Abstract
Background
Currently considered an occupational disease, the burnout syndrome affects 13–27% of the active population in multiple occupational sectors of the modern world.
Objectives
Considering the burnout syndrome from the new perspective of the predictive, preventive, personalized medicine concept as a pathological entity with a predictable appearance and evolution which allows a preventive approach and a personalized therapy, the main objective of the study is to highlight the possibility of psychotherapeutic interventions for producing measurable psychological changes in order to decrease the burnout level of hospital nurses.
Method
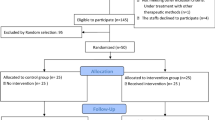
The research design is experimental, the independent variable being the participation or non-participation of nurses in psychotherapeutic sessions where specific classical psychodrama techniques are originally used. Nurses previously identified with medium or high levels of burnout participated in the clinical study, split into two groups: the experimental one, with 150-min weekly sessions, and the control one, without any intervention. Pre- and post-intervention questionnaires were administered to the members of both groups.
Results
The statistical analysis of the differences between pre- and post-intervention revealed (a) the decrease of the levels of personal burnout and of burnout generated by the working conditions and (b) the decrease of the depression and of anxiety on four dimensions (self-awareness, ergic tension, veiled and general anxiety).
Conclusions
The classical psychodrama method can be an effective solution in the prophylaxis and treatment of the burnout syndrome. The multidisciplinary approach according to the PPPM concept including changes of the environmental factors within the professional framework associated with stress control programmes can be promising solutions for the management of this syndrome.
Similar content being viewed by others
References
Montero-Marín J, Araya R. Understanding burnout according to individual differences: ongoing explanatory power evaluation of two models for measuring burnout types. BMC Public Health. 2012;12:922. https://doi.org/10.1186/1471-2458-12-922.
Karodia T. Psychometric properties of the burnout inventory. University of Pretoria. 2007, pp.2–25. https://repository.up.ac.za/bitstream/handle/2263/30563/dissertation.pdf?sequence=1. Accessed 15 Jan 2020.
Jonsdottir IH, Sjörs DA. Mechanisms in endocrinology: endocrine and immunological aspects of burnout: a narrative review. Eur J Endocrinol. 2019;180(3):R147–58. https://doi.org/10.1530/EJE-18-0741.
Grigorescu S, Cazan A, Grigorescu D, Rogozea L. The role of the personality traits and work characteristics in the prediction of the burnout syndrome among nurses—a new approach within predictive, preventive, and personalized medicine concept. EPMA J. 2018;9:355–65. https://doi.org/10.1007/s13167-018-0151-9.
Bianchi R, Schonfeld I, Laurent E. Is it time to consider the “burnout syndrome” a distinct illness? Front Public Health. 2015;3:158. https://doi.org/10.3389/fpubh.2015.00158.
World Health Organization 2019 https://www.who.int/mental_health/evidence/burn-out/en/. Accessed 6 Feb 2020.
Shackleton N, Bonell C, Jamal F, Allen E, Mathiot A, Elbourne D, et al. Teacher burnout and contextual and compositional elements of school environment. J Sch Health. 2019;89(12):977–93. https://doi.org/10.1111/josh.12839.
McLean D, Eklund K, Kilgus SP, Burns MK. Influence of teacher burnout and self-efficacy on teacher-related variance in social-emotional and behavioral screening scores. Sch Psychol. 34(5):503–11. https://doi.org/10.1037/spq0000304.
Parrello S, Ambrosetti A, Iorio I, Castelli L. School burnout, relational, and organizational factors. Front Psychol. 2019;10:1695. https://doi.org/10.3389/fpsyg.2019.01695.
Molero Jurado M, Pérez-Fuentes M, Gázquez Linares JJ, Márquez M, Martínez AM. Burnout risk and protection factors in certified nursing aides. Int J Environ Res Public Health. 2018;15(6):1116. https://doi.org/10.3390/ijerph15061116.
Dyrbye LN, Shanafelt TD, Sinsky C, Cipriano PF, Ommaya JA, Colin P, et al. Burnout among health care professionals: a call to explore and address this underrecognized threat to safe, high-quality care. Natl Acad Med. 2017. https://doi.org/10.31478/201707b.
Dyrbye LN, Shanafelt TD, Johnson P, Johnson A, Satele D, West C. A cross-sectional study exploring the relationship between burnout, absenteeism, and job performance among American nurses. BMC Nurs. 2019;18:57. https://doi.org/10.1186/s12912-019-0382-7.
Aronsson G, Theorell T, Grape T, Hammarström A, Hogstedt C, Marteinsdottir I, et al. A systematic review including meta-analysis of work environment and burnout symptoms. BMC Public Health. 2017;17:264. https://doi.org/10.1186/s12889-017-4153-7.
Grigorescu S, Grigorescu D, Rogozea L. Psihosocial factors generators of burnout in the public health system. J Med Brasov. 2016:4–10 ISSN1841–0782. http://webbut.unitbv.ro/jmb/JMB%202016%20nr%201/01_02_referat_burnout.pdf. Accessed 4 Feb 2020.
Vidotti V, Ribeiro RP, Galdino MJQ, Martins JT. Burnout syndrome and shift work among the nursing staff. Rev Lat Am Enfermagem. 2018;26:e3022. https://doi.org/10.1590/1518-8345.2550.3022.
Sánchez-Cruz J, Mugártegui-Sánchez S. Burnout syndrome among family physicians. Rev Med Inst Mex Seguro Soc. 2013;51(4):428–31.
Pradas-Hernández L, Ariza T, Gómez-Urquiza JL, Albendín-García L, De la Fuente EI, Cañadas-De la Fuente GA. Prevalence of burnout in paediatric nurses: a systematic review and meta-analysis. PLoS One. 2018;13(4):e0195039. https://doi.org/10.1371/journal.pone.0195039.
Zubairi AJ, Noordin SH. Factors associated with burnout amongresidents in a developing country. Ann Med Surg. 2016;6:60–3. https://doi.org/10.1016/j.amsu.2016.01.090.
López-López IM, Gómez-Urquiza JL, Cañadas GR, De la Fuente EI, Albendín-García L, Cañadas-De la Fuente GA. Prevalence of burnout in mental health nurses and related factors: a systematic review and meta-analysis. Int J Ment Health Nurs. 2019;28(5):1032–41. https://doi.org/10.1111/inm.12606.
Chen S, Lin S, Ruan Q, Li H, Wu S. Workplace violence and its effect on burnout and turnover attempt among Chinese medical staff. Arch Environ Occup Health. 2016;71(6):330–7. https://doi.org/10.1080/19338244.2015.1128874.
Molina-Praena J, Ramirez-Baena L, Gómez-Urquiza JL, Cañadas GR, De la Fuente EI, Cañadas-De la Fuente GA. Levels of burnout and risk factors in medical area nurses: a meta-analytic study. Int J Environ Res Public Health. 2018;15(12):2800. https://doi.org/10.3390/ijerph15122800.
Stehman CR, Zachary T, Gershaw R, Kellogg R. Burnout, drop out, suicide: physician loss in emergency medicine, part I. West J Emerg Med. 2019;20(3):485–94. https://doi.org/10.5811/westjem.2019.4.40970.
Patel RS, Bachu R, Adikey A, Malik M, Shah M. Factors related to physician burnout and its consequences: a review. Behav Sci (Basel). 2018;8(11):98. https://doi.org/10.3390/bs8110098.
West CP, Dyrbye LN, Shanafelt TD. (Mayo Clinic, Rochester, MN; and Stanford University Medical Center, Stanford, CA, USA). Physician burnout: contributors, consequences and solutions (Review). J Intern Med 2018; 283:516–529. https://doi.org/10.1111/joim.12752.
Medeiros de Oliveira S, Alcantara Sousa L, Gadelha M, Nascimento VB. Prevention actions of burnout syndrome in nurses: an integrating literature review. Clin Pract Epidemiol Ment Health. 2019;15:64–73. https://doi.org/10.2174/1745017901915010064.
Alan H. Rosenstein. Hospital administration response to physician stress and burnout. Hospital Practice. 2019;47(5):217–20. https://doi.org/10.1080/21548331.2019.1688596.
Ashraf F, Ahmad H, Shakeel M, Aftab S, Masood A. Mental health problems and psychological burnout in Medical Health Practitioners: a study of associations and triadic comorbidity. Pak J Med Sci. 2019;35(6):1558–64. https://doi.org/10.12669/pjms.35.6.444.
Ovchinnikov YV, Palchenkova MV, Kalachev OV. Burnout syndrome: diagnosis, principles of treatment, prophylaxis. Voen Med Zh. 2015;336(7):17–24.
McCormack H, MacIntyre T, O'Shea D, Herring MP, Campbell MJ. The prevalence and cause(s) of burnout among applied psychologists: a systematic review. Front Psychol. 2018;9:1897. https://doi.org/10.3389/fpsyg.2018.01897.
Panagioti M, Geraghty K, Johnson J, Zhou A, Panagopoulou E, Chew-Graham C, et al. Association between physician burnout and patient safety, professionalism, and patient satisfaction: a systematic review and meta-analysis. JAMA Intern Med. 2018;178(10):1317–30. https://doi.org/10.1001/jamainternmed.2018.3713.
De Vente M, Olff M, Van Amsterdam JG, Kamphuis JH, Emmelkamp PM. Physiological differences between burnout patients and healthy controls: blood pressure, heart rate, and cortisol responses. Occup Environ Med. 2003;60:54–61. https://doi.org/10.1136/oem.60.suppl_1.i54.
Onen Sertoz O, Tolga Binbay I, Koylu E, Noyan A, Yildirim E, Elbi MH. The role of BDNF and HPA axis in the neurobiology of burnout syndrome. Prog Neuropsychopharmacol Biol Psychiatry. 2008;32(6):1459–65. https://doi.org/10.1016/j.pnpbp.2008.05.001.
Gulen B, Serinken M, Eken C, Karcıoglu Ö, Kucukdagli OT, Kilic E, et al. Serum S100B as a surrogate biomarker in the diagnoses of burnout and depression in emergency medicine residents. Acad Emerg Med. 2016;23(7):786–9. https://doi.org/10.1111/acem.12973.
Golubnitschaja O, Costigliola V. Promoting predictive, preventive and personalised medicine in global scale: the EPMA World Congress 2011. EPMA J. 2011;2(Suppl 1):1–3. https://doi.org/10.1007/s13167-011-0106-x.
Golubnitschaja O, Costigliola V. EPMA summit 2014 under the auspices of the presidency of Italy in the EU: professional statement. EPMA J. 2015;6:4. https://doi.org/10.1186/s13167-015-0026-2.
Golubnitschaja O, Baban B, Boniolo G, et al. Medicine in the early twenty-first century: paradigm and anticipation - EPMA position paper 2016. EPMA J. 2016;7:23. https://doi.org/10.1186/s13167-016-0072-4.
Golubnitschaja O, Costigliola V, Grech G. EPMA world congress: traditional forum in predictive, preventive and personalised medicine for multi-professional consideration and consolidation. EPMA J. 2017;8(Suppl 1):S1–S54. https://doi.org/10.1007/s13167-017-0108.
Golubnitschaja O, Costigliola V. General report & recommendations in predictive, preventive and personalised medicine 2012: white paper of the European Association for Predictive, Preventive and Personalised Medicine. EPMA J. 2012;3(1):14. https://doi.org/10.1186/1878-5085-3-14.
Yalom I, Leszcz M. Tratat de psihoterapie de grup. Editura Trei, Romania, București; 2008, ISBN 978-973-707-213-9.
Sexton JB, Adair KC, Leonard MW, et al. Providing feedback following leadership WalkRounds is associated with better patient safety culture, higher employee engagement and lower burnout. BMJ Qual Saf. 2018;27(4):261–70. https://doi.org/10.1136/bmjqs-2016-006399.
Oflaz F, Meriç M, Yuksel Ç, Ozcan CT. Psychodrama: an innovative way of improving self-awareness of nurses. J Psychiatr Ment Health Nurs. 2011;18(7):569–75. https://doi.org/10.1111/j.1365-2850.2011.01704.x.
Özbaş AA, Tel H. The effect of a psychological empowerment program based on psychodrama on empowerment perception and burnout levels in oncologynurses: psychological empowerment in oncology nurses. Palliat Support Care. 2015;14(4):393–401. https://doi.org/10.1017/S1478951515001121.
Grigorescu S, Cazan AM, Grigorescu D, Rogozea L. Assessing professional burnout among hospital nurses using the Copenhagen Burnout Inventory. Acta Medica Transilvanica. 2018;4 ISSN 2285–7079. http://www.amtsibiu.ro/Arhiva/2018/Nr4-en/Grigorescu.pdf.
Minulescu M. Psihodiagnoza modernă -Chestionarele de personalitate. Editura Fundației România de Mâine, București; 2004, pp 122–131. ISBN 973-582-802-2.
Vrasti R. Măsurarea sănătății mentale- Scalele de evaluare a depresiei. 2008 http://www.vrasti.org/evaluarea%20depresiei.pdf. Accessed 20 Feb 2020.
Garnefski N, Kraaij V, Spinhoven P. Manualul de utilizare a chestionarului de coping cognitiv și emoțional. Editura ASCR. 2002. ISBN 978-606-8244-0307.
Patel RS, Sekhri S, Bhimanadham NN, Imran S, Hossain S. A review on strategies to manage physician burnout. Cureus. 2019;11(6):e4805. https://doi.org/10.7759/cureus.4805.
Wiederhold BK, Cipresso P, Pizzioli D, Wiederhold M, Riva G. Intervention for physician burnout: a systematic review. Open Med (Wars). 2018;13:253–63. https://doi.org/10.1515/med-2018-0039.
Koutsimani P, Montgomery A, Georganta K. The relationship between burnout, depression, and anxiety: a systematic review and meta-analysis. Front Psychol. 2019;10:284. https://doi.org/10.3389/fpsyg.2019.00284.
Beauvais AM, Özbaş AA, Wheeler K. End-of-life psychodrama: Influencing nursing students’ communication skills, attitudes, emotional intelligence and self-reflection. J Psy Nurs. 2019;10(2):103–10. https://doi.org/10.14744/phd.2019.96636.
Noben C, Smit F, Nieuwenhuijsen K, Ketelaar S, Gärtner F, Boon B, et al. Comparative cost-effectiveness of two interventions to promote work functioning by targeting mental health complaints among nurses: pragmatic cluster randomised trial. Int J Nurs Stud. 2014;51(10):1321–31. https://doi.org/10.1016/j.ijnurstu.2014.01.017.
Noben C, Evers S, Nieuwenhuijsen K, Ketelaar S, Gärtner F, Sluiter J, et al. Protecting and promoting mental health of nurses in the hospital setting: is it cost-effective from an employer’s perspective? Int J Occup Med Environ Health. 2015;28(5):891–900. https://doi.org/10.13075/ijomeh.1896.00465.
Bretland RJ, Thorsteinsson EB. Reducing workplace burnout: the relative benefits of cardiovascular and resistance exercise. PeerJ. 2015;3:e891. https://doi.org/10.7717/peerj.891.
Han S, Shanafelt TD, Sinsky CA, Awad KM, Dyrbye LN, Fiscus LC, et al. Estimating the attributable cost of physician burnout in the United States. Ann Intern Med. 2019;170(11):784–90. https://doi.org/10.7326/M18-1422.
Lui JNM, Andres EB, Johnston JM. Presenteeism exposures and outcomes amongst hospital doctors and nurses: a systematic review. BMC Health Serv Res. 2018;18(1):985. https://doi.org/10.1186/s12913-018-3789-z.
Fiorilli C, Benevene P, De Stasio S, Buonomo I, Romano L, Alessandro P, et al. Teachers’ burnout: the role of trait emotional intelligence and social support. Front Psychol. 2019;10 https://www.frontiersin.org/articles/10.3389/fpsyg.2019.02743/full. Accessed 25 Feb 2020.
Kim B, Jee S, Lee J, An S, Lee SM. Relationships between social support and student burnout: a meta-analytic approach. Stress Health. 2018;34:127–34. https://doi.org/10.1002/smi.2771.
Ben-Zur H, Michael K. Burnout, social support, and coping at work among social workers, psychologists, and nurses. Soc Work Health Care. 2007;45(4):63–8.
Arrogante Maroto Ó, Aparicio-Zaldívar EG. Tools to face burnout in nursing: social support, resilience and coping strategies. Rev Enferm. 2017;40(3):10–7.
Li L, Ai H, Gao L, Zhou H, Liu X, Zhang Z, et al. Moderating effects of coping on work stress and job performance for nurses in tertiary hospitals: a cross-sectional survey in China. BMC Health Serv Res. 2017;17:401. https://doi.org/10.1186/s12913-017-2348-3.
Acknowledgements
We acknowledge that the development of the research was authorized by the nurses who participated in this study and the research team would like to thank the management team of the Emergency County Hospital Brasov for their cooperation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest. All authors approve the content of the manuscript and have contributed significantly to the research and the writing of the manuscript.
Ethical approval
The research did not involve any risk for the participants. All ethical guidelines were followed as required for conducting human research. The procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional research, the study being approved to be run by the manager of the Emergency County Hospital Brasov, where the study was conducted and by the Committee for Ethical Research of Transylvania University of Brasov (Ethical approval number 06.2/2017). The research was also consistent with the ethical guidelines of The College of Psychologists in Romania. The research complies with the provisions of the Declaration of Helsinki (as revised in Brazil 2013). All the participants gave their informed consent for the research and their anonymity was preserved.
Authorship statement
The authors certify their contribution to this manuscript, as follows: study design (SG, LMR); data collection (SG, ODG) and analysis (SG, AMC); manuscript writing (SG, ODG, AMC).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Grigorescu, S., Cazan, AM., Rogozea, L. et al. Original targeted therapy for the management of the burnout syndrome in nurses: an innovative approach and a new opportunity in the context of predictive, preventive and personalized medicine. EPMA Journal 11, 161–176 (2020). https://doi.org/10.1007/s13167-020-00201-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13167-020-00201-6