Abstract
Aim and background
Colon and rectum (colorectal) cancer cause substantial mortality and morbidity worldwide. The management and control of a complex disease such as cancer cannot rely on the old strategy of “one disease one medicine” and must make a transition into new-age practices involving predictive, preventive, and personalized medicine (PPPM) at its core. Adoption of PPPM approach to cancer management at the policy level requires quantification of cancer burden at the country level. For this purpose, we examine the burden of colorectal cancer in 185 countries in 2018. Based on results, we discuss the opportunities presented by PPPM and challenges to be encountered while adopting PPPM for the treatment and prevention of colorectal cancer.
Data and methods
Age- and sex-wise estimates of colorectal cancer were procured from the GLOBOCAN 2018. The country- and region-wise burden of colorectal cancer in 185 countries was examined using all-age and age-standardized incidence and mortality estimates. Human development index (HDI) was employed as the indicator of socioeconomic status of a country. Mortality-to-incidence ratio (MIR) was employed as the proxy of 5-year survival rate.
Results
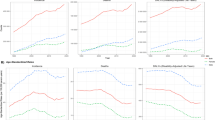
Globally, colorectal cancer claimed an estimated 880,792 lives (males 484,224; females 396,568) with 1.85 million new cases (males 1.03 million; females 823,303) were estimated to be diagnosed in 2018. Globally, the age-standardized incidence rate (ASIR) was 19.7/100,000, whereas age-standardized mortality rate (ASMR) recorded to be 16.3/100,000 in 2018. Age-standardized rates were the highest in developed countries led by Hungary with ASIR of 51.2/100,000 followed by South Korea with ASIR of 44.5/100,000. ASMR followed the patterns of ASIR with the highest ASMR recorded by Hungary (21.5 per 100,000) and Slovakia (20.4 per 100,000). Globally, MIR stood at 0.48, and among the countries recording more than 1000 cases, Nepal registered the highest MIR of 0.83 and the lowest was recorded by South Korea (0.27). The age-standardized rates exhibited nonlinear association with HDI, whereas MIR was negatively associated with HDI.
Conclusion
Colorectal cancer causes a substantial burden worldwide and exhibit a positive association with the socioeconomic status. With the aid of improving screening modalities, preventable nature of the disease (due to dietary and lifestyle risk factors) and improving treatment procedures, the burden of CRC can largely be curtailed. The high burden of CRC in developing countries, therefore, calls for effective prevention strategies, cost-effective screening, and early-stage detection, cost-effective predictive, and personalized treatment regime.



Similar content being viewed by others
Notes
UNDP defines mean number of years of schooling as the number of years of schooling received by people ages 25 and older, and expected years of schooling s defined as number of years of schooling that a child of school entrance age can expect to receive if prevailing patterns of age-specific enrolment rates persist throughout life [12].
US Preventive Services Task Force (US PSTF) recommends the use of low-dose aspirin for the prevention of colorectal cancer in high-risk patients [45].
References
Roth GA, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1736–88.
Fitzmaurice C, Akinyemiju TF, Al Lami FH, Alam T, Alizadeh-Navaei R, Allen C, et al. Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 29 cancer groups, 1990 to 2016: a systematic analysis for the global burden of disease study. JAMA Oncol. 2018;4:1553–68.
Sung JJ, Lau JY, Goh KL, Leung WK. Increasing incidence of colorectal cancer in Asia: implications for screening. Lancet Oncol. 2005;6:871–6.
Allemani C, Matsuda T, Di Carlo V, Harewood R, Matz M, Nikšić M. Global surveillance of trends in cancer survival 2000–14 (CONCORD-3): analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet. 2018;391:1023–75.
Hamilton SR, Bosman FT, Boffetta P, et al. Carcinoma of the colon and rectum. In: In Bosman FT, Carneiro F, Hruban RH, Theise ND, editors. WHO classification of tumours of the digestive system. Lyon: IARC Press; 2010. p. 134–46.
Taylor DP, Burt RW, Williams MS, Haug PJ, Cannon–Albright LA. Population-based family history–specific risks for colorectal cancer: a constellation approach. Gastroenterology. 2010;138:877–885.
Bibbins-Domingo K, Grossman DC, Curry SJ, Davidson KW, Epling JW, García FA, et al. Screening for colorectal cancer: US Preventive Services Task Force recommendation statement. JAMA. 2016;315:2564–75.
Grech G, Zhan X, Yoo BC, Bubnov R, Hagan S, Danesi R, et al. EPMA position paper in cancer: current overview and future perspectives. EPMA J. 2015;6:9.
Golubnitschaja O, Baban B, Boniolo G, Wang W, Bubnov R, Kapalla M, et al. Medicine in the early twenty-first century: paradigm and anticipation - EPMA position paper 2016. EPMA J. 2016;7:23.
Janssens JP, Schuster K, Voss A. Preventive, predictive, and personalized medicine for effective and affordable cancer care. EPMA J. 2018;9:113–23.
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424.
UNDP (2018). Human Development Indices and Indicators 2018 Statistical Update. Available at http://hdr.undp.org/sites/default/files/2018_human_development_statistical_update.pdf (Accessed: 3.5.2019).
Vostakolaei F, Karim-Kos HE, Janssen-Heijnen ML, Visser O, Verbeek AL, Kiemeney LA. The validity of the mortality to incidence ratio as a proxy for site-specific cancer survival. Eur J Pub Health. 2010;21:573–7.
Sunkara V, Hebert JR. The colorectal cancer mortality-to-incidence ratio as an indicator of global cancer screening and care. Cancer. 2015;121:1563–9.
Sharma R. Breast cancer incidence, mortality and mortality-to-incidence ratio (MIR) are associated with human development, 1990–2016: evidence from Global Burden of Disease Study 2016. Breast Cancer. 2019a;26:428–45.
Sharma R. The burden of prostate cancer is associated with human development index: evidence from 87 countries, 1990–2016. EPMA J. 2019b;10:137–52.
Ferlay J, Colombet M, Soerjomataram I, Mathers C, Parkin DM, Piñeros M, et al. Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int J Cancer. 2019;144:1941–53.
Ferlay J, Ervik M, Lam F, Colombet M, Mery L, Piñeros M et al (2018). Global Cancer Observatory. Lyon, France: International Agency for Research on Cancer. Available from: https://gco.iarc.fr/, accessed [01.05.2019].
Human Development Database: http://hdr.undp.org/en/data# (Accessed: 3.5.2019).
Arnold M, Sierra MS, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global patterns and trends in colorectal cancer incidence and mortality. Gut. 2017;66:683–91.
Haggar FA, Boushey RP. Colorectal cancer epidemiology: incidence, mortality, survival, and risk factors. Clin Colon Rectal Surg. 2009;22:191–7.
Devesa SS, Chow WH. Variation in colorectal cancer incidence in the United States by subsite of origin. Cancer. 1993;71:3819–26.
Cheng X, Chen VW, Steele B, Ruiz B, Fulton J, Liu L, et al. Subsite-specific incidence rate and stage of disease in colorectal cancer by race, gender, and age group in the United States, 1992–1997. Cancer. 2001;92:2547–54.
Murphy G, Devesa SS, Cross AJ, Inskip PD, McGlynn KA, Cook MB. Sex disparities in colorectal cancer incidence by anatomic subsite, race and age. Int J Cancer. 2011;128:1668–75.
Atkin WS, Edwards R, Kralj-Hans I, Wooldrage K, Hart AR, Northover JM, et al. Once-only flexible sigmoidoscopy screening in prevention of colorectal cancer: a multicentre randomised controlled trial. Lancet. 2010;375:1624–33.
Segnan N, Armaroli P, Bonelli L, Risio M, Sciallero S, Zappa M, et al. Once-only sigmoidoscopy in colorectal cancer screening: follow-up findings of the Italian Randomized Controlled Trial—SCORE. J Natl Cancer Inst. 2011;103:1310–22.
Schoen RE, Pinsky PF, Weissfeld JL, Yokochi LA, Church T, Laiyemo AO, et al. Colorectal-cancer incidence and mortality with screening flexible sigmoidoscopy. N Engl J Med. 2012;366:2345–57.
Holme Ø, Bretthauer M, Fretheim A, Odgaard-Jensen J, Hoff G. Flexible sigmoidoscopy versus faecal occult blood testing for colorectal cancer screening in asymptomatic individuals. Cochrane Database Syst Rev. 2013;9:CD0009259
Holme Ø, Løberg M, Kalager M, Bretthauer M, Hernán MA, Aas E, et al. Effect of flexible sigmoidoscopy screening on colorectal cancer incidence and mortality: a randomized clinical trial. JAMA. 2014;312:606–15.
Schreuders EH, Ruco A, Rabeneck L, Schoen RE, Sung JJ, Young GP, et al. Colorectal cancer screening: a global overview of existing programmes. Gut. 2015;64:1637–49.
Shapiro JA, Klabunde CN, Thompson TD, Nadel MR, Seeff LC, White A. Patterns of colorectal cancer test use, including CT colonography, in the 2010 National Health Interview Survey. Cancer Epidemiol Biomark Prev. 2012;21:895–904.
Decker KM, Singh H. Reducing inequalities in colorectal cancer screening in North America. J Carcinog. 2014;13:12.
Fedirko V, Tramacere I, Bagnardi V, Rota M, Scotti L, Islami F. Alcohol drinking and colorectal cancer risk: an overall and dose–response meta-analysis of published studies. Ann Oncol. 2011;22:1958–72.
Botteri E, Iodice S, Bagnardi V, Raimondi S, Lowenfels AB, Maisonneuve P. Smoking and colorectal cancer: a meta-analysis. JAMA. 2008;300:2765–78.
Demeyer D, Mertens B, De Smet S, Ulens M. Mechanisms linking colorectal cancer to the consumption of (processed) red meat: a review. Crit Rev Food Sci Nutr. 2016;56:2747–66.
Bardou M, Barkun AN, Martel M. Obesity and colorectal cancer. Gut. 2013;62:933–47.
Moghaddam AA, Woodward M, Huxley R. Obesity and risk of colorectal cancer: a meta-analysis of 31 studies with 70,000 events. Cancer Epidemiol Biomark Prev. 2007;16:2533–47.
Peeters PJ, Bazelier MT, Leufkens HG, de Vries F, De Bruin ML. The risk of colorectal cancer in patients with type 2 diabetes: associations with treatment stage and obesity. Diabetes Care. 2015;38:495–502.
Terry P, Giovannucci E, Michels KB, Bergkvist L, Hansen H, Holmberg L, et al. Fruit, vegetables, dietary fiber, and risk of colorectal cancer. J Natl Cancer Inst. 2001;93:525–33.
Van Duijnhoven FJ, Bueno-De-Mesquita HB, Ferrari P, Jenab M, Boshuizen HC, Ros MM, et al. Fruit, vegetables, and colorectal cancer risk: the European Prospective Investigation into Cancer and Nutrition. Am J Clin Nutr. 2009;89:1441–52.
Huxley RR, Ansary-Moghaddam A, Clifton P, Czernichow S, Parr CL, Woodward M. The impact of dietary and lifestyle risk factors on risk of colorectal cancer: a quantitative overview of the epidemiological evidence. Int J Cancer. 2009;125:171–80.
Rothwell PM, Wilson M, Elwin CE, Norrving B, Algra A, Warlow CP, et al. Long-term effect of aspirin on colorectal cancer incidence and mortality: 20-year follow-up of five randomised trials. Lancet. 2010;376:1741–50.
Rothwell PM, Fowkes FG, Belch JF, Ogawa H, Warlow CP, Meade TW. Effect of daily aspirin on long-term risk of death due to cancer: analysis of individual patient data from randomised trials. Lancet. 2011;377:31–41.
Burn J, Gerdes AM, Macrae F, Mecklin JP, Moeslein G, Olschwang S, et al. Long-term effect of aspirin on cancer risk in carriers of hereditary colorectal cancer: an analysis from the CAPP2 randomised controlled trial. Lancet. 2011;378:2081–7.
Chubak J, Kamineni A, Buist DSM, Anderson ML & Whitlock EP (2015) Aspirin use for the prevention of colorectal cancer: an updated systematic evidence review for the U.S. Preventive Services Task Force (Agency for Healthcare Research and Quality (US), 2015).
Gonzalez CA, Riboli E. Diet and cancer prevention: contributions from the European Prospective Investigation into Cancer and Nutrition (EPIC) study. Eur J Cancer. 2010;46:2555–62.
Thirunavukarasu P, Sukumar S, Sathaiah M, Mahan M, Pragatheeshwar KD, Pingpank JF, et al. C-stage in colon cancer: implications of carcinoembryonic antigen biomarker in staging, prognosis, and management. J Natl Cancer Inst. 2011;103:689–97.
Nikolaou S, Qiu S, Fiorentino F, Rasheed S, Tekkis P, Kontovounisios C. The prognostic and therapeutic role of hormones in colorectal cancer: a review. Mol Biol Rep. 2019:461477–86.
Sullivan R, Alatise OI, Anderson BO, Audisio R, Autier P, Aggarwal A, et al. Global cancer surgery: delivering safe, affordable, and timely cancer surgery. Lancet Oncol. 2015;16:1193–224.
Lu M, Zhan X. The crucial role of multiomic approach in cancer research and clinically relevant outcomes. EPMA J. 2018;9:77–102.
Horgan RP, Kenny LC. ‘Omic’ technologies: genomics, transcriptomics, proteomics and metabolomics. Obstet Gynaecol. 2011;13:189–95.
Golubnitschaja O, Kinkorova J, Costigliola V. Predictive, preventive and personalized medicine as the hardcore of ‘Horizon 2020’: EPMA position paper. EPMA J. 2014;5:6.
Acknowledgments
The authors thank the International Agency for Research on Cancer (IARC) for making available GLOBOCAN 2018 estimates in the public domain.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The research is conducted using data available in the public domain and does not include any human participants and/or animals.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Sharma, R. An examination of colorectal cancer burden by socioeconomic status: evidence from GLOBOCAN 2018. EPMA Journal 11, 95–117 (2020). https://doi.org/10.1007/s13167-019-00185-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13167-019-00185-y