Abstract
Purpose
Preserved ejection fraction heart failure (HFpEF) can be treated by installing a shunt in the interatrial septum, which relieves excess pressure in the left atrium by allowing blood to flow from left to right. This technique has proven effective in clinical trials, but the details of the flow through the shunted heart are not well understood. The current study aims to collect quantitative data on the relationship between pressure and flow rate in such shunts.
Methods
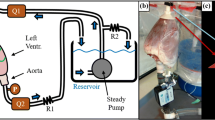
An in vitro, shunted double atrium flow phantom was fabricated and used to investigate the relationship between pressure drop and flow across an interatrial shunt. Flow rate was controlled and the resulting pressure drop across the shunt was measured for a variety of flow cases, including steady and pulsatile flow, flow rate waveforms typical of healthy and failing hearts, and low and high heart rates.
Results
The results show a positive relationship between shunt flow rate and pressure drop which is more pronounced in steady flow than in pulsatile flow. Increasing heart rate increases the time-averaged pressure drop across the shunt but not the maximum pressure drop. For steady-flow cases, large changes in pressure drop resulting from moderate changes in flow rate suggest a flow regime transition during parts of the cardiac cycle. Comparison of time-averaged pulsatile flow pressure measurements with steady-flow measurements and two analytical plate-orifice models suggests that none approximate pulsatile flow accurately.
Conclusions
The flow rate/pressure drop relationship across an in vitro model of an interatrial shunt has been measured for a variety of physiologically relevant cases. Among other things, the results suggest that steady flow approximations to the heart’s pulsatile flow should be used with caution and simplified theoretical models do not approximate the flow rate/pressure drop relationship accurately.








Similar content being viewed by others
References
Abebe, T. B., E. A. Gebreyohannes, Y. G. Tefera, and T. M. Abegaz. Patients with hfpef and hfref have different clinical characteristics but similar prognosis: a retrospective cohort study. BMC Cardiovasc. Disord., 16:1–8, 2016.
Abudiab, M. M., M. M. Redfield, V. Melenovsky, T. P. Olson, D. A. Kass, B. D. Johnson, and B. A. Borlaug. Cardiac output response to exercise in relation to metabolic demand in heart failure with preserved ejection fraction. Eur. J. Heart Fail. 15:776–785, 2013.
Ahmed, R., B. Botezatu, M. Nanthakumar, T. Kaloti, and A. Harky.Surgery for heart failure: treatment options and implications. J. Cardiac Surg. 36:1511–1519, 2020.
Anwar, A. M., M. L. Geleijnse, O. I. I. Soliman, J. S. McGhie, R. Frowijn, A. Nemes, A. E. van den Bosch, T. W. Galema, and F. J. ten Cate. Assessment of normal tricuspid valve anatomy in adults by real-time three-dimensional echocardiography. Int. J. Cardiovasc. Imaging 23:717–724, 2007.
Ascuitto, R., N. Ross-Ascuitto, M. Guillot, and C. Celestin. Computational fluid dynamics characterization of pulsatile flow in central and sano shunts connected to the pulmonary arteries: importance of graft angulation on shear stress-induced, platelet-mediated thrombosis. Interact. Cardiovasc. Thorac. Surg. 25:414–421, 2017.
Aslan, S., M. Guillot, N. Ross-Ascuitto, and R. Ascuitto. Hemodynamics in a bidirectional glenn shunt supplemented with a modified blalock-taussig shunt: computational fluid dynamics assessment. Prog. Pediatr. Cardiol. 60:101256, 2021.
Aune, E., M. Baekkevar, J. Roislien, O. Rodevand, and J. E. Otterstad. Normal reference ranges for left and right atrial volume indexes and ejection fractions obtained with real-time three-dimensional echocardiography. Eur. J. Echocardiogr. 10:738–744, 2009.
Borlaug, B. A., and W. J. Paulus. Heart failure with preserved ejection fraction: pathophysiology, diagnosis, and treatment. Eur. Heart J. 32:670–679, 2011.
Celestin, C., M. Guillot, N. Ross-Ascuitto, and R. Ascuitto. Computational fluid dynamics characterization of blood flow in central aorta pulmonary artery connections: Importance of shunt angulation as a determinant of shear stress-induced thrombosis. Pediatr. Cardiol. 36:600–615, 2015.
Chnafa, C., S. Mendez, F. Nicoud, R. Moreno, S. Nottin, and I. Schuster. Image-based patient-specific simulation: a computational modelling of the human left heart haemodynamics. Comput. Methods Biomech. Biomed. Eng. 15(S1):74–75, 2012.
Debl, K., B. Djavidani, S. Buchner, N. Heinicke, F. Poschenrieder, S. Feuerbach, G. Riegger, and A. Luchner. Quantification of left-to-right shunting in adult congenital heart disease: phase-contrast cine MRI compared with invasive oximetry. Br. J. Radiol. 82:386–391, 2009.
Doshi, D., and D. Burkhoff. Cardiovascular simulation of heart failure pathophysiology and therapeutics. J. Cardiac Fail. 22(4):303–311, 2106.
Dunn, T. S. I., P. Patel, B. Abazid, H. M. Magaraj, R. V. Desai, H. Gupta, and S. G. Lloyd. Quantification of pulmonary/systemic shunt ratio by single-acquisition phase-contrast cardiovascular magnetic resonance. Echocardiography 36:1181–1190, 2019.
Edelmann, F. Facts and numbers on epidemiology and pharmacological treatment of heart failure with preserved ejection fraction. ESC Heart Fail. 2:41–45, 2015.
Ernst, G., C. Stoellberger, F. Abzieher, W. Veit-Dirscherl, E. Bonner, B. Bibus, B. Schneider, and J. Slany. Morphology of the left atrial appendage. Anat. Rec. 242:553–561, 1995.
Ewert, P., F. Berger, N. Nagdyman, O. Kretschmar, S. Dittrich, H. Abdul-Khaliq, and P. Lange. Masked left ventricular restriction in elderly patients with atrial septal defects: a contraindication for closure? Catheter Cardiovasc. Intervention 52(2):177–180, 2001.
Galderisi, M. Diastolic dysfunction and diastolic heart failure: diagnostic, prognostic and theraputic aspects. Cardiovasc. Ultrasound 3(9):1–14, 2005.
Griffin, J. M., B. A. Borlaug, J. Komtebedde, S. E. Litwin, S. J. Shah, D. M. Kaye, E. Hoendermis, G. Hasenfuss, F. Gustafsson, E. Wolsk, N. Uriel, and D. Burkhoff. Impact of interatrial shunts on invasive hemodynamics and exercise tolerance in patients with heart failure. J. Am. Heart Assoc. 9:1–15, 2020.
Hanneman, K., M. Sivagnanam, E. T. Nguyen, R. Wald, A. Breiser, A. M. Crean, S. Ley, and B. J. Wintersperger, Magnetic resonance assessment of pulmonary (qp) to systemic (qs) flows using 4d phase-contrast imaging. Acad. Radiol. 21:1002–1008, 2014.
Hasenfuss, ,G. C. Hayward, D. Burkhoff, F. E. Silvestry, S. McKenzie, F. Gustafsson, F. Malek, J. Van der Heyden, I. Lang, M. C. Petrie, J. G. F. Cleland, M. Leon, and D. M. Kaye. A transcatheter intracardiac shunt device for heart failure with preserved ejection fraction (reduce lap-hf): a muticentre, open-label, single-arm, phase 1 trial. The Lancet 387:1298–1304, 2016.
He, X., and D. N. Ku. Unsteady entrance flow development in a straight tube. J. Biomech. Eng. 116:355–360, 1994.
Hiraoka, A., R. Symons, J. A. Bogaert, P. Morais, A. Van De Bruaene, W. Budts, and J. Bogaert. Assessment of long-term cardiac adaptation in adult patients with type II atrial septal defect. Eur. Radiol. 31:1905–1914, 2021.
Kato, A., J. P. Sandoval, D. Mroczek, R. Chaturvedi, H. Houle, B. Georgescu, S. J. Yoo, L. N. Benson, and K. J. Lee. Automated 3-dimensional single-beat real-time volume colour flow doppler echocardiography in children: a validation study of right and left heart flows. Can. J. Cardiol. 34:726–735, 2018.
Kaye, D. M., G. Hasenfuss, P. Neuzil, M. Post, R. Doughty, J. N. Trochu, A. Kolodziej, R. Westenfeld, M. Penicka, M. Rosenberg, A. Walton, D. Muller, D. Walters, J. Hausleiter, P. Raake, M. C. Petrie, M. Bergmann, G. Jondeau, T. Feldman, D. J. van Veldhuisen, P. Ponikowski, F. E. Silvestry, D. Burkhoff, and C. Hayward. One-year outcomes after transcatheter insertion of an interatrial shunt device for the management of heart failure with preserved ejection fraction. Circulation 9(12):e003662, 2016.
Kaye, D., S. J. Shah, B. A. Borlaug, F. Gustafsson, J. Komtebedde, S. Kubo, C. Magnin, M. S. Maurer, T. Feldman, and D. Burkhoff. Effects of an interatrial shunt on rest and exercise hemodynamics: results of a computer simulation in heart failure. J. Cardiac Fail. 20(3):212–221, 2014.
Kay, D. M., M. C. Petrie, S. McKenzie, G. Hasenfuss, F. Malek, M. Post, R. N. Doughty, J. N. Trochu, F. Gustafsson, I. Lang, A. Kolodziej, R. Westenfeld, M. Penicka, M. Rosenberg, J. Hausleiter, P. Raake, G. Jondeau, M. W. Bergmann, T. Spelman, H. Aytug, P. Ponikowski, and C. Hayward, Impact of an interatrial shunt device on survival and heart failure hospitalization in patients with preserved ejection fraction. ESC Heart Fail. 6:62–69, 2019.
Kim, Y. H., E. M. Marom, J. E. I. Herndon, and H. P. McAdams. Pulmonary vein diameter, cross-sectional area, and shape: CT analysis. Radiology 235(1):43–49, 2005.
Mihalef, V., R. I. Ionasec, P. Sharma, B. Georgescu, I. Voigt, M. Suehling, and D. Comaniciu. Patient-specific modelling of whole heart anatomy, dynamics and haemodynamics from four-dimensional cardiac CT images. Interface Focus 1:286–296, 2011.
Mittal, R. Matters of the heart. J. Fluid Mech. 844:1–4, 2018.
Miyagi, C., T. Miyamoto, J. H. Karimov, R. C. Starling, and K. Fukamachi, Device-based treatment options for heart failure with preserved ejection fraction. Heart Fail. Rev. 26:749–762, 2021.
Mookadam, F., T. A. Warsame, H. S. Yang, U. R. Emani, C. P. Appleton, and S. F. Raslan. Effect of positional changes on inferior vena cava size. Eur. J. Echocardiogr. 12:322–325, 2011.
Nishikawa, T., K. Saku, K. Uike, K. Uemura, G. Sunagawa, T. Tohyama, K. Yoshida, T. Kishi, K. Sunagawa, and H. Tsutsui. Prediction of haemodynamics after interatrial shunt for heart failure using the generalized circulatory equilibrium. ESC Heart Fail. 7:3075–3085, 2020.
Ormiston, J. A., P. M. Shah, C. Tei, and M. Wong. Size and motion of the mitral valve annulus in man: I. Two-dimensional echocardiographic method and findings in normal subjects. Circulation 64(1):113–120, 1981.
Owan, T. E., D. O. Hodge, R. M. Herges, S. J. Jacobsen, V. L. Roger, and M. M. Redfield. Trends in prevalence and outcome of heart failure with preserved ejection fraction. N. Engl. J. Med. 355:251–259, 2006.
Prather, R., J. Seligson, M. Ni, E. Divo, A. Kassab, and W. DeCampli. Patient-specific multiscale computational fluid dynamics assessment of embolization rates in the hybrid norwood: effects of size and placement of the reverse blalock-taussig shunt. Can. J. Physiol. Pharmacol. 96:690–700, 2018.
Roldan-Alzate, A., S. Garcia-Rodriguez, P. V. Anagnostopoulos, S. Srinivasan, O. Wieben, and C. J. Francois. Hemodynamic study of tcpc using in vivo and in vitro 4d flow mri and numerical simulation. J. Biomech. 48:1325–1330, 2015.
Sonavane, S. K., D. M. Milner, S. P. Singh, A. K. A. Aal, K. S. Shahir, and A. Chaturvedi. Comprehensive imaging review of the superior vena cava. RadioGraphics 35:1873–1892, 2015.
Upadhya, B., M. J. Haykowsky, and D. W. Kitzman. Therapy for heart failure with preserved ejection fraction: current status, unique challenges, and future directions. Heart Fail. Rev. 23: 609–629, 2018.
Wessler, J., D. Kaye, F. Gustafsson, M. C. Petrie, G. Hasenfuss, C. S. P. Lam, B. A. Borlaug, J. Komtebedde, T. Feldman, S. Shah, and D. Burkhoff. Impact of baseline hemodynamics on the effects of a transcatheter interatrial shunt device in heart failure with preserved ejection fraction. Circulation 11:e004540, 2018.
Yamasaki, Y., S. Kawanami, T. Kamitani, K. Sagiyama, I. Sakamoto, K. I. Hiasa, H. Yabuuchi, M. Nagao, and H. Honda, Noninvasive quantification of left-to-right shunt by phase contrast magnetic resonance imaging in secundum atrial septal defect: the effects of breath holding and comparison with invasive oximetry. Int. J. Cardiovasc. Imaging 34:931–937, 2018.
Zhang, N., H. Yuan, X. Chen, J. Liu, Q. Jian, M. Huang, and K. Zhang. Computational fluid dynamics characterization of two patient-specific systemic-to-pulmonary shunts before and after operation. Computat. Math. Methods Med. 2019.
Funding
Funding was supported by Corvia Medical, Inc.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Erica Cherry Kemmerling declares that she has no conflict of interest.
Additional information
Associate Editor Igor Efimov oversaw the review of this article.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cherry Kemmerling, E. In Vitro Pressure Measurements Across an Interatrial Shunt for HFpEF Treatment. Cardiovasc Eng Tech 13, 662–672 (2022). https://doi.org/10.1007/s13239-021-00607-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13239-021-00607-x