Abstract
Blood pressure variability has a great effect on the progression of arterial stiffness, which has increasingly become a hot research topic recently. In this study, beat-to-beat recordings of blood pressure (BP), heart rate, cardiac output, total peripheral resistance, and left ventricular ejection time during the cold pressor test (CPT) were analyzed together. We recruited 101 young Chinese subjects (aged 21–33) with no known history of high BP into the study. We found that the mean level of beat-to-beat BP and the average real variability and successive variation of beat-to-beat diastolic BP variability in the CPT showed significant correlations with pulse wave velocity (PWV) (r = 0.22–0.34, P < 0.05). In addition, we also found correlations between beat-to-beat heart rate and heart rate variability indices and PWV in each phase of the CPT. At the same time, the standard deviation of the R–R intervals and square root of the mean squared difference of successive R–R intervals in the cold stimulus phase also showed significant correlations with PWV (r = 0.23–0.24, P < 0.05). In conclusion, the level and variability of beat-to-beat BP have a strong influence on arterial stiffness.
Similar content being viewed by others
Introduction
The clinical value of blood pressure variability (BPV) has gained great attention during the past years. A large number of studies have suggested that variability of BP plays an important role in the assessment of end-organ damage independently of the traditional BP level, and the target organs have mainly been the heart, brain, and kidney in these studies [1–6]. Among them, artery alteration is a very important indicator because early lesions precede cardiovascular disease. A number of studies have examined the relationship between BPV and artery alterations [1, 6–8]. Asayama et al. found a significant relationship between arterial stiffness and home BPV in patients with pre-hypertension and hypertension [7]. Another study discovered that not only average 24-hour pulse pressure (PP) and systolic blood pressure (SBP) but also 24-hour BPV were associated with changes of large artery structure in hypertension [8]. Furthermore, Shintania et al. have shown that ambulatory BP values were more closely associated with carotid artery alteration than with casual BP in the general population [5]. García-García et al. found that 24-hour systolic blood pressure variability (SBPV) had a positive relationship with PWV and ambulatory arterial stiffness index (AASI) in hypertensive patients [9]. Stabile et al. reported that increased SBPV was closely associated with arterial stiffness in children and adolescents [10]. However, it is still controversial whether the mean level and variability of BP can be used as potential risk factors for arterial stiffness.
In these previous studies, most of the BPV parameters were captured from home BP or ambulatory BPV. Guido Grassi et al. discussed the relationships between cardiovascular risk factors and the increase in BPV, with sympathetic cardiovascular drive characterizing the high BP state [1]. Tatsuo Kawai et al. analyzed 143 consecutive patients performing renal Doppler ultrasonography and measured BP at outpatient visits six or more times [3]. In that study, they showed that visit-to-visit BPV correlated significantly with renal function and renal arteriosclerotic change [3]. Overall, in previous studies, most of the BPV parameters were captured from 24-hour ambulatory BP monitoring (ABPM) or from several BP measurements from home visits using clinical BPV. However, recently, beat-to-beat recordings of BP are recommended as the best means to capture short-term BPV, whereas intermittent ABPM is less precise [4]. Fang-Fei Wei et al. demonstrated that beat-to-beat SBPV expressed as variation independent of mean (VIM), maximum–minimum difference (MMD), or average real variability (ARV) was correlated with left ventricular mass index (LVMI), whereas beat-to-beat SBPV expressed as MMD was correlated with urinary albumin-to-creatinine ratio [6]. However, to the best of our knowledge, no previous studies have demonstrated a relationship between measures of beat-to-beat BPV and arterial stiffness.
The CPT, which measures changes of BP by immersing the hand into an ice water container, has been used to evaluate cardiovascular autonomic regulatory function [11]. Victor et al. thought that there were different effects on sympathetic outflow to the heart and to the skeletal muscles produced by the CPT [12] and that stimulation of sympathetic neural outflow to skeletal muscle was an important component of the sympathetic response to the CPT. Moreover, the arterial pressure response to the CPT can be used as a marker of muscle sympathetic activity. Lambert et al. reported that during the CPT, BP and the sympathetic nervous system (SNS) indicator increased significantly. and low-frequency (LF) power, high-frequency (HF) power, and the parasympathetic nervous system indicator declined significantly [13]. Lambert et al. also hypothesized that the surge in BP was associated with the degree of SNS response to the CPT [13]. The possible causes of this effect on hemodynamic and sympathetic responses are marked rises in BP, heart rate (HR), total peripheral resistance (TPR), plasma noradrenaline concentration, and muscle sympathetic burst frequency. Enrique et al. demonstrated differences of radioisotope uptake in a fragment between images acquired in the post-exercise phase and in the CPT [14]. The result showed significant differences of radioactive isotope absorption in a fragment between images acquired in the post-exercise phase and in the CPT. The author inferred that the explanation may be that the sympathetic nerve activation produced by the CPT gives rise to contraction of the coronary vessels, which leads to a decrease of coronary blood flow in the diseased coronary artery [14]. Nabel et al. showed that in normal coronary arteries, vasodilation is caused by sympathetic nerve activation produced by the CPT through several mechanisms [15]. The mechanisms possibly include the release of norepinephrine and epinephrine, the activation of β-adrenergic receptors and α2-adrenergic activity in the coronary vasculature, and an increase in average arterial pressure [15]. In contrast, the sympathetic nerve activation generated by the hardening of the coronary vessels during the CPT can play a role in constriction through the release of catecholamine and/or endothelial dysfunction [15]. Based on these studies, it was produced by endothelial dysfunction caused by atherosclerosis, which decreases the dilator function and increases the shrinkage reaction to sympathetic stimulation [16]. As previously described, the sympathetic and parasympathetic nerve counterbalance each other, and external cold stimulation could affect the balance. Simultaneously, the important role of the sympathetic nervous system in the CPT is to effect peripheral vasoconstriction.
Previous studies showed that PWV is a noninvasive parameter that is widely used to evaluate arterial stiffness [17, 18]. It is also easy to measure with high reproducibility in humans [19], and it has a strong correlation with cardiovascular events and all-cause mortality [20, 21]. Although aortic or carotid-femoral PWV is currently considered the gold standard for evaluating arterial stiffness, brachial-ankle PWV (baPWV) is widely prevalent in Asia. Studies have also proven the clinical value of baPWV in the cardiovascular disease field. For example, Takashima N et al. investigated the role of baPWV in predicting future cardiovascular disease events in the general Japanese population [22]. Noriko et al. recruited 3,960 middle-aged and elderly Japanese men, and after a mean of 8.2 years of follow-up, identified a variety of reasons for cardiovascular disease factors to lead to significantly increased mortality as PWV increased [18]. This study showed that an increased PWV can have important prognostic value for cardiovascular disease, especially in predicting mortality [18]. We chose to measure PWV to evaluate arterial stiffness for several reasons: first, because PWV reflects arterial wall elasticity, which is widely related to the aorta [23]; second, PWV can also reflect the hardening of arteries and endothelial damage; third, the PWV measurement method is widely considered to have high validity and be highly reproducible [24]. As a simple and quick method, PWV reflects the presence and severity of atherosclerosis, and this measurement is strongly associated with cardiovascular risk [25].
To the best of our knowledge, no previous studies have assessed the correlation between different indices of beat-to-beat BPV and arterial stiffness, which can indicate cardiovascular risk clearly. Therefore, the aim of this study was to analyze whether the different indices of beat-to-beat BPV are associated with arterial stiffness in healthy adults in different phases of the CPT, which is a standard test for evaluating cardiovascular autonomic regulation function [26, 27]. The arterial stiffness in this study was assessed by baPWV. We also investigated the influence of HRV indices on arterial stiffness. Pearson’s linear correlation coefficient was employed to measure the correlation of each BP and HR index to PWV in each phase of the CPT.
Methods
Study population
This study was ethically approved by the Shenzhen Institutes of Advanced Technology Institutional Review Board. We successfully recruited 101 young Chinese subjects with no family history of high blood pressure who were aged 21 to 33 years (25.2 ± 2.2). Among them, 85 were eligible for inclusion in the present analysis because they were in accordance with the experimental requirements through the experiment and provided all the required data. Risk factors, such as smoking and body mass index, were recorded. We excluded 16 subjects from the analysis due to having a large motion artifact during the CPT or to not following the study protocol.
Study design
In the experiment, subjects were brought to a quiet air-conditioned room in which the temperature was controlled at 20 °C. All the subjects were asked to lie on a bed for 13 min and to keep still and supine throughout the experimental procedure. The experiment was divided into three states, which were named baseline state (5 min), cold stimulus state (3 min) and post-baseline (5 min). In the second state, we asked the subject to immerse their left hand up to their wrist in cold stimulation produced by a mixture of ice and water and to maintain this state for 3 min. When measuring, we used a Form PWV/ABI® pulse pressure analyzer (BP-203RPEII, Omron Colin Co., Ltd., Tokyo, Japan) to measure baPWV. Moreover, the measurements were repeated twice. The first reading was as a calibration, but the value of the second measurement was recorded and used for more analysis. During the experiment, the cold stimulation was produced by a washbasin containing ice bags and water, and the temperature of the water (0 °C) was monitored by a thermometer.
BPV and HRV assessments
SBPV, diastolic blood pressure variability (DBPV), and HR variability (HRV) were examined using beat-to-beat SBP, diastolic blood pressure (DBP), and R–R interval (RRI) series (i.e., systolic BP-t, diastolic BP-t and RRI-t), respectively. Of those, RRI was defined as the time interval between two consecutive R-wave peaks of the ECG signal. In this study, it was calculated as 60 s divided by HR (beats/min). Beat-to-beat BP and HR were assessed by mean level and variability indices in the time-domain and in the frequency-domain. The BPV indices in the time-domain included standard deviation (SD), coefficient of variation (CV), ARV, and successive variation (SV) [4, 28, 29]. In addition, we also added prevalent parameters, which included VIM, residual standard deviation (RSD), MMD, and AASI [6, 30]. These parameters, such as VIM, RSD, and MMD, reflect the characteristics of BPV. The HRV indices in the time-domain included the standard deviation of the R–R intervals (SDNN), the coefficient of variation of RR intervals (CVrr), and the square root of the mean squared difference of successive R–R intervals (rMSSD) [31]. We calculated these indices using the equations listed in Table 1 [4, 26, 28, 32]. Then, the DC component was removed by subtracting the average value of the series. After that, fast Fourier transform was used to estimate the spectrum of the series at 256 window length. In the end, the BPV and HRV measures in frequency-domain were assessed as LF power (LF = 0.04–0.15 Hz), HF power (HF = 0.15–0.4 Hz), LF in normalized units (LFn), and HF in normalized units (HFn) [27, 31, 33, 34].
Statistical analysis
In this study, the baPWV was used for assessing the arterial stiffness, a parameter that reflects the target organ damage of the artery. The BP level and variability measures were first adjusted by age through BP measures/age for each subject. Then, the same was carried out for the HR measures. Afterwards, Pearson’s linear correlation coefficient was employed to measure the correlation of each BP and HR index to PWV in each phase of the CPT, respectively. And P < 0.05 was considered statistically significant. SPSS (Statistical Package for the Social Sciences) 19.0 statistical package (IBM Company, USA) was used for statistical analyses.
Results
The clinical characteristics of the study subjects are shown in Table 2. The subjects included 38 males (44.7 %) and 47 females (55.3 %). The prevalence of smoking, alcohol and coffee consumption was 0, 3.5 and 7.1 %, respectively. Nearly half of the subjects exercised regularly, and no one took medicine.
Table 3 shows cardiovascular measurements taken that can affect BP variability, which were cardiac output (CO), TPR, and left ventricular ejection time (LVET). In the condition of cold stimulation, levels of CO and TPR rose, while LVET fell. This phenomenon demonstrated that cold stimulation increased cardiac load and strengthened the force of cardiac contraction.
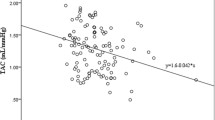
Table 4 shows the correlation between beat-to-beat BPV measures and PWV and the relation between the mean level of BP and PWV in each phase of the CPT. The results indicate that mean levels of BP were significantly correlated with PWV in all three phases (r = 0.26–0.34, P < 0.05). In addition, the ARV and the SV of DBPV in the cold stimulus phase also showed significant correlation with PWV (r = 0.22–0.25, P < 0.05). In addition, the scatter plots in Fig. 1 further confirm the linear correlation between the ARV and the SV of DBPV in the cold stimulus phase and PWV.
Table 5 presents the correlation between beat-to-beat HR measures and PWV in each phase of the CPT. The HF of HRV showed significant correlation with PWV in all three phases (r = 0.23–0.28, P < 0.05). The SDNN and rMSSD in the cold stimulus phase also showed significant correlation with PWV (r = 0.23–0.24, P < 0.05).
Discussion
Generally speaking, there is a close relationship between adverse cardiovascular events and increased average BP. However, an increasing number of recent studies have shown that the variability of BP level is another important cardiovascular complication related to hypertension status. Arterial stiffening can cause myocardial infarction, cognitive disorders, stroke, and kidney diseases, and it also can be taken for an independent predictor of cardiovascular outcome [35, 36].
In the present experiments, an important finding was that the ARV and SV of beat-to-beat DBPV in the cold stimulus phase showed significant correlations with PWV, indicating that both the mean level and variability of beat-to-beat BP have a strong influence on arterial stiffness in the pre-hypertension stage. It has been suggested that ARV is a more appropriate measure of variability and a more useful predictor of cardiovascular outcome [37]. ARV can also be usefully applied to visit-to-visit measurements. Therefore, ARV provides a computationally simple way of estimating variation about a trend. SV will be highly correlated with ARV, tending to be larger in absolute value and influenced to a greater extent by large discrepancies between successive measurements. These two parameters very accurately reflect the variability of DBP. DBP mainly reflects the magnitude of the peripheral resistance. High peripheral resistance is a major cause of high BP.
In our current study, PWV independently increased with the level, ARV and SV of beat-to-beat DBP. Because of the cross-sectional nature of our study, we cannot distinguish cause from effect. The observation demonstrates that aortic stiffening is closely associated with the progression of high BP in humans. Arterial stiffening plays a pivotal role in the progression of high BP and the development of cardiovascular diseases. Arterial stiffness is a consequence of arteriosclerosis, which results from long-term cumulative damage from risk factors in the artery [19]. Indeed, arterial stiffness has always been regarded as a complication of hypertension that is a long-term outcome of the combined action of elevated BP and other risk factors. Because high BP will lead to arterial stiffness and vice versa, hardened arteries will increase BP, resulting in the high correlation between BP and arterial stiffness. With the passage of time, large arteries become increasingly thicker and lose their elasticity, which leads to an increase in PWV, the gold standard measure of arterial stiffness. Hardening of the arteries weakens the pumping and buffering function of the arteries and increases PWV by increasing SBP and PP. In a longitudinal cohort study, Bernhard et al. showed that the degree of arteriosclerosis and vascular lumen enlargement increase the likelihood of developing high BP [38]. However, that is not to say that the initial BP value is independently related to the risk of atherosclerosis [38]. Therefore, the hardening of the arteries can predict effects on increased SBP and high BP events [38].
Several studies have been conducted with the aim of disentangling the precise contribution of humoral, neural, and environmental factors to BPV [39–41]. In previous studies, Fang-Fei Wei et al. reported that beat-to-beat BPV was used to evaluate target organ damage [6]. This study mainly explained that short BPV, such as beat-to-beat recordings, even as short as 10 min, was associated with LVMI independent of level. In another study, they found a positive correlation between systolic and diastolic BPV and PWV in hypertensive patients [42]. During the experiment, they measured 24-hour BPV using SD and CV. Similarly, we come to the conclusion that the ARV and SV of DBPV in the CPT are also related to PWV (r = 0.22–0.25, P < 0.05).
The above findings have shown that these factors are interacting and thus are inseparable. There may be theoretical scientific significance to distinguishing them, but there is no significance in clinical practice. To a large degree, BPV in beat-to-beat and 24-hour ABPM reflect central and autonomic nervous regulation (increased central sympathetic nervous regulation and decreased arterial reactions and cardiopulmonary reflexes) [40], arterial elasticity (reduced arterial wall compliance) [43, 44], humoral effects (angiotensin II, insulin, nitric oxide), hemodynamics (blood viscosity), a variety of psychological emotional factors and duration. Why does DBP show such responses to the CPT while systolic pressure does not? The explanation for this phenomenon may be aging. A few previous studies have reported that aging is an important factor that influences BP responses to the CPT, particularly showing greater BP responses in elderly patients [45, 46]. For example, Mingzhi Zhang et al. reported that SBP responses to the CPT were greater in elderly patients, whereas DBP responses were greater in young patients [11]. Hess et al. came to similar conclusions that DBP responses to the CPT show the same trend with aging [46]. With increasing age, there is a reverse change from DBP responses produced by the CPT pattern to more SBP responses [45].
It appears to be widely assumed that central atherosclerosis partially explains this mechanism of potentially greater variability in SBP, but not DBP, responses to the CPT in older subjects. Throughout the cardiac cycle, the buffer effect of blood vessels can be thickened due to systemic structural changes in the arteries with age, which leads to increased SBP and potentially increased pulse pressure in response to the CPT [11]. In addition, Giuseppe et al. considered that short-term SBP variability measured by 24-hour ABPM and atherosclerosis in high BP patients showed an independent but moderate correlation, especially the parameters of short-term BPV (ARV and weighted 24-hour SD) [39]. In that study, the average age was 40 years or older, whereas our study population was relatively young, healthy subjects with no foundation disease. The different age structures in the two experiments led to different conclusions. One possible explanation is that with the increase of age, the degree of large artery hardening increased and elasticity decreased, which led to changes in SBP being greater than DBP in the whole CPT.
Ageing is a process that causes structural and functional modifications in the vasculature, resulting in decreased arterial compliance and increased arterial stiffness. Previous findings have suggested that increased 24-hour BPV is associated with an elevated risk of target organ damage [1, 2], early atherosclerosis [38] and cardiovascular events [25]. However, we do not fully understand the reasons for the changes of BPV. Inflammatory factors causing vasoconstriction and promoting acute BP increases may play a role in the increase of BPV [47, 48]. Therefore, our results are consistent with these findings. That is to say, the potential arterial stiffness being induced by cold stimulation leads to the increase of BPV. In other words, it may be useful to assess arterial stiffness by measuring different parameters of BPV. Consequently, we hope that this method of evaluating beat-to-beat BPV is more accessible at the clinic.
Moreover, the HF region of the HRV spectrum, SDNN, and rMSSD all showed significant correlations with PWV, also indicating that HRV potentially influences arterial stiffness [49]. Increased resting HR is an independent risk factor for arterial stiffness that is positively associated with cardiovascular disease [50]. Excessive sympathetic nerve action contributes to the variability of HR, which may increase arterial stiffness by increasing the shear stress on the arterial wall. Greater HRV may increase pressure on the wall and increase artery shear stress in the shorter diastolic. Thus, the growth of smooth muscle cells and collagen deposition possibly further accelerates the pace of arterial wall stiffening [51].
Although our study obtained some findings, there were some limitations. First of all, the relatively small sample size of our study is a major limitation, although our results and those of previous studies are complementary to each other. Second, we can improve choosing the characteristics of the study subjects, whether guaranteeing single factor analysis or characteristics of the sample itself. Therefore, further analysis is required to study these effects in greater detail. Third, the relative contributions of increased aortic stiffness and increased short-term BPV (beat-to-beat BPV) to cardiovascular complications in hypertension also require a better understanding.
Conclusions
In this study, we provide evidence that some of the indices of beat-to-beat BPV show significant correlations with PWV in the CPT. Specifically, the ARV and SV of DBPV in the cold stimulus phase were found to be related to PWV (r = 0.22–0.25, P < 0.05). In addition, we found correlations between some of the indices of HRV and PWV in all three phases of the CPT. Specifically, the HF of HRV showed a significant correlation with PWV for all the values of the three phases (r = 0.23–0.28, P < 0.05). The SDNN and rMSSD in the cold stimulus phase also showed significant correlations with PWV (r = 0.23–0.24, P < 0.05). However, in the future, more research should be conducted to prove the worth of different indices of beat-to-beat BPV in clinical applications.
References
Grassi G, Bombelli M, Brambilla G, Trevano FQ, Dell’oro R, Mancia G (2012) Total cardiovascular risk, blood pressure variability and adrenergic overdrive in hypertension: evidence, mechanisms and clinical implications. Curr Hypertens Rep 14(4):333–338. doi:10.1007/s11906-012-0273-8
Green P, Woglom AE, Genereux P, Daneault B, Paradis JM, Schnell S, Hawkey M, Maurer MS, Kirtane AJ, Kodali S, Moses JW, Leon MB, Smith CR, Williams M (2012) The impact of frailty status on survival after transcatheter aortic valve replacement in older adults with severe aortic stenosis: a single-center experience. JACC Cardiovasc Interv 5(9):974–981. doi:10.1016/j.jcin.2012.06.011
Kawai T, Ohishi M, Kamide K, Onishi M, Takeya Y, Tatara Y, Oguro R, Yamamoto K, Sugimoto K, Rakugi H (2012) The impact of visit-to-visit variability in blood pressure on renal function. Hypertens Res 35(2):239–243. doi:10.1038/hr.2011.170
Dolan E, O’Brien E (2010) Blood pressure variability: clarity for clinical practice. Hypertension 56(2):179–181. doi:10.1161/HYPERTENSIONAHA.110.154708
Shintani Y, Kikuya M, Hara A, Ohkubo T, Metoki H, Asayama K, Inoue R, Obara T, Aono Y, Hashimoto T, Hashimoto J, Totsune K, Hoshi H, Satoh H, Imai Y (2007) Ambulatory blood pressure, blood pressure variability and the prevalence of carotid artery alteration: the Ohasama study. J Hypertens 25(8):1704–1710. doi:10.1097/HJH.0b013e328172dc2e
Wei F-F, Li Y, Zhang L, Xu T-Y, Ding F-H, Wang J-G, Staessen JA (2014) Beat-to-beat, reading-to-reading, and day-to-day blood pressure variability in relation to organ damage in untreated Chinese. Hypertension 63(4):790–796. doi:10.1161/HYPERTENSIONAHA.113.02681
Asayama K, Kikuya M, Schutte R, Thijs L, Hosaka M, Satoh M, Hara A, Obara T, Inoue R, Metoki H, Hirose T, Ohkubo T, Staessen JA, Imai Y (2013) Home blood pressure variability as cardiovascular risk factor in the population of Ohasama. Hypertension 61(1):61–69. doi:10.1161/HYPERTENSIONAHA.111.00138
Mancia G, Parati G, Hennig M, Flatau B, Omboni S, Glavina F, Costa B, Scherz R, Bond G, Zanchetti A (2001) Relation between blood pressure variability and carotid artery damage in hypertension: baseline data from the European lacidipine study on atherosclerosis (ELSA). J Hypertens 19(11):1981–1989. doi:10.1097/00004872-200111000-00008
Xiong H, Wu D, Tian X, Lin WH, Li C, Zhang H, Cai Y, Zhang YT (2014) The relationship between the 24 h blood pressure variability and carotid intima-media thickness: a compared study. Comput Math Methods Med 2014:303159. doi:10.1155/2014/303159
Stabouli S, Papakatsika S, Kotronis G, Papadopoulou-Legbelou K, Rizos Z, Kotsis V (2015) Arterial stiffness and SBP variability in children and adolescents. J Hypertens 33(1):88–95. doi:10.1097/hjh.0000000000000369
Zhang M, Zhao Q, Mills KT, Chen J, Li J, Cao J, Gu D, He J (2013) Factors associated with blood pressure response to the cold pressor test: the GenSalt study. Am J Hypertens 26(9):1132–1139. doi:10.1093/ajh/hpt075
Victor RG, Leimbach WN, Seals DR, Wallin BG, Mark AL (1987) Effects of the cold pressor test on muscle sympathetic nerve activity in humans. Hypertension 9(5):429–436. doi:10.1161/01.hyp.9.5.429
Lambert EA, Chatzivlastou K, Schlaich M, Lambert G, Head GA (2014) Morning surge in blood pressure is associated with reactivity of the sympathetic nervous system. Am J Hypertens 27(6):783–792. doi:10.1093/ajh/hpt273
Pautasso E, Koretzky M, Marcon L, Borrego C, Panini J, Lerman J (2014) Can the cold pressor test predict future cardiovascular events in patients without demonstrated ischemic heart disease by SPECT? Int J Cardiol 175(2):226–232. doi:10.1016/j.ijcard.2014.04.202
Nabel EG, Ganz P, Gordon JB, Alexander RW, Selwyn AP (1988) Dilation of normal and constriction of atherosclerotic coronary arteries caused by the cold pressor test. Circulation 77(1):43–52. doi:10.1161/01.cir.77.1.43
Zeiher AM, Drexler H, Wollschlaeger H, Saurbier B, Just H (1989) Coronary vasomotion in response to sympathetic stimulation in humans: importance of the functional integrity of the endothelium. J Am Coll Cardiol 14(5):1181–1190. doi:10.1016/0735-1097(89)90414-2
Kazūne S, Grabovskis A, Strīķe E, Vanags I (2014) Arterial stiffness measured by pulse wave velocity in patients with early sepsis/Artēriju Cietība Un Pulsa Viļņa Izplatīšanās Ātrums Pacientiem Ar Agrīnu Sepsi. In: Proceedings of the Latvian Academy of sciences section B natural, exact, and applied sciences 68 (5–6). doi:10.2478/prolas-2014-0030
Inoue N, Maeda R, Kawakami H, Shokawa T, Yamamoto H, Ito C, Sasaki H (2009) Aortic pulse wave velocity predicts cardiovascular mortality in middle-aged and elderly Japanese men. Circ J 73(3):549–553
Ngim CA, Abdul Rahman AR, Ibrahim A (1999) Pulse wave velocity as an index of arterial stiffness: a comparison between newly diagnosed (untreated) hypertensive and normotensive middle-aged Malay men and its relationship with fasting insulin. Acta Cardiologica 54(5):277–282
Laurent S, Katsahian S, Fassot C, Tropeano AI, Gautier I, Laloux B, Boutouyrie P (2003) Aortic stiffness is an independent predictor of fatal stroke in essential hypertension. Stroke 34(5):1203–1206. doi:10.1161/01.STR.0000065428.03209.64
Cruickshank K (2002) Aortic pulse-wave velocity and its relationship to mortality in diabetes and glucose intolerance: an integrated index of vascular function? Circulation 106(16):2085–2090. doi:10.1161/01.cir.0000033824.02722.f7
Takashima N, Turin TC, Matsui K, Rumana N, Nakamura Y, Kadota A, Saito Y, Sugihara H, Morita Y, Ichikawa M, Hirose K, Kawakani K, Hamajima N, Miura K, Ueshima H, Kita Y (2014) The relationship of brachial-ankle pulse wave velocity to future cardiovascular disease events in the general Japanese population: the Takashima study. J Hum Hypertens 28(5):323–327. doi:10.1038/jhh.2013.103
Blacher J, Guerin AP, Pannier B, Marchais SJ, Safar ME, London GM (1999) Impact of aortic stiffness on survival in end-stage renal disease. circulation 99(18):2434–2439. doi:10.1161/01.cir.99.18.2434
Yamashina A, Tomiyama H, Takeda K, Tsuda H, Arai T, Hirose K, Koji Y, Hori S, Yamamoto Y (2002) Validity, reproducibility, and clinical significance of noninvasive brachial-ankle pulse wave velocity measurement. Hypertens Res 25(3):359–364. doi:10.1291/hypres.25.359
Blacher J, Asmar R, Djane S, London GM, Safar ME (1999) Aortic pulse wave velocity as a marker of cardiovascular risk in hypertensive patients. Hypertension 33(5):1111–1117. doi:10.1161/01.hyp.33.5.1111
Wirch JL, Wolfe LA, Weissgerber TL, Davies GA (2006) Cold pressor test protocol to evaluate cardiac autonomic function. Appl Physiol Nutr Metab 31(3):235–243. doi:10.1139/h05-018
Silverthorn DU, Michael J (2013) Cold stress and the cold pressor test. Adv Physiol Educ 37(1):93–96. doi:10.1152/advan.00002.2013
Parati G, Ochoa JE, Lombardi C, Bilo G (2013) Assessment and management of blood-pressure variability. Nat Rev Cardiol 10(3):143–155. doi:10.1038/nrcardio.2013.1
Rothwell PM, Howard SC, Dolan E, O’Brien E, Dobson JE, Dahlöf B, Sever PS, Poulter NR (2010) Prognostic significance of visit-to-visit variability, maximum systolic blood pressure, and episodic hypertension. Lancet 375(9718):895–905. doi:10.1016/S0140-6736(10)60308-X
Gomez-Marcos MA, Recio-Rodriguez JI, Patino-Alonso MC, Gomez-Sanchez L, Agudo-Conde C, Gomez-Sanchez M, Rodriguez-Sanchez E, Garcia-Ortiz L, Vasorisk G (2012) Ambulatory arterial stiffness indices and target organ damage in hypertension. BMC Cardiovasc Disord 12:1. doi:10.1186/1471-2261-12-1
Electrophysiology TFotESoCtNASoP (1996) Heart rate variability: standards of measurement, physiological interpretation, and clinical use. Circulation 93(5):1043–1065. doi:10.1161/01.cir.93.5.1043
Manios E, Michas F, Stamatelopoulos K, Barlas G, Koroboki E, Tsouma I, Vemmos K, Zakopoulos N (2014) Short-term beat-to-beat but not ambulatory blood pressure variability is correlated to carotid intima-media thickness. Blood Press Monit 19(5):288–293. doi:10.1097/MBP.0000000000000062
Stauss HM (2007) Identification of blood pressure control mechanisms by power spectral analysis. Clin Exp Pharmacol Physiol 34(4):362–368. doi:10.1111/j.1440-1681.2007.04588.x
Liu Q, Poon CCY, Zhang YT (2011) Time?–frequency analysis of variabilities of heart rate, systolic blood pressure and pulse transit time before and after exercise using the recursive autoregressive model. Biomedical Signal Process Control 6(4):364–369. doi:10.1016/j.bspc.2011.03.009
Hashimoto J, Ito S (2013) Aortic stiffness determines diastolic blood flow reversal in the descending thoracic aorta: potential implication for retrograde embolic stroke in hypertension. Hypertension 62(3):542–549. doi:10.1161/hypertensionaha.113.01318
Karras A, Haymann JP, Bozec E, Metzger M, Jacquot C, Maruani G, Houillier P, Froissart M, Stengel B, Guardiola P, Laurent S, Boutouyrie P, Briet M, Nephro Test Study G (2012) Large artery stiffening and remodeling are independently associated with all-cause mortality and cardiovascular events in chronic kidney disease. Hypertension 60(6):1451–1457. doi:10.1161/HYPERTENSIONAHA.112.197210
Kikuya M, Ohkubo T, Metoki H, Asayama K, Hara A, Obara T, Inoue R, Hoshi H, Hashimoto J, Totsune K, Satoh H, Imai Y (2008) Day-by-day variability of blood pressure and heart rate at home as a novel predictor of prognosis: the Ohasama study. Hypertension 52(6):1045–1050. doi:10.1161/HYPERTENSIONAHA.107.104620
Kaess BM, Rong J, Larson MG et al (2012) Aortic stiffness, blood pressure progression, and incident hypertension. JAMA 308(9):875–881. doi:10.1001/2012.jama.10503
Schillaci G, Bilo G, Pucci G, Laurent S, Macquin-Mavier I, Boutouyrie P, Battista F, Settimi L, Desamericq G, Dolbeau G, Faini A, Salvi P, Mannarino E, Parati G (2012) Relationship between short-term blood pressure variability and large-artery stiffness in human hypertension: findings from 2 large databases. Hypertension 60(2):369–377. doi:10.1161/HYPERTENSIONAHA.112.197491
Mancia G, Parati G, Pomidossi G, Casadei R, Di Rienzo M, Zanchetti A (1986) Arterial baroreflexes and blood pressure and heart rate variabilities in humans. Hypertension 8(2):147–153. doi:10.1161/01.hyp.8.2.147
Mancia G, Grassi G (2000) Mechanisms and clinical implications of blood pressure variability. J Cardiovasc Pharmacol 35 (0160-2446 (Print)):S15–S19. doi:10.1097/00005344-200000004-00003
Garcia-Garcia A, Garcia-Ortiz L, Recio-Rodriguez JI, Patino-Alonso MC, Agudo-Conde C, Rodriguez-Sanchez E, Gomez-Marcos MA (2013) Relationship of 24-h blood pressure variability with vascular structure and function in hypertensive patients. Blood Press Monit 18(2):101–106. doi:10.1097/MBP.0b013e32835ebc58
Kotsis V, Stabouli S, Karafillis I, Papakatsika S, Rizos Z, Miyakis S, Goulopoulou S, Parati G, Nilsson P (2011) Arterial stiffness and 24 h ambulatory blood pressure monitoring in young healthy volunteers: the early vascular ageing Aristotle University Thessaloniki study (EVA-ARIS Study). Atherosclerosis 219(1):194–199. doi:10.1016/j.atherosclerosis.2011.07.111
Parati G (2005) Blood pressure variability: its measurement and significance in hypertension. J Hypertens 23:S19–S25. doi:10.1007/s11906-006-0051-6
Huisman H, Van Rooyen J, Malan N, Eloff F, Laubscher P, Steyn H, Pretorius P (2002) Cardiovascular reactivity patterns elicited by the cold pressor test as a function of aging. Aging Clin Exp Res 14(3):202–207. doi:10.1007/BF03324437
Hess KL, Wilson TE, Sauder CL, Gao Z, Ray CA, Monahan KD (2009) Aging affects the cardiovascular responses to cold stress in humans. J Appl Physiol 107(4):1076–1082. doi:10.1152/japplphysiol.00605.2009
White LR, Juul R, Skaanes KO, Aasly J (2000) Cytokine enhancement of endothelin ET(B) receptor-mediated contraction in human temporal artery. Eur J Pharmacol 406(1):117–122. doi:10.1016/S0014-2999(00)00642-7
Kim K-I, Lee J-H, Chang H-J, Cho Y-S, Youn T-J, Chung W-Y, Chae I-H, Choi D-J, Park KU, Kim C-H (2008) Association between blood pressure variability and inflammatory marker in hypertensive patients. Circ J 72(2):293–298. doi:10.1253/circj.72.293
Sa Cunha R, Pannier B, Benetos A, London GM, Mallion JM, Safar ME (1997) Association between high heart rate and high arterial rigidity in normotensive and hypertensive subjects. J Hypertens 15(12 Pt 1):1423–1430
Palatini P, Benetos A, Grassi G, Julius S, Kjeldsen SE, Mancia G, Narkiewicz K, Parati G, Pessina AC, Ruilope LM, Zanchetti A (2006) Identification and management of the hypertensive patient with elevated heart rate: statement of a European Society of Hypertension Consensus Meeting. J Hypertens 24(4):603–610. doi:10.1097/01.hjh.0000217838.49842.1e
Chatzizisis YS, Coskun AU, Jonas M, Edelman ER, Feldman CL, Stone PH (2007) Role of endothelial shear stress in the natural history of coronary atherosclerosis and vascular remodeling: molecular, cellular, and vascular behavior. J Am Coll Cardiol 49(25):2379–2393. doi:10.1016/j.jacc.2007.02.059
Acknowledgments
This work was supported partly by the Technology Planning Project of Guangdong Province (2013A022100036, 2014A020212257), the China Postdoctoral Science Foundation (201003745), Shenzhen innovation funding (JCYJ20140901003939025), Guangdong Image-guided Therapy Innovation Team (2011S013) and the Key Lab for Health Informatics of Chinese Academy of Sciences.
Author information
Authors and Affiliations
Corresponding author
Additional information
Lin Xu, Hongqiang Lei and Jian Qiu have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Xu, L., Lei, H., Qiu, J. et al. Correlation between beat-to-beat blood pressure variability and arterial stiffness in healthy adults in the cold pressor test. Australas Phys Eng Sci Med 39, 977–985 (2016). https://doi.org/10.1007/s13246-015-0378-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13246-015-0378-x