Abstract
A major opportunity in nuclear cardiology is the many significant artificial intelligence (AI) applications that have recently been reported. These developments include using deep learning (DL) for reducing the needed injected dose and acquisition time in perfusion acquisitions also due to DL improvements in image reconstruction and filtering, SPECT attenuation correction using DL without need for transmission images, DL and machine learning (ML) use for feature extraction to define myocardial left ventricular (LV) borders for functional measurements and improved detection of the LV valve plane and AI, ML, and DL implementations for MPI diagnosis, prognosis, and structured reporting. Although some have, most of these applications have yet to make it to widespread commercial distribution due to the recency of their developments, most reported in 2020. We must be prepared both technically and socio-economically to fully benefit from these and a tsunami of other AI applications that are coming.


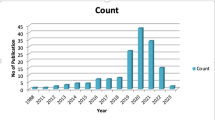
adapted from slide courtesy of MA King and AJ Ramon



adapted from LeCun et al. [33]

Similar content being viewed by others
References
Salerno M, Beller GA. Noninvasive assessment of myocardial perfusion. Circ Cardiovasc Imaging. 2009;2:412–24.
Einstein AJ, Pascual TNB, Mercuri M, Karthikeyan G, Vitola JV, Mahmarian JJ, et al. Current worldwide nuclear cardiology practices and radiation exposure: results from the 65 country IAEA Nuclear Cardiology Protocols Cross-Sectional Study (INCAPS). Eur Heart J. 2015;36:1689–96.
Slomka P, Xu Y, Berman D, Germano G. Quantitative analysis of perfusion studies: strengths and pitfalls. J Nucl Cardiol. 2012;19:338–46.
Nuclear Medicine Market Outlook Report 2018. Accessed on 12/30/2020. Available from: https://imvinfo.com/product/nuclear-medicine-market-outlook-report-2018/
Schindler T, Schelbert HR, Quercioli A, Dilsizian V. Cardiac PET for the detection and monitoring of coronary artery disease and microvascular health. JACC Cardiovasc Imag. 2010;3:623–40.
Al Badarin FJ, Malhotra S. Diagnosis and prognosis of coronary artery disease with SPECT and PET. Curr Cardiol Rep. 2019;21:57.
Garcia E, Slomka P, Moody JB, Germano G, Ficaro EP. Quantitative clinical nuclear cardiology, Part 1: established applications. J Nucl Med. 2019;60:1507–16.
Slomka PJ, Moody JB, Miller RJ, et al. Quantitative clinical nuclear cardiology, Part 2: evolving/emerging applications. J Nucl Med. 2020. https://doi.org/10.2967/jnumed.120.242537. Online ahead of print.
Motwani M, Berman DS, Germano G, Slomka PJ. Automated quantitative nuclear cardiology methods. Cardiol Clin. 2016;34:47–57.
Garcia EV, Klein JL, Moncayo V, Cooke CD, Del’Aune C, Folks R, et al. Diagnostic performance of an artificial intelligence-driven cardiac-structured reporting system for myocardial perfusion SPECT imaging. J Nucl Cardiol. 2020;27:1652–64.
Garcia EV: Deep learning, another important tool for improving acquisition efficiency in SPECT MPI Imaging. (Editorial) J Nucl Cardiol. 2020. https://doi.org/10.1007/s12350-020-02188-z
Shiri I, Sabet KA, Arabi H, Pourkeshavarz M, Teimourian B, Ay MR, et al. Standard SPECT myocardial perfusion estimation from half-time acquisitions using deep convolutional residual neural networks. J Nucl Cardiol. 2020. https://doi.org/10.1007/s12350-020-02119-y. Online ahead of print.
Ramon AJ, Yang Y, Pretorius PH, Johnson KL, King MA, Wernick MN. Improving diagnostic accuracy in low-dose SPECT myocardial perfusion imaging with convolution denoising networks. IEEE Trans Med Imaging. 2020;39:2893–903.
Song C, Yang Y, Wernick MN, Pretorius PH, King MA. Low-dose cardiac-gated SPECT studies using a residual convolutional neural network. 2019 IEEE 16th International Symposium on Biomedical Imaging (ISBI 2019), 2019, 653–656.
Hu LH, Miller RJH, Sharir T, Commandeur F, Rios R, Einstein AJ, et al. Prognostically safe stress-only single-photon emission computed tomography myocardial perfusion imaging guided by machine learning: report from REFINE SPECT. Eur Heart J Cardiovasc Imaging. 2020; 00–1–10.
Shi L, Onofrey JA, Liu H, Liu YH, Liu C. Deep learning-based attenuation map generation for myocardial perfusion SPECT. Eur J Nucl Med Mol Imag. 2020;47:2383–95.
Gomez J, Doukky R, Germano G, Slomka P. New trends in quantitative nuclear cardiology methods. Curr Cardiovasc Imaging Rep. 2018;11:1. https://doi.org/10.1007/s12410-018-9443-7.
Xu Y, Kavanaugh PB, Fish MB, Gerlach J, Ramesh A, Lemley M, et al. Automated quality control for segmentation of myocardial perfusion. J Nucl Med. 2009;50:1418–26.
Betancur J, Rubeaux M, Fuchs TA, Otaki Y, Arnson Y, Slipczuk L, et al. Automatic valve plane localization in myocardial perfusion SPECT/CT by machine learning: anatomic and clinical validations. J Nucl Med. 2017;58:961–7.
Wang T, Lei Y, Tang H, He Z, Castillo R, Wang C, et al. A learning-based automatic segmentation and quantification method of left ventricle in gated myocardial perfusion SPECT imaging: a feasibility study. J Nucl Cardiol. 2020;27:976–87.
Fujita H, Katafuchi T, Uehara T, Nishimura T. Application of neural network to computer-aided diagnosis of coronary artery disease in myocardial SPECT bull’s eye images. J Nucl Med. 1992;33:272–6.
Porenta G, Dorffner G, Kundrat S, Petta P, Duit-Schedlmayer J, Sochor H. Automated interpretation of planar thallium-201-dipyridamole stress-redistribution scintigrams using artificial neural networks. J Nucl Med. 1994;35:2041–7.
Hamilton D, Riley PJ, Miola UJ, Amro AA. A feed-forward neural network for classification of bull’s eye myocardial perfusion images. Eur J Nucl Med. 1995;22:108–15.
Lindhal D, Palmer J, Ohlsson M, Peterson C, Lundlin A, Edenbrandt. Automated interpretation of myocardial SPECT perfusion images using artificial neural networks. J Nucl Med. 1997;38:1870–5.
Lindhal D, Palmer J, Edenbrandt L. Myocardial SPECT: artificial neural networks describe extent and severity of perfusion defects. Clin Physiol. 1999;19:497–503.
Lindhal D, Toft J, Hesse B, Palmer J, Ali S, Lundin A, et al. Scandinavian test of artificial neural network for classification of myocardial perfusion images. Clin Physiol. 2000;20:253–61.
Allison JS, Heo J, Iskandrian AE. Artificial neural network modeling of stress single-photon emission computed tomographic imaging for detecting extensive coronary artery disease. Am J Cardiol. 2005;95:178–81.
Arsanjani R, Xu Y, Dey D, Fish M, Dorbala S, Hayes S, et al. Improved accuracy of myocardial perfusion SPECT for the detection of coronary artery disease using a support vector machine algorithm. J Nucl Med. 2013;54:549–55.
Arsanjani R, Xu Y, Dey D, Vahistha V, Shalev A, Nakanishi R, et al. Improved accuracy of myocardial perfusion SPECT for detection of coronary artery disease by machine learning in a large population. J Nucl Cardiol. 2013;20:553–62.
Arsanjani R, Dey D, Khachatryan T, Shalev A, Hayes SW, Fish M, et al. Prediction of revascularization after myocardial perfusion SPECT by machine learning in a large population. J Nucl Cardiol. 2015;22:877–84.
Hu LH, Betancur J, Sharir T, Einstein AJ, Bokhari S, Fish MB, et al. Machine learning predicts per-vessel early coronary revascularization after fast myocardial perfusion SPECT: results from multicenter REFINE SPECT registry. Eur Heart J Cardiovasc Imaging. 2020;12:549–59.
Betancur J, Commandeur F, Motlagh M, Sharir T, Einstein AJ, Bokhari S, et al. Deep learning for prediction of obstructive disease from fast myocardial perfusion SPECT: a multicenter study. JACC Cardiovasc Imaging. 2018;11:1654–63.
LeCun Y, Bengio Y, Hinton G. Deep Learning. Nature. 2015;521:436–44.
Betancur J, Hu LH, Commandeur F, Sharir T, Einstein AJ, Fish MB, et al. Deep learning analysis of upright-supine high-efficiency SPECT myocardial perfusion imaging for prediction of coronary artery disease: a multicenter study. J Nucl Med. 2019;60:664–70.
Betancur J, Otaki Y, Motwani M, Fish MB, Lemley M, Dey D, et al. Prognostic value of combined clinical and myocardial perfusion imaging data using machine learning. JACC Cardiovasc Imaging. 2018;11:1000–9.
Juarez-Orozco LE, Knol RJJ, Sanches-Catasus CA, Martinez-Manzanera O, van der Zant FM, Knuuti J. Machine learning in the integration of simple variables for identifying patients with myocardial ischemia. J Nucl Cardiol. 2020;27:147–55.
Alonso DH, Wernick MN, Yang Y, Germano G, Berman DS, Slomka P. Prediction of cardiac death after adenosine myocardial perfusion SPECT based on machine learning. J Nucl Cardiol. 2019;26:1746–54.
Sung J, Stewart CL, Freedman B. Artificial intelligence in health care: preparing for the fifth Industrial Revolution. MJA 213(6), 2020. https://doi.org/10.5694/mja2.50755
Ornstein C, Thomas K. Sloan Kettering’s cozy deal with start-up ignites a new uproar. New York Times. https://www.nytimes.com/2018/09/20/ health/memorial-sloan-kettering-cancer-paige-ai.html. Published September 20, 2018. Accessed May 5, 2021.
Larson DB, Magnus DC, Lungren MP, Shah NH, Langlotz CP. Ethics of using and sharing clinical imaging data for artificial intelligence: a proposed framework. Radiology. 2020;295:675–82.
Copeland R. Google’s ‘Project Nightingale’ gathers personal health data on millions of Americans. Wall Street Journal. https://www.wsj.com/articles/ google-s-secret-project-nightingale-gathers-personal-health-data-on-millionsof-americans-11573496790?mod=article_inline. Published November 11, 2019. Accessed May 5, 2021.
Artificial Intelligence/Machine Learning (AI/ML)-Based software as a medical device (SaMD) Action Plan (2021) https://www.fda.gov/media/145022/download Accessed May 5, 2021
Proposed regulatory framework for modifications to artificial intelligence/machine learning (AI/ML)-based software as a medical device (SaMD) - discussion paper and request for feedback. (2019) https://www.fda.gov/media/122535/download Accessed May 5, 2021
Skloot R. The Immortal Life of Henrietta Lacks. New York: Penguin Random House; 2010.
Tobia K, Nielsen A, Stremitzer S. When does physician use of AI increase liability? J Nucl Med. 2021;62:17–21. https://doi.org/10.2967/jnumed.120.256032.
Faden RR, Kass NE, Goodman SN, Pronovost P, Tunis S, Beauchamp TL. An ethics framework for a learning health care system: a departure from traditional research ethics and clinical ethics. Hastings Cent Rep. 2013;43(Spec No):S16–27.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Ernest Garcia receives royalties from the sale of the Emory Cardiac Toolbox and has equity positions with Syntermed, Inc. The terms of these arrangements have been reviewed and approved by Emory University in accordance with its conflict of interest policies. Marina Piccinelli reports no conflict of interest.
Ethics Approval
For this review, ethical approval is not required.
Informed Consent
For this review, consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Garcia, E.V., Piccinelli, M. Preparing for the Artificial Intelligence Revolution in Nuclear Cardiology. Nucl Med Mol Imaging 57, 51–60 (2023). https://doi.org/10.1007/s13139-021-00733-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13139-021-00733-3