Abstract
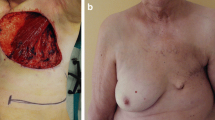
Locally advanced breast cancer (LABC) constitutes 40–50% of breast cancer in developing countries. Large soft tissue defects after mastectomy often require some additional cover. The primary aim of reconstruction in this group should be an expeditious and simple closure with good-quality skin cover, early recovery, and short hospital stay so that the patients can receive early post-operative radio-chemotherapy. Thoracoabdominal (TA) flap is a type-c fasciocutaneous flap and the skin and fat of the upper abdomen are used, based on medial or lateral perforating vessels. We present our experience of TA flap cover for large post-mastectomy defects. A retrospective analysis of prospectively maintained breast cancer database in the Department of Surgical Oncology from January 1994 to December 2017 at All India Institute of Medical Sciences, New Delhi, was performed. The medical records of patients undergoing TA flap cover were analyzed to assess operative duration, blood loss, post-operative morbidity, hospital stay, adjuvant treatment, recurrence patterns, and survival outcome. A total of 3142 breast cancer patients underwent surgery, of which 1840 were LABC and 88 patients (4.13%) of LABC required flap cover for the closure of mastectomy defect. TA flap was used in majority of these patients 72/83 (86.7%) for cover. Majority was stage IIIB (54 out of 72) and we could achieveR0 resection in all patients. TA flap was done following MRM in 60 patients and RM in 12 patients. Upfront primary surgery was performed in 27 patients and 45 underwent surgery after neoadjuvant chemotherapy. Most commonly laterally based flaps were done, except 4 medially based flaps. The mean operating time was 30 min and blood loss was 45 ml. Mean hospital stay was 4.45 days. Superficial flap necrosis occurred in 6 and wound infection in 4 patients, all managed conservatively. Only 2 patients had major flap loss and required debridement and skin grafting. Planned post-operative radiation could be delivered in most of the patients in time. At a mean follow-up of 24 months, only 9 out of 72 (12.5%) patients had a loco-regional recurrence. Results of our experience show that TA flap is a simple, cost-effective procedure for managing large post-mastectomy soft tissue defects in LABC. It has huge potential in developing countries dealing with a large number of LABC because of simplicity and short learning curve.



Similar content being viewed by others
References
Leinster SJ, Webster JT (1992) Thoracoabdominal and thoracoepigastric flaps: alternatives to skin grafting after mastectomy. Clin Oncol 8:145–148
Lee SH, Cheah DS, Krishnan MM (1990) Omental transposition flap and split skin graft for locally advanced breast carcinoma. Singap Med J 31:217–220
Maxwell GP (1980) Ignio Tansini and origin of latissimus dorsi myocutaneous flap. Plast Reconst Surg 65:686–692
Deo SV, Purkayastha J, Shukla NK, Asthana S (2003) Myocutenous versus thoraco-abdominal flap cover for soft tissue defects following surgery for locally advanced and recurrent breast cancer. J Surg Oncol 83:31–35
Jhulka PK, Prasad R, Mohanti BK et al (2000) Cancer of the breast. In: Rath GK, Mohanti BK (eds) Textbook of radiation oncology. B. I. Churchill Livingstone, New Delhi, pp 239–284
Parkin DM, Pisani P, Ferlay J (1993) Estimates of the worldwide incidence of eighteen major cancers in 1985. Int J Cancer 54:594–606
Halstead WS (1895) Results of operation for cure of cancer of the breast performed at John Hopkins Hospital from June 1889 January 1894. John Hopkins Hosp Rev 4:297–350
McGraw JB, Bostwick J III, Harton CE (1979) Methods of soft tissue coverage for mastectomy defect. Clin Plast Surg 6:57–69
Nakao K, Miyata M, Ito T, Ogino N, Kawashima Y, Maeda M, Matsumoto K (1986) Omental transposition and skin grafti in patients for advanced or recurrent breast cancer. Jpn J Surg 16:112–117
Parkash S, Srinivasan R, Ananthakrishnan N (1981) Primary closure of excisional defects of the breast with local flaps: a problem in the treatment of advanced carcinoma of the breast in developing countries. Br J Plast Surg 34:291–294
Lopez JF, Bouchet Y, Dupre A (1990) The Kiricuta procedure in reconstructive surgical treatment of the breast. Surg Gynecol Obstet 170:209–211
Cheung KL, Willsher PC, Robertson JF, Bailie FB, Daly JC, Blamey RW (1997) Omental transposition flap for gross locally recurrent breast cancer. Aust N Z J Surg 67:185–186
Williams RJ, Fryyat IJ, Abbott WC, White H (1989) Omental transposition in treatment of locally advanced and recurrent breast cancer. Br J Surg 76(6):559–563
Schneider WJ, Hill LH Jr, Brown RG (1977) LD myocutaneous flap for breast reconstruction. Br J Plast Surg 30:277–281
Bostwick J III (1982) LD flap. Current applications. Ann Plast Surg 9:377–380
Hartrampf CR Jr, Schelfan M, Block PW (1982) Breast reconstruction with TRAM. Plast Reconstr Surg 69:216–225
McGraw JB, Papp C, Crammer A et al (1998) Breast reconstruction following mastectomy. In: Bland KI, Copeland EM III (eds) The breast: comprehensive management of benign and malignant diseases. WB Saunders Co, pp 962–993
Brown RG, Vasconez LO, Jurkiewicz MJ (1975) Transverse abdominal flaps and the deep epigastric arcade. Plastic Reconstr Surg 55:416–421
Bohmert H (1980) Experience in breast reconstruction with thoraco-epigastric and advancement flaps. Acta Chir Belg 79:105–110
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Suryanarayana Deo, S.V., Mishra, A., Shukla, N.K. et al. Thoracoabdominal Flap: a Simple Flap for Covering Large Post-mastectomy Soft Tissue Defects in Locally Advanced Breast Cancer. Indian J Surg Oncol 10, 494–498 (2019). https://doi.org/10.1007/s13193-019-00927-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13193-019-00927-4