Abstract
Purpose
The COVID-19 pandemic created conditions of scarcity that led many provinces within Canada to develop triage protocols for critical care resources. In this study, we sought to undertake a narrative synthesis and ethical analysis of early provincial pandemic triage protocols.
Methods
We collected provincial triage protocols through personal correspondence with academic and political stakeholders between June and August 2020. Protocol data were extracted independently by two researchers and compared for accuracy and agreement. We separated data into three categories for comparative content analysis: protocol development, ethical framework, and protocol content. Our ethical analysis was informed by a procedural justice framework.
Results
We obtained a total of eight provincial triage protocols. Protocols were similar in content, although age, physiologic scores, and functional status were variably incorporated. Most protocols were developed through a multidisciplinary, expert-driven, consensus process, and many were informed by influenza pandemic guidelines previously developed in Ontario. All protocols employed tiered morality-focused exclusion criteria to determine scarce resource allocation at the level of regional health care systems. None included a public engagement phase, although targeted consultation with public advocacy groups and relevant stakeholders was undertaken in select provinces. Most protocols were not publicly available in 2020.
Conclusions
Early provincial COVID-19 triage protocols were developed by dedicated expert committees under challenging circumstances. Nonetheless, few were publicly available, and public consultation was limited. No protocols were ever implemented, including during periods of extreme critical care surge. A national approach to pandemic triage that incorporates additional aspects of procedural justice should be considered in preparation for future pandemics.
Résumé
Objectif
La pandémie de COVID-19 a créé des conditions de pénurie qui ont amené de nombreuses provinces canadiennes à élaborer des protocoles de triage pour l’allocation des ressources en soins intensifs. Dans le cadre de cette étude, nous avons cherché à réaliser une synthèse narrative et une analyse éthique des premiers protocoles provinciaux de triage lors de la pandémie.
Méthode
Nous avons recueilli les protocoles de triage provinciaux en correspondant de façon personnelle avec des intervenant·es universitaires et politiques entre juin et août 2020. Les données des protocoles ont été extraites indépendamment par deux personnes de l’équipe de recherche et comparées pour en vérifier l’exactitude et la concordance. Nous avons séparé les données en trois catégories pour l’analyse comparative du contenu : l’élaboration d’un protocole, le cadre éthique et le contenu du protocole. Notre analyse éthique s’est appuyée sur un cadre de justice procédurale.
Résultats
Nous avons obtenu un total de huit protocoles de triage provinciaux. Les protocoles étaient similaires dans leur contenu, bien que l’âge, les scores physiologiques et l’état fonctionnel aient été incorporés de manière variable. La plupart des protocoles ont été élaborés dans le cadre d’un processus consensuel multidisciplinaire dirigé par des expert·es, et bon nombre d’entre eux ont été élaborés en fonction des lignes directrices sur la pandémie de grippe élaborées antérieurement en Ontario. Tous les protocoles utilisaient des critères d’exclusion à plusieurs niveaux axés sur la moralité pour déterminer l’affectation de ressources limitées au niveau des systèmes de soins de santé régionaux. Aucun ne comportait de phase de mobilisation du public, bien que des consultations ciblées aient été menées auprès des groupes de défense des droits du public et des instances concernées dans certaines provinces. La plupart des protocoles n’étaient pas accessibles au public en 2020.
Conclusion
Les premiers protocoles provinciaux de triage pour la COVID-19 ont été élaborés par des comités spécialisés d’expert·es dans des circonstances difficiles. Néanmoins, peu d’entre eux étaient accessibles au public et la consultation publique était limitée. Aucun protocole n’a été mis en œuvre, même pendant les périodes de pointe extrême en soins intensifs. Une approche nationale du triage en cas de pandémie qui intègre d’autres aspects de justice procédurale devrait être envisagée en prévision de futures pandémies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The COVID-19 pandemic placed a significant burden on health care systems worldwide. Concerns regarding intensive care unit (ICU) capacity and inadequate supply of life-sustaining resources such as ventilators led many governments and institutions to develop guidelines and protocols for pandemic triage and scarce resource allocation.1,2 The underlying ethical principles and content of these documents, as well as stakeholder involvement, have varied significantly across regions and countries.3,4 At present, there is no universal consensus on the most ethical or medically appropriate way to allocate scarce medical resources in a pandemic.5 Nonetheless, most organizations and experts agree that triage of scarce medical resources should occur in a rational, protocolized way to maintain fairness, transparency, and accountability.6,7,8
In Canada, where health care resource allocation is under provincial jurisdiction, provinces were responsible for developing their own COVID-19 pandemic triage plans. While this approach allows for regional autonomy in priority-setting, it also has the potential to conflict with the principle of universality inherent in the Canada Health Act by hypothetically denying services to a patient in one province that they would receive in another with a different triage protocol.6,7,8,9 Moreover, it remains unclear how the development of these protocols, stakeholder involvement, and guiding ethical principles varied from province to province.
The aims of this study were twofold. The first aim was to undertake a narrative synthesis and comparative content analysis of early written provincial COVID-19 pandemic triage protocols for the allocation of ICU resources. The second aim was to provide an ethical commentary on the processes of triage protocol development and implementation, with a focus on procedural justice. Importantly, we wish to acknowledge the significant effort put forth by individuals involved in triage protocol development across Canada in the early days of the pandemic under politically and emotionally charged circumstances. Our hope is that our retrospective analysis will help clinicians, policy makers, and the public better understand regional variation in priorities and constraints and contribute to a national discussion on how best to allocate scarce life-saving resources in future public health crises.
Methods
We obtained provincial protocols by contacting the provincial health bodies, as well as relevant academic and political stakeholders for each province, by e-mail between June and August 2020. We identified stakeholders through government and health authority websites and personal communication within the Canadian critical care community. An abbreviated search was subsequently conducted for updated, publicly available protocols in December 2022. We used the results of this search to inform the final analysis. Given the sensitive nature of these documents and the fact that permission was not obtained to share restricted or draft protocols publicly, we did not identify individual protocols by province except in the case of subsequent publication.
Once protocols were obtained, two researchers independently extracted data using Microsoft® Excel 2020 (Microsoft Corporation, Redmond, WA, USA)10 and then compared these data for accuracy and agreement. Our approach to narrative synthesis was drawn from the method described by Popay et al.11 We sorted and summarized triage protocols using a matrix and then examined relationships between protocols using directive content analysis of textual data through systematic classification (i.e., coding) and identification of themes or patterns.12,13 We separated data of interest into three categories: protocol development, ethical framework, and content. Protocol development data included protocol authorship, degree of public consultation, and public availability. Data on ethical framework included both guiding and rejected ethical principles. Content data included criteria used to determine priority for treatment, as well as responsibility for initiating, conducting, and overseeing triage.
We situated our ethical analysis within a distributive and procedural justice framework, guided by the work of the health ethicist and philosopher Norman Daniels and in particular, his arguments on “accountability for reasonableness” and fair procedures for setting allocation priorities within health care.14,15
Results
We obtained a total of eight triage protocols from the ten provinces and three territories in Canada (Table 1). As of September 2020, three protocols were publicly available and found through an internet search. We obtained five by formal e-mail request. One province provided an ethical framework that did not contain patient-level criteria or a plan to operationalize scarce resource allocation. Three provinces declined to share their protocols or did not reply to email requests (British Columbia, Nova Scotia, and Prince Edward Island). One territory, Nunavut, has no critical care beds and therefore had not developed a critical care triage protocol.
Four of the eight protocols were updated between September 2020 and December 2022, following additional consultation with disability advocacy groups and representatives from other vulnerable populations, as well as legal advisors. All four were available through an internet search in December 2022. Two protocols were additionally published in peer-review format: one in September 2020 and the other in January 2022.16,17
Protocol development
Most protocols were developed by committees involving health professionals, health organization leaders, and ethicists. One committee explicitly listed involvement of a patient and family advocate in protocol development. Two additional committees described targeted public consultation through patient and disability advocacy groups on draft protocols during development. None described use of broader engagement of the lay public in protocol development or revision. All protocols appeared intended to be applied at the level of provincial or regional health care system rather than at the level of individual hospitals or local health care systems, although this was not always explicitly stated. Many committees drew inspiration from publicly available or published documents from Ontario, including the 2006 Ontario Influenza Triage Guidelines, the 2009 Hamilton Health Sciences Critical Care Triage Policy for Pandemic Influenza, and the Ontario Health Clinical Triage Protocol for Major Surge in COVID Pandemic 2020.18,19,20 Other provincial draft triage documents from the H1N1 influenza pandemic were also used as guidance. In addition, one protocol referenced the 2020 University of Pittsburgh Protocol for Allocation of Scarce Critical Care Resources.21
Ethical framework
Protocols included three types of content: overarching ethical principles, clinical criteria to guide triage decisions about individual patients, and directions for implementation of the triage process. Relevant ethical principles are defined in Table 2. All protocols adopted the ethical principles of utilitarianism and egalitarianism. Five protocols included proportionality and three included fair innings and reciprocity as additional guiding principles.22 Conversely, two protocols explicitly rejected fair innings, reciprocity, and the multiplier effect from their ethical framework. Additional guiding principles that were mentioned at least once are listed in Table 1.
Protocol content
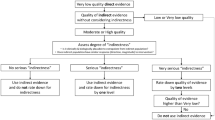
Most protocols employed a tiered mortality-focused approach to triage, wherein no patient was excluded from receiving critical care, but scare critical care resources would have been allocated based on predefined disease-specific prognostic criteria that attempted to standardize mortality estimates across various acute and chronic conditions. In six protocols, these prognostic criteria were used to stratify patients into three groups based on predicted in-hospital or short-term mortality (80%, 50%, 30%). A tiered approach to triage was then proposed based on the degree of resource scarcity: in stage 1 triage, critical care resources would not be allocated to patients with 80% predicted mortality; in stage 2, critical care resources would not be allocated to those with 50% predicted mortality; and in stage 3, the cut-off to not allocate critical care resources was 30% predicted mortality. Of the two remaining protocols, one did not specify numerical cut-offs for predicted mortality, and one only specified an 80% predicted mortality cut-off, without a more extensive tiered approach.
There was notable overlap in disease-specific clinical criteria between protocols. Most tiered mortality-focused criteria were based on the severity of pre-existing diagnoses such as chronic obstructive pulmonary disease, cancer, and dementia. Various combinations of age, functional status, and physiologic derangement according to the Sequential Organ Failure Assessment (SOFA) score23 were also used in three of the eight protocols. For patients whose predicted mortality was below the cut-offs used in the tiered mortality-focused prognostic criteria, tie-breaker criteria were then used to determine allocation of scare critical care resources. These were variable, and included first-come first-serve, a lottery system, or consideration of potential life-years lost. None of the protocols specified how a lottery system would be operationalized. Seven of eight protocols included a reassessment process that could involve withdrawal of life support from an existing ICU patient after a certain time frame had elapsed, or if advancement to the next stage of tiered triage was required. In most protocols, the stated goal of triage was maximizing short-term survival, measured in weeks to months, although two protocols used one-year survival as their benchmark.
All protocols were directed towards adult patients. Three protocols additionally included a plan for pediatric triage to be triggered at either stage 2 (two protocols) or at stage 3 (one protocol) of the adult triage process. In two of the three protocols, decisions to withhold or withdraw life support treatment (WLST) from pediatric patients would be informed by expert consensus among pediatric intensivists that predicted mortality was likely to be high. The third protocol also used the Pediatric Logistic Organ Dysfunction score to inform WLST for pediatric patients.24
Protocol implementation
In most cases, initiating the triage process was considered either the responsibility of the provincial ministry of health, the executive leadership team of a regional health authority, or a separate provincial oversight committee. In all cases, decisions to activate triage would be made based on reaching a particular level of resource scarcity, typically measured as the percentage of ICU bed capacity (either baseline or surge) occupied. Only one province would use an automatic trigger to initiate triage, based on exceeding the maximum number of critical care surge beds in the province.
All protocols employed a triage team, with or without involvement of the patient’s most responsible physician, to make frontline triage decisions. All triage decisions were intended to be overseen by a central body, removed from frontline decision-making. This central body was responsible for ensuring that triage decisions followed the prescribed procedure and for mediating clinical disagreements.
Discussion
In this comparative analysis, we found important similarities and differences between provincial triage protocols for the COVID-19 pandemic. Most protocols employed tiered mortality-focused disease-specific criteria, while age, physiologic scores, and functional status were variably incorporated. All were intended to determine allocation of scarce resources at the level of provincial or regional health care systems, although only three protocols included pediatric patients. Most protocols were developed through a multidisciplinary, expert-driven, consensus process, and many were informed by influenza pandemic guidelines previously developed in Ontario. Targeted consultation with public advocacy groups and citizen stakeholders was used to refine draft protocols in select provinces. Most protocols were not publicly available or easily accessible at the time of initial data analysis, although two protocols were subsequently published in peer-review format. Notably, no triage protocols were formally activated in Canada, including at times of substantial critical care surge.25,26
It is interesting to consider how Canadian COVID-19 triage protocols compare with others in the literature. A comparative analysis of 21 publicly available COVID-19 triage guidelines from 13 countries identified similar considerations and disagreements, including whether to use illness severity scores to prioritize patients and whether to involve the patient’s most responsible physician in triage decisions.4 In many cases, details of protocol development, including authorship, were unclear in contradiction to stated commitments to transparency and accountability. Substantial variation was also seen in early ventilator allocation guidelines within the USA, highlighting the potential for inequity within a federal system.27
Considerations of distributive justice
Fair allocation of scarce medical resources within society invokes considerations of both substantive and procedural justice.14 Much of the existing ethical debate around allocation of critical care resources in the COVID-19 pandemic has centred on issues of substantive justice, i.e., the criteria used to prioritize certain individuals for access to care. These include SOFA score, age, chronic disease, and functional impairment, which may have poor predictive accuracy for short-term survival in viral respiratory illness28,29 or unfairly and systematically disadvantage groups that have already been marginalized within society, such as people with disabilities or from racial and ethnic minority communities.30,31,32,33,34 Given that issues of substantive justice in COVID-19 triage have been widely and robustly debated, we have chosen to focus our discussion on aspects of procedural justice that we believe can be refined in preparation for the next global pandemic. These aspects are ensuring the ethical legitimacy of triage protocols and determining ethical and legal responsibility for their implementation and oversight.
Triage protocols must be transparent, accountable, and responsive
Ideally, a process to distribute scarce resources should be accepted as legitimate and fair by the members of society to whom it applies.35 Transparency, accountability, and public consultation are instrumental to legitimacy. Although some public and stakeholder consultation occurred during the COVID-19 pandemic, more can be done to enhance the transparency and accountability of triage protocols that exist within the Canadian health care system. For instance, pediatric patients, along with their caregivers and physicians, are important stakeholders for pediatric triage. Their involvement was not clearly described in existing protocols. Additionally, greater consideration should be given to including more diverse stakeholders on protocol development committees (e.g., various ages, cultural and ethnic identities, and socioeconomic strata) to minimize unrecognized entrenchment of health care system bias into triage protocols. Triage development committees should clearly indicate the roles and demographics of involved members, along with processes used for stakeholder engagement. In some cases, consultation may have been adequate, but was not clearly described in protocol documents.
Health care systems and government bodies should also develop mechanisms to involve the broader public when determining acceptable guiding principles for pandemic triage, and to make protocols publicly available for review. Otherwise, these processes may contribute to further mistrust of the health care system by historically marginalized communities. Effective models for public consultation exist.36,37 For instance, the Canadian Program of Research on Ethics in a Pandemic conducted a successful public engagement initiative following the H1N1 pandemic.37 A similar process ought to be repeated now on a national level to strengthen trust given public concerns about COVID-19 triage and to take advantage of heightened public interest in this topic.25,26 Importantly, fair and adequate public consultation does not require decision-makers to adopt all proposed criteria or to reach complete consensus. Rather, we propose that inclusion of diverse nonmedical stakeholders from committee inception, public release of draft protocols, and a deliberate and well-documented consideration of points of disagreement by the committee should be considered a good faith attempt to achieve procedural justice.
Transparency and accountability can also be enhanced through development of explicit processes for tracking and publicly reporting on triage decisions if triage becomes necessary. Processes for conducting independent review after the need for triage has been resolved are also important and should be incorporated into protocols in advance. Broad public consultation and measures to improve accountability for Canadian triage protocols should occur as soon as possible in preparation for future public health emergencies.
Legitimacy also requires protocols that are responsive and adaptive. Governments and health care systems have a duty to revise triage protocols based on updated scientific information and ethical deliberation. Otherwise, justice is threatened by ineffective and misguided allocation of resources. For instance, SOFA scores have been shown to have poor discriminative accuracy for COVID-19 mortality.28,38 Some provincial protocols were more responsive than others and rejected the use of SOFA criteria based on this evidence; however, others did not. These remaining protocols must be updated before the next respiratory pandemic.
Attempts to test triage protocols using real-world data are inherently limited by difficulties such as obtaining granular information on clinical criteria, predicting counterfactual outcomes, and accounting for situational complexity. We caution that data-driven attempts to validate triage criteria may lead to flawed conclusions that further disadvantage certain populations. Nonetheless, thoughtful research efforts can still provide useful information on inconsistencies and unforeseen challenges associated with protocol implementation.39 Governments and researchers should jointly develop methods to periodically refine triage criteria as new evidence emerges.
Triage implementation should involve automatic triggers
There is broad consensus that triage should be considered only when severe resource shortages require clinicians to make decisions that put patients at risk of poor outcomes, otherwise known as crisis standards of care.40 Premature initiation is harmful if it prevents health systems and governments from maximizing all available resources, including redistribution of patients to areas with greater capacity (load balancing) or mitigation and adaptation to provide functionally equivalent care (e.g., caring for ICU patients in the postanesthesia care unit). Conversely, delayed initiation or refusal to activate triage can also cause substantial harm. Persistent crisis standards of care may lead to unnecessary mortality through suboptimal treatment of large numbers of people. In the USA, ICU demand during the pandemic strongly correlated with increased ICU mortality. In one study, one in four deaths were potentially attributable to hospital capacity strain.41 In another, the hazard ratio for death was 1.94 (95% confidence interval, 1.46 to 2.59) when COVID-19 ICU demand was more than 75% to 100% when compared with periods of low ICU demand.42
Without formal triage protocols, frontline providers may also feel obligated to pursue ad hoc, subjective triage in an attempt to maintain some internal standard of care, because of an inaccurate perception of resource shortages or the belief that institutions have abdicated responsibility.40 Anecdotally, informal triage has been reported in both the USA and Italy.40,43 Secretive or informal triage can lead to moral distress for frontline providers or expose them to medicolegal risk.44 Biased clinician judgements may also lead to unfair and medically unnecessary withholding or withdrawal of life support based on nonevidence-based criteria.
It is difficult to determine how formal triage protocols might have impacted excess pandemic-related mortality within Canada had they been instituted.45 Nevertheless, decisions not to employ triage despite crisis standards of care deserve equal scrutiny. It is notable that no triage protocols were ever activated in Canada, including at times of substantial critical care surge. A similar phenomenon was observed in the USA. Despite widespread crisis conditions, only nine states formally declared crisis standards of care46 and implementation of ventilator triage within these states was still left to individual hospitals, none of which initiated formal triage.40 Reasons for avoiding triage are complex but may include political concerns, practical concerns about liability or logistics, or uncertainty about appropriate resource thresholds at which to authorize triage. Additionally, the psychological challenges of ethical decision-making, which include considerations of competing risk, anticipation of decision regret, and concerns about the consequences of action versus inaction, must not be underestimated.47,48,49 The fact that no provincial triage protocols were implemented, despite extensive efforts devoted to their development and the prolonged state of crisis care in many health systems, illustrates the significant political and psychological challenges involved in allocating scarce life-saving resources.
We propose that future protocols make greater use of automatic triggers to determine when to take the difficult step of initiating triage. In Canada, only one province used an automatic trigger in their protocol to determine when to initiate triage. All other protocols required a subjective decision for initiation. The use of explicit triggers is beneficial because such triggers are fully transparent and prevent political considerations from dissuading necessary acts. Although determining appropriate triggers may be challenging, several have recently been proposed.50 Defining these triggers in advance allows for public and expert consultation to ensure optimal societal agreement before a crisis arises. Once explicit triggers are set, they can also be used as clear benchmarks of pandemic severity and motivators to hold governments responsible for maximizing effective use of resources across regions. Although some may argue that subjective judgement leads to more nuanced decisions and should be allowed to override automatic triggers, we propose that this should be the exception rather than the rule.
A pan-Canadian approach to triage is needed
Automatic triggers address decisional inertia but do not determine who ought to be responsible for determining allocation of scarce life-saving resources and at what level of society this should occur. We propose that governments, not hospitals, ought to be responsible for initiating triage in times of crisis standards of care. We further propose that Canada adopt a national approach to crisis standards of care and triage of critical care resources in preparation for future pandemics.
Governments are directly accountable to members of society, unlike hospital boards or ad hoc triage committees. Appointing governments with the moral responsibility for activating pandemic triage also removes one of many moral burdens from frontline clinicians and allows them to focus on their primary ethical obligation to individual patients and families. Some might worry that political motivations will hinder necessary acts if governments are responsible for triage. These concerns can be mitigated by establishing processes for transparency and accountability, automatic triggers, and binding independent review in advance through democratic legislation. Once such processes are in place, direct accountability and the negative political consequences of triage are more likely to motivate governments to innovate and coordinate resources more effectively across broad regions, rather than avoid decision-making because of political concerns.
A national approach is justified for several reasons. First, by ensuring that a patient’s chance of receiving scarce resources is equivalent regardless of location, a national approach best conforms to the ethical tenants of procedural justice as well as the legislative stipulations of the Canada Health Act.9 More explicit and transparent collaboration between provinces and the federal government provides an opportunity to effectively use national expertise and actively debate key ethical decision points from diverse perspectives. Canada already has a coordinated approach to assessing health technologies and data sharing (Canadian Research Data Centre Network). There is also increasing recognition of the need for pan-Canadian health human resources planning. Thus, there is both precedent and growing demand for national collaboration on key health issues such as pandemic planning.
Second, because global pandemics generally affect entire countries, allowing local triage to occur while resources go unused elsewhere is inefficient and potentially unjust.51 Although geographic constraints will always pose challenges, a national approach allows for a coordinated response to load sharing and the most effective distribution of all available national resources. This approach is particularly beneficial to ensure provinces and territories, such as Nunavut, who rely on intra-provincial transfer to access critical care resources are not unfairly disadvantaged in times of national crisis. Additionally, the federal government already has a well-established blueprint for public consultation and for independent inquiry, as was seen following use of the Emergencies Act in February 2022.52,53 Moreover, a federal approach overcomes concerns at the provincial level about unfavourable comparisons with other provinces, eliminating another barrier to rational risk-based decision-making. Nonetheless, even with enhanced national coordination, regional variation in the need for triage activation will likely remain. Thus, close coordination between provincial and federal levels of governments will always be important and should be integrated into any future crisis standards of care. Concerns about regional autonomy, however, should not outweigh considerations of distributive justice, nor the utilitarian and egalitarian objectives of public health in an emergency.
Strengths and limitations
Regarding the limitations of our study, we were unable to obtain protocols from three provinces. All protocols analyzed in this study were obtained over the summer and fall of 2020 and may have undergone further revisions since that time. Our analysis was confined to written documents and does not capture aspects of protocol development that were not recorded within the documents themselves, which may have included additional public or expert consultation. Finally, although we completed an updated search for revised documents in late 2022, we confined this to publicly available protocols.
Our study also has important strengths. Although there have been several secondary analyses of triage documents, our study focuses specifically on the Canadian context. Furthermore, our study includes documents that were not made publicly available, allowing for a broader comparison. Lastly, we believe our focus on aspects of procedural justice is unique and underrepresented in existing literature on COVID-19 triage.
Conclusion
In Canada, early provincial COVID-19 triage protocols were developed by dedicated committees of thoughtful experts under challenging circumstances. Nonetheless, no protocols were ever implemented, including during periods of extreme critical care surge. While many ethical concerns pertaining to early triage protocols have been addressed,54 others remain unresolved within Canadian health policy, including how to enhance transparency and public accountability. Here, we have attempted to draw attention to aspects of pandemic triage that could benefit from further discussion and have proposed potential avenues for future policy development. Although it is tempting to avoid the topic of triage now that the moment of crisis has passed, a national conversation is needed to learn from recent efforts and prepare for future pandemics.
References
Maves RC, Downar J, Dichter JR, et al. Triage of scarce critical care resources in COVID-19: an implementation guide for regional allocation: an expert panel report of the Task Force for Mass Critical Care and the American College of Chest Physicians. Chest 2020; 158: 212–25. https://doi.org/10.1016/j.chest.2020.03.063
Sprung CL, Joynt GM, Christian MD, Truog RD, Rello J, Nates JL. Adult ICU triage during the coronavirus disease 2019 pandemic: who will live and who will die? Recommendations to Improve Survival. Crit Care Med 2020; 48: 1196–202. https://doi.org/10.1097/ccm.0000000000004410
Antommaria AH, Gibb TS, McGuire AL, et al. Ventilator triage policies during the COVID-19 pandemic at U.S. hospitals associated with members of the Association of Bioethics Program Directors. Ann Intern Med 2020; 173: 188–94. https://doi.org/10.7326/m20-1738
Aquino YS, Rogers WA, Scully JL, Magrabi F, Carter SM. Ethical guidance for hard decisions: a critical review of early international COVID-19 ICU triage guidelines. Health Care Anal 2022; 30: 163–95. https://doi.org/10.1007/s10728-021-00442-0
Ghanbari V, Ardalan A, Zareiyan A, Nejati A, Hanfling D, Bagheri A. Ethical prioritization of patients during disaster triage: a systematic review of current evidence. Int Emerg Nurs 2019; 43: 126–32. https://doi.org/10.1016/j.ienj.2018.10.004
Devereaux AV, Dichter JR, Christian MD, et al. Definitive care for the critically ill during a disaster: a framework for allocation of scarce resources in mass critical care: from a Task Force for Mass Critical Care summit meeting, January 26–27, 2007, Chicago, IL. Chest 2008; 133: 51S–66. https://doi.org/10.1378/chest.07-2693
Thompson AK, Faith K, Gibson JL, Upshur RE. Pandemic influenza preparedness: an ethical framework to guide decision-making. BMC Med Ethics 2006; 7: E12. https://doi.org/10.1186/1472-6939-7-12
Biddison LD, Berkowitz KA, Courtney B, et al. Ethical considerations: care of the critically ill and injured during pandemics and disasters: CHEST consensus statement. Chest 2014; 146: e145S–55. https://doi.org/10.1378/chest.14-0742
Canada Health Act, RCS 1985, c. C-6. Available from URL: https://laws-lois.justice.gc.ca/eng/acts/c-6/page-1.html (accessed January 2024).
Microsoft Corporation. Microsoft Excel. Available from URL: https://office.microsoft.com/excel (accessed January 2024).
Popay J, Roberts H, Sowden A, et al. Guidance on the conduct of narrative synthesis in systematic reviews: a product from the ESRC Methods Programme; 2006. Available from URL: https://www.lancaster.ac.uk/media/lancaster-university/content-assets/documents/fhm/dhr/chir/NSsynthesisguidanceVersion1-April2006.pdf (accessed January 2024).
Stemler S. An overview of content analysis. Pract Assess Res Evaluation 2001; 7. https://doi.org/10.7275/z6fm-2e34
Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res 2005; 15: 1277–88. https://doi.org/10.1177/1049732305276687
Daniels N. Justice, fair procedures, and the goals of medicine. Hastings Cent Rep 1996; 26: 10–2. https://doi.org/10.2307/3528745
Daniels N. Accountability for reasonableness. BMJ 2000; 321: 1300–1. https://doi.org/10.1136/bmj.321.7272.1300
Downar J, Smith MJ, Godkin D, et al. A framework for critical care triage during a major surge in critical illness. Can J Anesth 2022; 69: 774–81. https://doi.org/10.1007/s12630-022-02231-2
Valiani S, Terrett L, Gebhardt C, Prokopchuk-Gauk O, Isinger M. Development of a framework for critical care resource allocation for the COVID-19 pandemic in Saskatchewan. CMAJ 2020; 192: E1067–73. https://doi.org/10.1503/cmaj.200756
Christian MD, Hawryluck L, Wax RS, et al. Development of a triage protocol for critical care during an influenza pandemic. CMAJ 2006; 175: 1377–81. https://doi.org/10.1503/cmaj.060911
Hamilton Health Sciences Corporation. EDM—adult critical care triage and resource allocation protocol for pandemic influenza; 2009. Available from URL: https://www.longwoods.com/articles/images/PandemicProtocol.pdf (accessed January 2024).
Ontario Health. Clinical triage protocol for major surge in COVID pandemic; 2020. Available from URL: https://med.uottawa.ca/pathology/sites/med.uottawa.ca.pathology/files/clinical_triage_protocol_for_major_surge_in_covid_pandemic_-_march_28_20205.pdf (accessed January 2024).
White DB. Allocation of scarce critical care resources during a public health emergency: a model hospital policy; 2020. Available from URL: https://bioethics.pitt.edu/sites/default/files/Univ%20Pittsburgh%20-%20Allocation%20of%20Scarce%20Critical%20Care%20Resources%20During%20a%20Public%20Health%20Emergency.pdf (accessed January 2024).
Fins JJ, Miller FG. Proportionality, pandemics, and medical ethics. Am J Med 2020; 133: 1243–4. https://doi.org/10.1016/j.amjmed.2020.06.008
Ferreira FL, Bota DP, Bross A, Mélot C, Vincent JL. Serial evaluation of the SOFA score to predict outcome in critically ill patients. JAMA 2001; 286: 1754–8. https://doi.org/10.1001/jama.286.14.1754
Leteurtre S, Duhamel A, Salleron J, et al. PELOD-2: an update of the PEdiatric logistic organ dysfunction score. Crit Care Med 2013; 41: 1761–73. https://doi.org/10.1097/ccm.0b013e31828a2bbd
Favaro A, St. Philip E, Cousins B. Coronavirus: Ontario hospitals on the verge of enacting ‘last resort’ triage protocols; 2021. Available from URL: https://www.ctvnews.ca/health/coronavirus/ontario-hospitals-on-the-verge-of-enacting-last-resort-triage-protocols-1.5406746 (accessed January 2024).
Snowdon W. Life and death: what critical-care triage could mean in Alberta ICUs; 2021. Available from URL: https://www.cbc.ca/news/canada/edmonton/emergency-covid-triage-alberta-1.6178253#:~:text=Alberta%27s%20critical%20care%20triage%20protocol,in%20preparation%20for%20the%20worst. (accessed January 2024).
Piscitello GM, Kapania EM, Miller WD, Rojas JC, Siegler M, Parker WF. Variation in ventilator allocation guidelines by US state during the coronavirus disease 2019 pandemic: a systematic review. JAMA Netw Open 2020; 3: e2012606. https://doi.org/10.1001/jamanetworkopen.2020.12606
Raschke RA, Agarwal S, Rangan P, Heise CW, Curry SC. Discriminant accuracy of the SOFA score for determining the probable mortality of patients with COVID-19 pneumonia requiring mechanical ventilation. JAMA 2021; 325: 1469–70. https://doi.org/10.1001/jama.2021.1545
Shahpori R, Stelfox HT, Doig CJ, Boiteau PJ, Zygun DA. Sequential organ failure assessment in H1N1 pandemic planning. Crit Care Med 2011; 39: 827–32. https://doi.org/10.1097/ccm.0b013e318206d548
Mello MM, Persad G, White DB. Respecting disability rights—toward improved crisis standards of care. N Engl J Med 2020; 383: e26. https://doi.org/10.1056/nejmp2011997
Schmidt H, Roberts DE, Eneanya ND. Rationing, racism and justice: advancing the debate around ‘colourblind’ COVID-19 ventilator allocation. J Med Ethics 2022; 48: 126–30. https://doi.org/10.1136/medethics-2020-106856
Solomon MZ, Wynia MK, Gostin LO. Covid-19 crisis triage—optimizing health outcomes and disability rights. N Engl J Med 2020; 383: e27. https://doi.org/10.1056/nejmp2008300
Schmidt H, Roberts DE, Eneanya ND. Sequential organ failure assessment, ventilator rationing and evolving triage guidance: new evidence underlines the need to recognise and revise, unjust allocation frameworks. J Med Ethics 2022; 48: 136–8. https://doi.org/10.1136/medethics-2021-107696
Sonmez T, Pathak PA, Ünver MU, Persad G, Truog RD, White DB. Categorized priority systems: a new tool for fairly allocating scarce medical resources in the face of profound social inequities. Chest 2021; 159: 1294–9. https://doi.org/10.1016/j.chest.2020.12.019
Persad G, Wertheimer A, Emanuel EJ. Principles for allocation of scarce medical interventions. Lancet 2009; 373: 423–31. https://doi.org/10.1016/s0140-6736(09)60137-9
Biddison EL, Gwon HS, Schoch-Spana M, et al. Scarce resource allocation during disasters: a mixed-method community engagement study. Chest 2018; 153: 187–95. https://doi.org/10.1016/j.chest.2017.08.001
Winsor S, Bensimon CM, Sibbald R, et al. Identifying prioritization criteria to supplement critical care triage protocols for the allocation of ventilators during a pandemic influenza. Healthc Q 2014; 17: 44–51. https://doi.org/10.12927/hcq.2014.23833
Cuartas PA, Santos HT, Levy BM, Gong MN, Powell T, Chuang E. How useful are sequential organ failure assessment (SOFA) score-based ventilator triage guidelines during the covid-19 pandemic? Am J Respir Crit Care Med 2021; 203: A1494. https://doi.org/10.1164/ajrccm-conference.2021.203.1_MeetingAbstracts.A1494
Wunsch H, Hill AD, Bosch N, et al. Comparison of 2 triage scoring guidelines for allocation of mechanical ventilators. JAMA Netw Open 2020; 3: e2029250. https://doi.org/10.1001/jamanetworkopen.2020.29250
Hick JL, Hanfling D, Wynia MK, Toner E. Crisis standards of care and COVID-19: what did we learn? How do we ensure equity? What should we do? NAM Perspect 2021; https://doi.org/10.31478/202108e
Kadri SS, Sun J, Lawandi A, et al. Association between caseload surge and COVID-19 survival in 558 U.S. hospitals, March to August 2020. Ann Intern Med 2021; 174: 1240–51. https://doi.org/10.7326/m21-1213
Bravata DM, Perkins AJ, Myers LJ, et al. Association of intensive care unit patient load and demand with mortality rates in US Department of Veterans Affairs hospitals during the COVID-19 pandemic. JAMA Netw Open 2021; 4: e2034266. https://doi.org/10.1001/jamanetworkopen.2020.34266
Rosenbaum L. Facing Covid-19 in Italy—ethics, logistics, and therapeutics on the epidemic’s front line. N Engl J Med 2020; 382: 1873–5. https://doi.org/10.1056/nejmp2005492
Close E, Willmott L, Cockburn T, Young S, Cairns W, White BP. Transparent triage policies during the COVID-19 pandemic: a critical part of medico-legal risk management for clinicians. Med J Aust 2021; 215: 71–4. https://doi.org/10.5694/mja2.51079
McGrail K. Excess mortality, COVID-19 and health care systems in Canada. CMAJ 2022; 194: E741–5. https://doi.org/10.1503/cmaj.220337
ASPR TRACIE. Crisis standards of care during COVID-19: summary of state actions; 2022. Available from URL: https://asprtracie.hhs.gov/technical-resources/resource/10803/crisis-standards-of-care-during-covid-19-summary-of-state-actions (accessed January 2024).
Barasz K, Hagerty SF. Hoping for the worst? A paradoxical preference for bad news. J Consum Res 2021; 48: 270–88. https://doi.org/10.1093/jcr/ucab004
Simonson I. The influence of anticipating regret and responsibility on purchase decisions. J Consum Res 1992; 19: 105–18. https://doi.org/10.1086/209290
Messick DM, Bazerman MH. Ethical leadership and the psychology of decision making; 1996. Available from URL: https://sloanreview.mit.edu/article/ethical-leadership-and-the-psychology-of-decision-making/ (accessed January 2024).
Kelen GD, Marcozzi D, Marx JJ, Kachalia A. Criteria for declaring crisis standards of care: a single, uniform model; 2023. Available from URL: https://catalyst.nejm.org/doi/full//10.1056/CAT.22.0269 (accessed January 2024).
Gordon SH, Huberfeld N, Jones DK. What federalism means for the US response to coronavirus disease 2019. JAMA Health Forum 2020; 1: e200510. https://doi.org/10.1001/jamahealthforum.2020.0510
Emergencies Act, RSC, 1985, c. 22 (4th Supp). Available from URL: https://laws-lois.justice.gc.ca/eng/acts/e-4.5/page-1.html (accessed January 2024).
BBC News. Canada’s use of emergency powers justified—report; 2023. Available from URL: https://www.bbc.com/news/world-us-canada-64683747# (accessed January 2024).
Owens B. Should triage guidelines be revisited ahead of a second wave of COVID-19? CMAJ 2020; 192: E690–1. https://doi.org/10.1503/cmaj.1095876
Author contributions
Sarah K. Andersen was involved in study conception and design, data analysis and interpretation, and drafting and editing the manuscript. Nathan Gamble was involved in data acquisition, data analysis, and manuscript review. Oleksa Rewa was involved in study conception, data acquisition, and manuscript review.
Acknowledgements
An early version of this project was presented at the Harvard Bioethics Fellowship retreat in February 2023. We thank Mildred Solomon and members of the Harvard Bioethics Fellowship Program for their thoughtful input.
Disclosures
Dr. Andersen was a member of the Provincial Pandemic Critical Care Triage Working Group within the Alberta Critical Care Strategic Clinical Network from March to December 2020 and received no financial compensation for this work. Dr. Andersen was a postdoctoral research fellow in the Ethics and Decision Making program at the Clinical Research, Investigation, and Systems Modeling of Acute Illness (CRISMA) Center in the Department of Critical Care Medicine at the University of Pittsburgh and a visiting fellow at the Harvard Medical School Center for Bioethics at the time this study was conducted. There are no other potential conflicts of interest to declare.
Funding statement
Dr. Andersen was supported by a T32 training grant from the National Institutes of Health (NIH) (T32HL007820) at the time of this study. The NIH was not involved in any aspect of study design, data collection and analysis, or manuscript preparation.
Data availability statement
The data sets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Editorial responsibility
This submission was handled by Dr. Patricia S. Fontela, Associate Editor, Canadian Journal of Anesthesia/Journal canadien d’anesthésie.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Andersen, S.K., Gamble, N. & Rewa, O. COVID-19 critical care triage across Canada: a narrative synthesis and ethical analysis of early provincial triage protocols. Can J Anesth/J Can Anesth (2024). https://doi.org/10.1007/s12630-024-02744-y
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12630-024-02744-y