Abstract
Introduction
The aim of this study was to assess the efficacy of co-administering sitagliptin to patients with inadequate glycemic control following treatment with metformin (MET), sulfonylurea (SU), or MET + SU.
Methods
A cohort of 25,386 patients with type 2 diabetes mellitus (hemoglobin A1c [HbA1C] >53 mmol/mol or 7%), newly treated with sitagliptin between 2007 and 2013, was sourced from UK general practices via The Health Improvement Network database. Among these, eligible patients were segregated into three groups: MET (n = 3364), SU (n = 509), or MET + SU therapy (n = 5929). The relative efficacy of sitagliptin added to SU or MET + SU compared with sitagliptin added to MET monotherapy was assessed with regards to HbA1c and body weight changes from baseline up to 52 weeks. The glycemic efficacy was a measure of average treatment effects obtained from multivariable linear regression models and propensity score-matching analysis.
Results
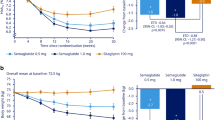
A total of 9802 patients were included in the study. Overall, addition of sitagliptin 100 mg once daily resulted in 5.5 mmol/mol (0.5%) HbA1c reduction (P < 0.001) and 0.8 kg weight reduction at 1 year (P < 0.001). Efficacy was similar across the treatment groups, but in patients with baseline HbA1c ≥9% adding sitagliptin to MET + SU produced a significantly smaller reduction in HbA1c when compared to the reference group MET (MET + SU vs. MET only: −0.5% vs. −0.7%, P < 0.001). The mean HbA1c reduction from baseline within this subgroup of patients was not significantly different between SU and MET monotherapies (−0.8% vs. −0.7%, respectively, P = 0.4). Across treatment groups, HbA1c reductions with add-on sitagliptin occurred after 24 weeks of treatment with a peak reduction occurring between 36 and 48 weeks, and receded after week 48.
Conclusion
In a real-world general practice setting, sitagliptin was effective in patients with suboptimal glycemic control with MET, SU or dual therapy, maximum between 36 and 48 weeks, but in patients with HbA1c of >9% receiving MET + SU therapy, adding sitagliptin, as a third agent, conferred minimal benefit.
Similar content being viewed by others
Introduction
The majority of patients with type 2 diabetes mellitus (T2DM) eventually require combination therapy to control hyperglycemia as their disease progress [1]. To this end, the use of combination therapies from different classes that have complementary mechanisms of action is recommended to facilitate more effective lowering of blood glucose levels [2]. The combination of metformin (MET) and sulfonylurea (SU) is the most widely used dual combination glucose-lowering therapy (GLT) in patients with T2DM [3]. However, combination therapy with these two agents may also not achieve or maintain glycemic control [4], necessitating the need for further treatment intensification. In this setting, use of injectable therapy such as insulin or glucagon-like peptide 1 (GLP-1) receptor agonist is often the next therapeutic step, although triple GLT (e.g., adding a thiazolidinedione to ongoing dual therapy with MET and a SU) is also used in clinical practice. However, many patients find the need for insulin injection or the adverse effects of edema and/or an increase in body weight with thiazolidinediones to be undesirable, which may adversely affect treatment compliance and glycemic response [5]. Hence, there is a need for additional options that can be added to MET and SU to avoid the need to switch to insulin. While randomized clinical trials (RCT) have examined the efficacy of various combination therapies, comparative efficacy data from routine real-world clinical practice could yield important and complimentary clinical information that needs be taken into account when determining treatment strategies [6].
Sitagliptin is a once-a-day orally active dipeptidyl peptidase-4 (DPP-4) inhibitor which has been administered to improve glycemic control in patients with T2DM treated as add-on therapy to MET or to SU monotherapy as well as add-on to MET-SU combination therapy [7–9]. Real-world studies on the comparative efficacy of the co-administration of sitagliptin with MET, SU, or dual MET and SU therapy have not been reported. This is relevant in view of the fact that, although both sitagliptin and SU stimulate insulin secretion from pancreatic β-cells [11, 12], sitagliptin, unlike SU, also lowers glucagon concentrations [10], which is likely to also contribute to the glucose lowering obtained with this agent. Although previous RCTs have shown that sitagliptin was effective when used as add-on combination treatment with MET and SU therapy [9], its efficacy in real-world practice has not been reported. Furthermore, within this setting, if sitagliptin is effective in combination with an SU then triple combination therapy with MET and an SU is likely to be effective as well.
The aim of the present work therefore is to report the glycemic response and treatment effect of sitagliptin when added to MET, SU, or MET + SU combination therapy in routine clinical practice. To address the influence of bias from confounders, the glycemic efficacy of sitagliptin co-administration was evaluated using multivariable linear regression and propensity score-matched analysis.
Methods
Study Design and Data Source
Retrospective cohort analyses were conducted of data from The Health Improvement Network (THIN) database, which contains anonymous patient data from more than 400 general practices throughout England and Wales [11]. This article is based on anonymous patient data and does not involve any new studies of human or animal subjects performed by any of the authors. Ethical approval was obtained as part of the Specialist Research committee approval by THIN, provided by the National Research Ethics Committee South East Research Ethics Committee.
Study Population
The study population comprised a cohort of patients identified to have T2DM and registered to a practice for more than 12 months before the index date (i.e., between January 1, 2006 and the end of the study on May 30, 2013). The cohort included patients who were ≥18 years old. This consisted of patients who had inadequate glycemic control (hemoglobin A1c [HbA1c] levels ≥53 mmol/mol (7%) after 6 months of MET monotherapy, SU monotherapy, or dual therapy consisting of both MET and SU. Patients who were concurrently taking other GLTs such as thiazolidinedione, GLP-1 agonist, sodium–glucose co-transporter-2 (SGLT-2) inhibitors, glinides, and acarbose were excluded from the study. In addition, patients with any records of insulin prescription and those taking sitagliptin as monotherapy or those taking another type of DPP-4 inhibitor were excluded. Concurrent lipid-lowering drugs, aspirin, and antihypertensive medications were allowed. Standardized computerized routines were used to identify and extract information on patient prescriptions for oral hypoglycemic agents using read codes to derive the cohort that was prescribed sitagliptin as an add-on therapy.
Exposure
Patients were administered an average of 100 mg/day of sitagliptin and the follow-up period commenced from the index date (the date of the first sitagliptin prescription) until a switch to or addition of another antidiabetic drug, or the 90th day post-index date when HbA1c level is recorded, or 52 weeks after the index date. Patients were segregated into the following treatment groups based on the oral antidiabetic treatments they received at baseline: MET monotherapy (Group A), SU monotherapy (Group B) and MET + SU (Group C). A parallel-group study involving the underlying treatment groups was set up with MET monotherapy group serving as the comparison or reference group.
Outcome
The primary efficacy outcome was change from baseline in HbA1c at 52 weeks. Secondary outcome was change from baseline in body weight. The glycemic efficacy of a treatment regimen is a measure of average treatment effect (ATE) exhibited by the treatment groups when compared with Group A, the reference group.
Covariates
Covariates were selected a priori on the basis of clinical significance. These are baseline demographic and medical parameters, and they include: age, gender, social deprivation (measured using Townsends index scores), body weight, body mass index (BMI), baseline HbA1c, total cholesterol levels, low-density lipoprotein (LDL), high-density lipoprotein (HDL), triglycerides, systolic and diastolic blood pressures, smoking status, duration of DPP-4 inhibitor therapy, the use of lipid-lowering drugs, antihypertensive drugs and aspirin, and comorbidities (e.g., coronary heart diseases, peripheral artery disease, cerebrovascular disease, hypoglycemia and heart failure). In addition, we used total duration of patients being treated with a GLT prior to adding sitagliptin, as a proxy of diabetes duration.
Statistical Analysis
Analysis on the primary efficacy of sitagliptin as an add-on therapy assessed the treatment groups for superiority with regard to the average HbA1c change from baseline at their respective endpoints. Multinomial propensity scores on the baseline covariates were estimated [12]. Balance in baseline covariates was assessed between the treatment groups using absolute standardized differences before and after propensity score weighting. A standardized effect size ≥20% indicated serious imbalance. The variations in mean and frequency distribution of measured baseline covariates between treatment groups with the same estimated propensity score were examined and summarized.
Propensity Score Model
Inverse probability of treatment weighting (IPTW) using the propensity score was employed to estimate the measures of effect. IPTW uses weights based on the propensity score to create a synthetic sample in which the distribution of measured baseline covariates is independent of treatment status [13, 14]. The method allowed us to estimate the ATE on the population, enabled us ascertain how glycemic efficacy would change if patients receiving SU + sitagliptin had been assigned to receive MET + SU before the addition of sitagliptin, relative to whether they had all received MET + sitagliptin (reference group). Propensity score was considered as a prognostic covariate and included in the multivariable linear regression model. Average changes in HbA1c were calculated and expressed as point estimates with 95% confidence interval (CI), at the conventional statistical significance level of 0.05. Missing data in the baseline covariates was accounted for with multiple imputations using chained equation (MICE) model [15]. All analyses were conducted using R [16] and Stata [17] packages.
Secondary and Subgroup Analyses
Baseline HbA1c was categorized into four strata: 7 to <7.5% (53–58 mmom/mol), ≥7.5 to <8% (58–64 mmol/mol), ≥8 to <9% (64–75 mmol/mol), and ≥9% (75 mmol/mol). Subgroup analysis for efficacy in endpoint changes from baseline in HbA1c was performed across the treatment groups. In addition, correlation and linear regression analysis were performed to assess the relationship between changes in HbA1c and changes in weight at 52 weeks in the study population.
Bias
Our analysis employed the “new user” design to minimize biases associated with prevalent use of sitagliptins [18]. Post-index date exposure to any GLT other than the treatment regimen under investigation was not permitted in our study to reduce confounding by indication. Patients were segregated into separate combination treatment groups to prevent confounding by co-medication. In addition, propensity score analysis was conducted to control for any confounding differences across treatment groups. The cohort was restricted to an estimated 52-week follow-up to reduce the risk of bias introduced by an overlapping treatment effect [18]. Sensitivity analysis was carried out to compare results of missing data with imputed data and to assess the reliability of the outcomes and the impact of missing data.
Results
General Patient Characteristics
Of the 25,386 users of DPP-4 inhibitor who were screened, 9802 (39%) patients fulfilled the criteria for cohort entry and were assigned to one of three treatment groups as outlined in Fig. 1. The number of patients assigned to each treatment group includes: 3364 (34%) on sitagliptin plus MET alone, 509 (5%) on sitagliptin plus SU alone, and 5929 (61%) on sitagliptin plus MET + SU regimen. The patients had a mean age of 62 years and were predominantly male (60%), obese (BMI >30 kg/m2, 62%), and on various antihypertensive medication (73%). The average follow-up time was 38 weeks and there was no significant difference in baseline demographic and metabolic characteristics of patients between the treatment groups (Table 1).
Efficacy
Overall, the co-administration of sitagliptin to patients who had inadequate glycemic control from ongoing MET, SU, and MET + SU regimen resulted in a significant 5.5 mmol/mol (0.5%) reduction in HbA1c (P < 0.001) and a 0.8 kg reduction in body weight (P < 0.001) (Table 2). The average HbA1c and weight reductions across the treatment groups were generally similar.
Propensity Score Model
The ATEs with regards to HbA1c reduction produced by the co-administration of sitagliptin with SU (treatment Group B) and with MET + SU (treatment Group C) did not show any change in HbA1c value (0.02% [0.2 mmol/mol], P = 0.7, and 0.03% [0.3 mmol/mol], P = 0.2, respectively; Table 2) However, when stratified according to levels of HbA1c at baseline, a significant difference in the treatment efficacy was observed in the subgroup of HbA1c ≥9% at baseline (Table 2). In this HbA1c subgroup, after adjusting for confounders which include duration of GLT prior to starting sitagliptin, glycemic efficacy was significantly greater among patients in Group A compared with their counterparts in Group C (−0.7% vs. −0.5%, respectively, P < 0.001; Fig. 2). The mean reduction from baseline in HbA1c was not significantly different between the treatment Group B and the reference Group A (−0.8% vs. −0.7%, P = 0.4; Table 2). Hence, adding sitagliptin to MET + SU dual therapy (Group C) did not confer additional glucose-lowering effects compared with co-administration of sitagliptin with MET nor SU monotherapies.
Overall, after adjusting for confounders, the co-administration of sitagliptin produced a glycemic effect that appeared to increase over time in both treatment and reference groups. However, this effect was not sustained throughout the study period, independent of all treatment groups (Fig. 3). HbA1c reduction was observed to take effect after 24 weeks of treatment with sitagliptin, with a peak reduction between week 36 and 48 and receded after week 48. Although adding sitagliptin to the reference Group A initially appears to produce a better onset of effect compared with treatment Group C (Fig. 3), our data show that the adjusted mean changes from baseline were not significantly different between the treatment and reference groups.
Other Analyses
The probability density functions of the propensity score matching of the respective treatment groups to reference group show there is no violation of the overlap assumption [19] (Fig. S1 in the supplementary material), A scatter plot of individual patient data also shows a negative, very weak and non-significant association between change in HbA1c and change in weight from baseline to endpoints. (Pearson’s correlation coefficient, r = −0.01; P = 0.3; Fig. 4) Therefore, the changes in HbA1c observed in the population do not account for the variation in weight change. The sensitivity analysis after multiple imputation showed similar results to our complete case models which indicate findings are unlikely attributable to bias from missing information (Table S1 in the supplementary material).
Discussion
Comparative effectiveness studies which examine the efficacy of the co-administration of sitagliptin to SU or MET + SU are not widely reported. Even where RCTs were carried out, the lack of rigorous patient inclusion and exclusion criteria such as what we have explored in this study may limit the generalizability of study findings. Overall, this study showed the addition of 100 mg/day of sitagliptin to patients with T2DM with inadequate glycemic control following MET monotherapy, SU monotherapy or both, resulted in a 5.5 mmol/mol (0.5%) reduction in HbA1c and a 0.8 kg weight loss at endpoint. The average HbA1c and weight reductions across the treatment groups were generally similar except within a subgroup of patients who had HbA1c ≥9% at baseline, where the co-administration of sitagliptin with MET + SU did not confer additional significant glucose lowering, even after adjusting for a proxy of diabetes duration. Thus, adding sitagliptin to SU confers equivalent benefit in Hba1c lowering compared with adding to MET, but the use of sitagliptin in combination with SU and MET therapy is not efficacious. Since the glycemic efficacy of sitagliptin co-administration was analyzed using multivariable linear regression, absolute comparison between treatment groups could not be performed.
Interestingly, the latter finding contradicts findings from a RCT, which showed additional HbA1c reduction with sitagliptin when added to MET plus glimepiride therapy [9]. This discrepancy may reflect the longer disease duration and diabetes progression, before patients in real-world practice are being offered a third-line therapy to manage their hyperglycemia. Based on the availabilities of other injectable therapies such as insulin or GLP-1 analog, we would question the merit of using sitagliptin to manage hyperglycemia as a triple oral therapy in routine practice. However, the observed equal benefit in HbA1c reduction when sitagliptin was added to patients who have failed SU therapy (compared with MET–sitagliptin combination therapy) implies an additional mechanism of action of sitagliptin therapy, above and beyond its ability to stimulate insulin secretion from an already exhausted pancreatic β-cells, such as GLP-1 and glucose-dependent insulinotropic peptide (GIP)-induced suppression glucagon secretion [10]. However, results obtained from previous systematic reviews and meta-analysis of RCTs studies compared sitagliptin + MET with MET alone reported that the dual therapy effectively improved HbA1c levels [20]. Similarly, evidence from recent studies [21, 22] have shown that, compared with MET monotherapy, DPP-4 inhibitor plus MET was associated with more reduction in HbA1c level [21]. The synergistic effect of sitagliptin with MET is increasingly well recognized and may be explained by the fact that MET enhances the expression and production of GLP-1 from the terminal ileum [23].
Another important and novel observation from this study relates to the durability of sitagliptin therapy. As a whole, across the treatment group, HbA1c reduction was observed to take effect after 24 weeks of treatment with sitagliptin, with a peak reduction between week 36 and 48 and receded after week 48. This is in contrast to most findings from RCT, where peak HbA1c reduction seemed to occur earlier, at approximately 6 weeks post-initiation of sitagliptin. However, most RCTs investigating the efficacy of DPP-4 inhibitors with SU or MET have reported outcomes for 24 weeks. However, one study using saxagliptin in combination with glyburide followed up patients for 76 weeks [24]. In this study, HbA1c reduction occurred immediately upon initiation of saxagliptin, peak reduction after 8–12 weeks, with a further rise in Hba1c thereafter, returning to baseline at 76 weeks, which may reflect the progressive nature of diabetes. However, in the two longest-running trials of DPP-4 inhibitors, the ‘escape phenomenon’, assessed by a secondary increase in HbA1c levels between weeks 24 and 104 following a good initial HbA1c reduction, was significantly less pronounced with sitagliptin 100 mg or vildagliptin 100 mg than with glipizide or glimepiride, respectively [25, 26], suggesting better β-cell protection and durability of glucose control with a DPP-4 inhibitor. A more recent 52-week RCT comparing sitagliptin versus canagliflozin when added to MET + SU showed maximum HbA1c reduction at 12 weeks and a progressive rise in Hba1c thereafter [27].
Our analyses were subjected to some limitations inherent to observational studies; our exposure data relate to prescriptions so we cannot be certain that the patients were completely compliant with their medication. However, should there be any overestimation of exposure to the medications in our analysis, such a misclassification would be non-differential and only bias results towards unity. Although we could not account for potential residual confounders such as compliance, diabetes duration, indications for different drug treatments, markers of β-cells deterioration and differences in dosages, we were able to account for differences in the observed covariates and used robust analytical techniques to control confounding that may bias the results of the estimated treatment effects. This included using a proxy for diabetes duration. In addition, HbA1c level at time of intensification (which is the same across treatment groups) and duration of therapy since starting MET were used as surrogate of diabetes duration, and included in the model for analysis.
Conclusions
In summary, the addition of sitagliptin to MET monotherapy, SU monotherapy, and MET + SU regimens in patients with inadequate glycemic control is a good therapeutic option for achieving efficacy in patients with T2DM. However, adding sitagliptin to an ongoing MET + SU regimen appears to be less efficacious among patients whose HbA1c is above 9% at the time of administration. We suggest that treatment should be characterized on an individual basis and robust RCTs are required to fully investigate the influence of obesity and longer treatment durations on the efficacy of co-administering sitagliptin to patients unresponsive to oral GLT.
References
Turner RC, Cull CA, Frighi V, Holman RR. Glycemic control with diet, sulfonylurea, metformin, or insulin in patients with type 2 diabetes mellitus: progressive requirement for multiple therapies (UKPDS 49). UK Prospective Diabetes Study (UKPDS) Group. JAMA. 1999;281(21):2005–12.
Cheruvallath ZS, Gwaltney SL 2nd, Sabat M, Tang M, Feng J, Wang H, et al. Design, synthesis and SAR of novel glucokinase activators. Bioorg Med Chem Lett. 2013;23(7):2166–71.
Riddle MC. Glycemic management of type 2 diabetes: an emerging strategy with oral agents, insulins, and combinations. Endocrinol Metab Clin N Am. 2005;34(1):77–98.
Owen V, Seetho I, Idris I. Predictors of responders to insulin therapy at 1 year among adults with type 2 diabetes. Diabetes Obes Metab. 2010;12(10):865–70.
Liebl A, Prager R, Binz K, Kaiser M, Bergenstal R, Gallwitz B, et al. Comparison of insulin analogue regimens in people with type 2 diabetes mellitus in the PREFER Study: a randomized controlled trial. Diabetes Obes Metab. 2009;11(1):45–52.
Ahren B, Mathieu C, Bader G, Schweizer A, Foley JE. Efficacy of vildagliptin versus sulfonylureas as add-on therapy to metformin: comparison of results from randomised controlled and observational studies. Diabetologia. 2014;57(7):1304–7.
Scheen AJ. DPP-4 inhibitors in the management of type 2 diabetes: a critical review of head-to-head trials. Diabetes Metab. 2012;38(2):89–101.
Charbonnel B, Karasik A, Liu J, Wu M, Meininger G. Efficacy and safety of the dipeptidyl peptidase-4 inhibitor sitagliptin added to ongoing metformin therapy in patients with type 2 diabetes inadequately controlled with metformin alone. Diabetes Care. 2006;29(12):2638–43.
Hermansen K, Kipnes M, Luo E, Fanurik D, Khatami H, Stein P. Efficacy and safety of the dipeptidyl peptidase-4 inhibitor, sitagliptin, in patients with type 2 diabetes mellitus inadequately controlled on glimepiride alone or on glimepiride and metformin. Diabetes Obes Metab. 2007;9(5):733–45.
Chen B, Moore A, Escobedo LV, Koletsky MS, Hou D, Koletsky RJ, et al. Sitagliptin lowers glucagon and improves glucose tolerance in prediabetic obese SHROB rats. Exp Biol Med (Maywood, NJ). 2011;236(3):309–14.
Lewis JD, Schinnar R, Bilker WB, Wang X, Strom BL. Validation studies of the health improvement network (THIN) database for pharmacoepidemiology research. Pharmacoepidemiol Drug Saf. 2007;16(4):393–401.
McCaffrey DF, Griffin BA, Almirall D, Slaughter ME, Ramchand R, Burgette LF. A tutorial on propensity score estimation for multiple treatments using generalized boosted models. Stat Med. 2013;32(19):3388–414.
Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res. 2011;46(3):399–424.
Rosenbaum PR. Model-based direct adjustment. J Am Stat Assoc. 1987;82(398):387–94.
White IR, Royston P, Wood AM. Multiple imputation using chained equations: Issues and guidance for practice. Stat Med. 2011;30(4):377–99.
R Core Team. R: a language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2013.
StataCorp. Stata Statistical Software. Release 13 ed. College Station: StataCorp LP; 2013.
Ray WA. Evaluating medication effects outside of clinical trials: new-user designs. Am J Epidemiol. 2003;158(9):915–20.
Busso M, DiNardo J, McCrary J. New evidence on the finite sample properties of propensity score reweighting and matching estimators. Rev Econ Stat. 2014;96:885–97.
Li J, Sun JZ, Li GS, Dai J. Effects of sitaglipin combined with metformin for type 2 diabetes mellitus: a systematic review. Chin J Evid Based Med. 2013;13(7):836–43.
Gao W, Dong J, Liu J, Li Y, Liu F, Yang L, et al. Efficacy and safety of initial combination of DPP-IV inhibitors and metformin versus metformin monotherapy in type 2 diabetes: a systematic review of randomized controlled trials. Diabetes Obes Metab. 2014;16(2):179–85.
Wu D, Li L, Liu C. Efficacy and safety of dipeptidyl peptidase-4 inhibitors and metformin as initial combination therapy and as monotherapy in patients with type 2 diabetes mellitus: a meta-analysis. Diabetes Obes Metab. 2014;16(1):30–7.
Kim M-H, Jee J-H, Park S, Lee M-S, Kim K-W, Lee MK. Metformin enhances glucagon-like peptide-1 via cooperation between insulin and Wnt signaling. J Endocrinol. 2013;14:2013.
Chacra AR, Tan GH, Ravichandran S, List J, Chen R, Investigators C. Safety and efficacy of saxagliptin in combination with submaximal sulphonylurea versus up-titrated sulphonylurea over 76 weeks. Diabetes Vasc Dis Res. 2011;8(2):150–9.
Seck T, Nauck M, Sheng D, Sunga S, Davies MJ, Stein PP, et al. Safety and efficacy of treatment with sitagliptin or glipizide in patients with type 2 diabetes inadequately controlled on metformin: a 2-year study. Int J Clin Pract. 2010;64(5):562–76.
Matthews DR, Dejager S, Ahren B, Fonseca V, Ferrannini E, Couturier A, et al. Vildagliptin add-on to metformin produces similar efficacy and reduced hypoglycaemic risk compared with glimepiride, with no weight gain: results from a 2-year study. Diabetes Obes Metab. 2010;12(9):780–9.
Schernthaner G, Gross JL, Rosenstock J, Guarisco M, Fu M, Yee J, et al. Canagliflozin compared with sitagliptin for patients with type 2 diabetes who do not have adequate glycemic control with metformin plus sulfonylurea: a 52-week randomized trial. Diabetes Care. 2013;36(9):2508–15.
Acknowledgments
No funding or sponsorship was received for this study or publication of this article. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval for the version to be published.
Conflict of interest
JM and RM have no relevant financial or other relationships to disclose. II has received research grants, speaker fees, and/or advisory board fees from Eli Lilly, MSD and Novo Nordisk. RD has received speaker fees and/or advisory board fees from Eli Lilly, MSD, Novo Nordisk, Jansen.
Compliance with ethics guidelines
This article is based on anonymous patient data and does not involve any new studies of human or animal subjects performed by any of the authors. Ethical approval was obtained as part of the Specialist Research committee approval by The Health Improvement Network, provided by the National Research Ethics Committee South East Research Ethics Committee.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0), which permits use, duplication, adaptation, distribution, and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Mamza, J., Mehta, R., Donnelly, R. et al. Comparative Efficacy of Adding Sitagliptin to Metformin, Sulfonylurea or Dual Therapy: A Propensity Score-Weighted Cohort Study. Diabetes Ther 6, 213–226 (2015). https://doi.org/10.1007/s13300-015-0110-6
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-015-0110-6