Abstract
Purpose
A credible computational fluid dynamics (CFD) model can play a meaningful role in evaluating the safety and performance of medical devices. A key step towards establishing model credibility is to first validate CFD models with benchmark experimental datasets to minimize model-form errors before applying the credibility assessment process to more complex medical devices. However, validation studies to establish benchmark datasets can be cost prohibitive and difficult to perform. The goal of this initiative sponsored by the U.S. Food and Drug Administration is to generate validation data for a simplified centrifugal pump that mimics blood flow characteristics commonly observed in ventricular assist devices.
Methods
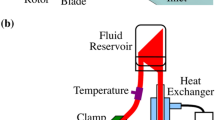
The centrifugal blood pump model was made from clear acrylic and included an impeller, with four equally spaced, straight blades, supported by mechanical bearings. Particle Image Velocimetry (PIV) measurements were performed at several locations throughout the pump by three independent laboratories. A standard protocol was developed for the experiments to ensure that the flow conditions were comparable and to minimize systematic errors during PIV image acquisition and processing. Velocity fields were extracted at the pump entrance, blade passage area, back gap region, and at the outlet diffuser regions. A Newtonian blood analog fluid composed of sodium iodide, glycerin, and water was used as the working fluid. Velocity measurements were made for six different pump flow conditions, with the blood-equivalent flow rate ranging between 2.5 and 7 L/min for pump speeds of 2500 and 3500 rpm.
Results
Mean intra- and inter-laboratory variabilities in velocity were ~ 10% at the majority of the measurement locations inside the pump. However, the inter-laboratory variability increased to more than ~ 30% in the exit diffuser region. The variability between the three laboratories for the peak velocity magnitude in the diffuser region ranged from 5 to 25%. The bulk velocity field near the impeller changed proportionally with the rotational speed but was relatively unaffected by the pump flow rate. In contrast, flow in the exit diffuser region was sensitive to both the flow rate and the rotational speed. Specifically, at 3500 rpm, the exit jet tilted toward the inner wall of the diffuser at a flow rate of 2.5 L/min, but the jet tilted towards the outer wall when the flow rate was 7 L/min.
Conclusions
Inter-laboratory experimental mean velocity data (and the corresponding variance) were obtained for the FDA pump model and are available for download at https://nciphub.org/wiki/FDA_CFD. Experimental datasets from the inter-laboratory characterization of benchmark flow models, including the blood pump model presented herein and our previous nozzle model, can be used for validating future CFD studies and to collaboratively develop guidelines on best practices for verification, validation, uncertainty quantification, and credibility assessment of CFD simulations in the evaluation of medical devices (e.g. ASME V&V 40 standards working group).













Similar content being viewed by others
References
Aycock, K. I., R. L. Campbell, F. C. Lynch, K. B. Manning, and B. A. Craven. The importance of hemorheology and patient anatomy on the hemodynamics in the inferior vena cava. Ann. Biomed. Eng. 44:3568–3582, 2016.
Behbahani, M., M. Behr, M. Hormes, U. Steinseifer, D. Arora, O. Coronado, and M. Pasquali. A review of computational fluid dynamics analysis of blood pumps. Eur. J. Appl. Math. 20:363, 2009.
Bhushan, S., D. K. Walters, and G. W. Burgreen. Laminar, turbulent, and transitional simulations in benchmark cases with cardiovascular device features. Cardiovasc. Eng. Technol. 4:408–426, 2013.
CDRH. CDRH regulatory science report, http://www.fda.gov/downloads/MedicalDevices/ScienceandResearch/UCM521503.pdf, 2018.
Day, S. W., and J. C. McDaniel. PIV measurements of flow in a centrifugal blood pump: steady flow. J. Biomech. Eng. 127:244, 2005.
Delorme, Y. T., K. Anupindi, and S. H. Frankel. Large eddy simulation of FDA’s idealized medical device. Cardiovasc. Eng. Technol. 2013. https://doi.org/10.1007/s13239-013-0161-7.
Fabritious, B. Application of Genetic Algorithms to Problems in Computational Fluid Dynamics. Exeter: University of Exeter, 2014.
Giarra, M. N. Shear Stress Distribution and Hemolysis Measurements in a Centrifugal Blood Pump. Rochester: Mechanical Engineering, Rochester Institute of Technology, 2009.
Haddad, T., A. Himes, L. Thompson, T. Irony, R. Nair, and MDIC Computer Modeling and Simulation Working Group Participants. Incorporation of stochastic engineering models as prior information in Bayesian medical device trials. J. Biopharm. Stat. 27:1089–1103, 2017.
Hariharan, P., M. Giarra, V. Reddy, S. W. Day, K. B. Manning, S. Deutsch, S. F. Stewart, M. R. Myers, M. R. Berman, G. W. Burgreen, E. G. Paterson, and R. A. Malinauskas. Multilaboratory particle image velocimetry analysis of the FDA benchmark nozzle model to support validation of computational fluid dynamics simulations. J. Biomech. Eng. 133:041002, 2011.
Himes, A. H., T. Haddad, and D. Bardot. Augmenting a clinical study with virtual patient models: Food and Drug Administration and industry collaboration 1. J. Med. Dev. 10(3):030947, 2016.
Smithee, I., and S. P. Gent. Computational fluid dynamics modeling of blood as a heterogeneous fluid. In: Design of Medical Devices Conference, 2018.
Janiga, G. Large eddy simulation of the FDA benchmark nozzle for a Reynolds number of 6500. Comput. Biol. Med. 47:113–119, 2014.
Lance, B. W., J. R. Harris, and B. L. Smith. Experimental validation benchmark data for computational fluid dynamics of mixed convection on a vertical flat plate. J. Verif. Valid. Uncertain. Quant. 1:021005, 2016.
Malinauskas, R. A., P. Hariharan, S. W. Day, L. H. Herbertson, M. Buesen, U. Steinseifer, K. I. Aycock, B. C. Good, S. Deutsch, K. B. Manning, and B. A. Craven. FDA benchmark medical device flow models for CFD validation. ASAIO J. 63:150–160, 2017.
McCroskey, W. J. A Critical Assessment of Wind Tunnel Results for the NACA 0012 Airfoil. Moffett Field: N.A.a.S. Administration, 1987.
Morrison, T. M., M. L. Dreher, S. Nagaraja, L. M. Angelone, and W. Kainz. The role of computational modeling and simulation in the total product life cycle of peripheral vascular devices. J. Med. Device 2017. https://doi.org/10.1115/1.4035866.
Nguyen, T. T. A method for matching the refractive index and kinematic viscosity of a blood analog for flow visualization in hydraulic cardiovascular models. J. Biomech. Eng. 126:529, 2004.
Oberkampf, W. L., and T. G. Trucano. Verification and validation in computational fluid dynamics. Prog. Aerosp. Sci. 38:209–272, 2002.
Oberkampf, W. L., and T. G. Trucano. Verification and Validation in Computational Fluid Dynamics. Albuquerque: S.N. Laboratories, 2002.
Passerini, T., A. Quaini, U. Villa, A. Veneziani, and S. Canic. Validation of an open source framework for the simulation of blood flow in rigid and deformable vessels. Int. J. Numer. Methods Biomed. Eng. 29:1192–1213, 2013.
Pathmanathan, P., R. A. Gray, V. J. Romero, and T. M. Morrison. Applicability analysis of validation evidence for biomedical computational models. J. Verif. Valid. Uncertain. Quant. 2:021005, 2017.
Sotiropoulos, F. Computational fluid dynamics for medical device design and evaluation: are we there yet? Cardiovasc. Eng. Technol. 3:137–138, 2012.
Steinman, D. A., Y. Hoi, P. Fahy, L. Morris, M. T. Walsh, N. Aristokleous, A. S. Anayiotos, Y. Papaharilaou, A. Arzani, S. C. Shadden, P. Berg, G. Janiga, J. Bols, P. Segers, N. W. Bressloff, M. Cibis, F. H. Gijsen, S. Cito, J. Pallares, L. D. Browne, J. A. Costelloe, A. G. Lynch, J. Degroote, J. Vierendeels, W. Fu, A. Qiao, S. Hodis, D. F. Kallmes, H. Kalsi, Q. Long, V. O. Kheyfets, E. A. Finol, K. Kono, A. M. Malek, A. Lauric, P. G. Menon, K. Pekkan, M. Esmaily Moghadam, A. L. Marsden, M. Oshima, K. Katagiri, V. Peiffer, Y. Mohamied, S. J. Sherwin, J. Schaller, L. Goubergrits, G. Usera, M. Mendina, K. Valen-Sendstad, D. F. Habets, J. Xiang, H. Meng, Y. Yu, G. E. Karniadakis, N. Shaffer, and F. Loth. Variability of computational fluid dynamics solutions for pressure and flow in a giant aneurysm: the ASME 2012 Summer Bioengineering Conference CFD Challenge. J. Biomech. Eng. 135(2013):021016, 2012.
Stewart, S. F. C., P. Hariharan, E. G. Paterson, G. W. Burgreen, V. Reddy, S. W. Day, M. Giarra, K. B. Manning, S. Deutsch, M. R. Berman, M. R. Myers, and R. A. Malinauskas. Results of FDA’s first interlaboratory computational study of a nozzle with a sudden contraction and conical diffuser. Cardiovasc. Eng. Technol. 4:374–391, 2013.
Stewart, S. F. C., E. G. Paterson, G. W. Burgreen, P. Hariharan, M. Giarra, V. Reddy, S. W. Day, K. B. Manning, S. Deutsch, M. R. Berman, M. R. Myers, and R. A. Malinauskas. Assessment of CFD performance in simulations of an idealized medical device: results of FDA’s First Computational Interlaboratory Study. Cardiovasc. Eng. Technol. 3:139–160, 2012.
Stiehm, M., C. Wüstenhagen, S. Siewert, N. Grabow, and K.-P. Schmitz. Numerical simulation of pulsatile flow through a coronary nozzle model based on FDA’s benchmark geometry. Curr. Direct. Biomed. Eng. 3(2):775–778, 2017.
American Society of Mechanical Engineers. Draft Standard (Under Development)—Verification and Validation in Computational Modeling of Medical Devices. New York: ASME.
Trias, M., A. Arbona, J. Masso, B. Minano, and C. Bona. FDA’s nozzle numerical simulation challenge: non-Newtonian fluid effects and blood damage. PLoS ONE 9:e92638, 2014.
U.S. FDA. Guidance for Industry and Food and Drug Administration Staff—Reporting of Computational Modeling Studies in Medical Device Submissions, 2016.
Valen-Sendstad, K., M. Piccinelli, and D. A. Steinman. High-resolution computational fluid dynamics detects flow instabilities in the carotid siphon: implications for aneurysm initiation and rupture? J. Biomech. 47:3210–3216, 2014.
Vogel, J. C., and J. K. Eaton. Combined heat transfer and fluid dynamic measurements downstream of a backward-facing step. J. Heat Transf. 107:922, 1985.
White, A. T., and C. K. Chong. Rotational invariance in the three-dimensional lattice Boltzmann method is dependent on the choice of lattice. J. Comput. Phys. 230:6367–6378, 2011.
Zmijanovic, V., S. Mendez, V. Moureau, and F. Nicoud. About the numerical robustness of biomedical benchmark cases: interlaboratory FDA’s idealized medical device. Int. J. Numer. Methods Biomed. Eng. 2017. https://doi.org/10.1002/cnm.2789.
Acknowledgments
Our thanks to Dr. Tina Morrison at the FDA/Center for Devices and Radiological Health for review of the manuscript and helpful comments. Matthew Giarra (Rochester Institute of Technology) was the principal design engineer for the blood pump model, under the direction of Dr. Steven W. Day and in collaboration with Dr. Richard A. Malinauskas.
Conflict of Interest
All authors declare that they have no conflicts of interest.
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editors David A. Steinman, Francesco Migliavacca, and Ajit P. Yoganathan oversaw the review of this article.
Rights and permissions
About this article
Cite this article
Hariharan, P., Aycock, K.I., Buesen, M. et al. Inter-Laboratory Characterization of the Velocity Field in the FDA Blood Pump Model Using Particle Image Velocimetry (PIV). Cardiovasc Eng Tech 9, 623–640 (2018). https://doi.org/10.1007/s13239-018-00378-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13239-018-00378-y