, 17]. Studies show that patients who suffer from hypoglycemia tend to interrupt the therapy regimen (i.e., perform more medical visits) and are associated with higher diabetes-related costs [15, 23]. Among these costs, those associated with treating complications and drugs were the highest [24]. Whether or not the hypoglycemia is severe, the economic burden of a hypoglycemic patient is higher than that of a nonhypoglycemic patient [25–28].
In our study, we found that a confounder, age, influenced hospitalization frequency: older patients were at a higher risk of hospitalization than 19–64 year-old patients. Patients older than 74 years presented a lower frequency of hospitalization. However, this effect may relate to the association between age and the incidence of hypoglycemia and related complications. Elderly patients are more likely to develop complications of hypoglycemia due to decreasing physiological function [10]. The elderly are more prone to hypoglycemia than other age groups, but they also find it more difficult to spot their own symptoms of hypoglycemia [29, 30]. To avoid severe complications, the target blood glucose level among the elderly could be adjusted to give a moderate regimen with a target HbA1c level that is above 7% [31].
Self-monitoring and family support are important for T2DM patients, as they make it more likely that hypoglycemia will be identified promptly, and glycemic status could be monitored dynamically to ensure that blood glucose levels remain optimal [32, 33]. Adherence to the treatment regimen also influences the frequency of hypoglycemia, while adherence to diabetes treatment has generally been found to be poor [34, 35]. Efforts have been made to reduce the healthcare costs associated with hypoglycemia and to increase knowledge of hypoglycemia in patients and their families [36]. In addition to alleviating the hypoglycemia itself, hypoglycemic patients should be shifted to a more appropriate insulin therapy option in order to reduce side effects, improve the outcome, and to initially mitigate the burden on the patient [6, 37–41].
There are some limitations of this study. First, the retrospective design of the study meant that we could not pinpoint the causality in the relationship of T2DM-related hypoglycemia to HCRU and costs. Second, there may have been a selection bias, since we only obtained medical records from one hospital, and those records lacked data on discharge status and length of hospital stay, which are two important HCRU factors. Third, the hypoglycemia cases considered in this study were those of severe hypoglycemia, which requires medical attention. Cases of asymptomatic hypoglycemia were not included in the hypoglycemia group, meaning that the prevalence and therefore social cost of hypoglycemia may have been underestimated in this study. Lastly, this study is a single-institute study, so the results may not be representative of the Chinese health system nationally; our findings cannot therefore be generalized to primary health institutions or other areas in China.
Conclusion
Insulin use and hypoglycemia in T2DM patients are associated with an increased likelihood of medical visits as well as greater healthcare resource utilization by and health-related expenditure on the patient. To ease the disease burden on and the economic burden of the patient, the insulin treatment regimen needs to be individualized, taking into account the patient’s status.
References
World Health Organization. Global report on diabetes. Geneva: WHO; 2016.
Valentine V, Goldman J, Shubrook JH. Rationale for initiation and titration of the basal insulin/GLP-1RA fixed-ratio combination products, IDegLira and IGlarLixi, for the management of type 2 diabetes. Diabetes Ther. 2017;8:739–52.
Yu CG, Fu Y, Fang Y, Zhang N, Sun RX, Zhao D, Zhang BY, et al. Fighting type-2 diabetes: present and future perspectives. Curr Med Chem. 2017;24:1–17.
Xiong Z, Yuan L, Guo X, Lou Q, Zhao F, Shen L, Sun Z, et al. Rejection of insulin therapy among patients with type 2 diabetes in China: reasons and recommendations. Chin Med J. 2014;127:3530–6.
Wong J, Tabet E. The introduction of insulin in type 2 diabetes mellitus. Aust Fam Physician. 2015;44:278–83.
Wallia A, Molitch ME. Insulin therapy for type 2 diabetes mellitus. JAMA. 2014;311:2315–25.
Birkner K, Hudzik B, Gasior M. The impact of type 2 diabetes mellitus on prognosis in patients with non-ST elevation myocardial infarction. Pol J Cardio-Thorac Surg. 2017;14:127–32.
Herman ME, O’Keefe JH, Bell DSH, Schwartz SS. Insulin therapy increases cardiovascular risk in type 2 diabetes. Prog Cardiovasc Dis. 2017;60:422–34.
Hulkower RD, Pollack RM, Zonszein J. Understanding hypoglycemia in hospitalized patients. Diabetes Manag. 2014;4:165–76.
Kalra S, Mukherjee J, Ramachandran A, Saboo B, Shaikh S, Venkataraman S, Das A, et al. Hypoglycemia: the neglected complication. Indian J Endocrinol Metab. 2013;17:819.
Yang S-W, Park K-H, Zhou Y-J. The impact of hypoglycemia on the cardiovascular system: physiology and pathophysiology. Angiology. 2016;67:802–9.
Lee AK, Lee CJ, Huang ES, Sharrett AR, Coresh J, Selvin E. Risk factors for severe hypoglycemia in black and white adults with diabetes: the Atherosclerosis Risk in Communities (ARIC) Study. Diabetes Care. 2017;40:1661–7.
Brutsaert E, Carey M, Zonszein J. The clinical impact of inpatient hypoglycemia. J Diabetes Complicat. 2014;28:565–72.
Green AJ, Fox KM, Grandy S. Self-reported hypoglycemia and impact on quality of life and depression among adults with type 2 diabetes mellitus. Diabetes Res Clin Pract. 2012;96:313–8.
Dalal MR, Kazemi M, Ye F, Xie L. Hypoglycemia after initiation of basal insulin in patients with type 2 diabetes in the United States: implications for treatment discontinuation and healthcare costs and utilization. Adv Ther. 2017;34:2083–92.
Lopez JMS, Bailey RA, Rupnow MFT, Annunziata K. Characterization of type 2 diabetes mellitus burden by age and ethnic groups based on a nationwide survey. Clin Ther. 2014;36:494–506.
Emral R, Pathan F, Cortes CAY, El-Hefnawy MH, Goh S-Y, Gomez AM, Mirasol R, et al. Self-reported hypoglycemia in insulin-treated patients with diabetes: results from an international survey on 7289 patients from nine countries. Diabetes Res Clin Pract. 2017;134:17–28.
Polinski JM, Kim SC, Jiang D, Hassoun A, Shrank WH, Cos X, Curtis BH, et al. Geographic patterns in patient demographics and insulin use in 18 countries, a global perspective from the multinational observational study assessing insulin use: understanding the challenges associated with progression of therapy (MOSAIc). BMC Endocr Disord. 2015;15:46.
Dong C, Wang T, Zhou D, Wang Y, Wang L, Lv D. Investigation and analysis of hypoglycemic drugs treatment in inpatients with type 2 diabetes mellitus in our hospital. Chin Clin Pharmacol Ther. 2017;22:87–91.
Li R, Shi L, Yang Q, Wu Z, Ruan Y, Li Y, Qi J. Glycemic control and medication compliance of type 2 diabetes in community management system in Shanghai. J Environ Occup Med. 2016;33:329–33.
Wang W, Ruan D, Wang X, Wei J, Tian Y. An survey on hypoglycemic agents used among patients with type 2 diabetes in Beijing Huairou Hospital. Beijing Med J. 2017;39:87–91.
Li T, Ghang X, Li J, Wang X, Su X, Zhu L, Sun K. A three-year follow-up on patients with T2DM on drug therapy in Shihezi communities. J Pract Med. 2017;33:87–91.
Wu EQ, Zhou S, Yu A, Lu M, Sharma H, Gill J, Graf T. Outcomes associated with post-discharge insulin continuity in US patients with type 2 diabetes mellitus initiating insulin in the hospital. Hosp Pract. 1995;40(2012):40–8.
Scalone L, Cesana G, Furneri G, Ciampichini R, Beck-Peccoz P, Chiodini V, Mantovani LG, et al. Burden of diabetes mellitus estimated with a longitudinal population-based study using administrative databases. PloS One. 2014;9:e113741.
Liu J, Wang R, Ganz ML, Paprocki Y, Schneider D, Weatherall J. The burden of severe hypoglycemia in type 2 diabetes. Curr Med Res Opin. 2018:34:171–7.
Heller SR, Frier BM, Herslov ML, Gundgaard J, Gough SCL. Severe hypoglycaemia in adults with insulin-treated diabetes: impact on healthcare resources. Diabet Med. 2016;33:471–7.
Foos V, Varol N, Curtis BH, Boye KS, Grant D, Palmer JL, McEwan P. Economic impact of severe and non-severe hypoglycemia in patients with type 1 and type 2 diabetes in the United States. J Med Econ. 2015;18:420–32.
Williams SA, Shi L, Brenneman SK, Johnson JC, Wegner JC, Fonseca V. The burden of hypoglycemia on healthcare utilization, costs, and quality of life among type 2 diabetes mellitus patients. J Diabetes Complicat. 2012;26:399–406.
Kong APS, Chan JCN. Hypoglycemia and comorbidities in type 2 diabetes. Curr Diabetes Rep. 2015;15(10):80.
Bremer JP, Jauch-Chara K, Hallschmid M, Schmid S, Schultes B. Hypoglycemia unawareness in older compared with middle-aged patients with type 2 diabetes. Diabetes Care. 2009;32:1513–7.
Chen Y, Wang J, Wang L-J, Lin H, Huang P-J. Effect of different blood glucose intervention plans on elderly people with type 2 diabetes mellitus combined with dementia. Eur Rev Med Pharmacol Sci. 2017;21:2702–7.
Hirsch IB. Professional flash continuous glucose monitoring as a supplement to A1C in primary care. Postgrad Med 2017:129:781–90.
Ishikawa T, Koshizaka M, Maezawa Y, Takemoto M, Tokuyama Y, Saito T, Yokote K. Continuous glucose monitoring reveals hypoglycemia risk in elderly patients with type 2 diabetes mellitus. J Diabetes Investig. 2018;9:69–74.
Peyrot M, Barnett AH, Meneghini LF, Schumm-Draeger P-M. Insulin adherence behaviours and barriers in the multinational global attitudes of patients and physicians in insulin therapy study. Diabet Med. 2012;29:682–9.
Sambamoorthi U, Garg R, Deb A, Fan T, Boss A. Persistence with rapid-acting insulin and its association with A1C level and severe hypoglycemia among elderly patients with type 2 diabetes. Curr Med Res Opin. 2017;33:1309–16.
Peyrot M, Barnett AH, Meneghini LF, Schumm-Draeger P-M. Insulin adherence behaviours and barriers in the multinational Global Attitudes of Patients and Physicians in Insulin Therapy Study. Diabet Med. 2012;29:682–9.
Wit HM, Vervoort GMM, de Galan BE, de Tack CJ. A cost-controlling treatment strategy of adding liraglutide to insulin in type 2 diabetes. Neth J Med. 2017;75:272–80.
Lane WS, Weatherall J, Gundgaard J, Pollock RF. Insulin degludec versus insulin glargine U100 for patients with type 1 or type 2 diabetes in the US: a budget impact analysis with rebate tables. J Med Econ 2018:21:144–51.
Mu YM, Guo LX, Li L, Li YM, Xu XJ, Li QM, Pan CY. The efficacy and safety of insulin degludec versus insulin glargine in insulin-naive subjects with type 2 diabetes: results of a Chinese cohort from a multinational randomized controlled trial. Chin J Intern Med. 2017;56:660–6.
Min SH, Yoon JH, Hahn S, Cho YM. Efficacy and safety of combination therapy with an alpha-glucosidase inhibitor and a dipeptidyl peptidase-4 inhibitor in patients with type 2 diabetes mellitus: a systematic review with meta-analysis. J Diabet Investig. 2017. https://doi.org/10.1111/jdi.12754.
Zhao L, Sun T, Wang L. Chitosan oligosaccharide improves the therapeutic efficacy of sitagliptin for the therapy of Chinese elderly patients with type 2 diabetes mellitus. Ther Clin Risk Manag. 2017;13:739–50.
Acknowledgements
Funding
A grant from the Science and Technology Innovation Platform of the Jiangxi Provincial Science and Technology Department (20171BCD40024) helped to fund this study and the article processing charges, as did a grant from the General Project of the Jiangxi Provincial Science and Technology Department (2017BBH80025).
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published. The opinions of all authors are fully represented in the publication.
Author Contributions
Yingping Yi and Yawei Li contributed equally to this manuscript and designed and analyzed the study. Yawei Li and Anran Hou analyzed and explained features of the data. Yanqiu Ge, Yuan Xu, Gang Xiong, and Xinlei Yang collected the data and helped to analyze it. Stephanie Ann Acevedo helped with the proofreading and provided important suggestions regarding the layout of the paper. The corresponding authors Hua Xu and Lizheng Shi provided important suggestions about the design of the study and about how to refine the analysis of the data.
Disclosures
All of the named authors—Yingping Yi, Yawei Li, Anran Hou, Yanqiu Ge, Yuan Xu, Gang Xiong, Xinlei Yang, Stephanie Ann Acevedo, Lizheng Shi, and Hua Xu—certify that they have no financial or other conflicting interests regarding this work.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Data Availability
The datasets generated and/or analyzed during the current study are not publicly available due to the confidentiality provision of SAHNU, but are available from the corresponding author on reasonable request.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Enhanced content
To view enhanced content for this article go to https://doi.org/10.6084/m9.figshare.5972734.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Yi, Y., Li, Y., Hou, A. et al. A Retrospective Cohort Study of Patients with Type 2 Diabetes in China: Associations of Hypoglycemia with Health Care Resource Utilization and Associated Costs. Diabetes Ther 9, 1073–1082 (2018). https://doi.org/10.1007/s13300-018-0409-1
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-018-0409-1