Abstract
Purpose
Individuals in late pregnancy are at risk of significant hemodynamic variations, especially during Cesarean delivery. Although non-invasive monitoring might enable the early detection of variations in cardiac output (CO), clinical validation is lacking.
Methods
In a prospective, single-center study, we measured CO simultaneously with finger plethysmography and transthoracic echocardiography in 100 third-trimester pregnant individuals in the supine and left lateral decubitus (LLD) positions.
Results
A Bland–Altman analysis revealed a mean (standard deviation) bias of 1.36 (1.04) L·min–1 in the supine position (95% limits of agreement, -0.68 to 3.4 L·min–1; percent error, 26.6%), indicating overestimation by finger plethysmography. The intra-class correlation coefficient was 0.43 (95% confidence interval [CI], 0.33 to 0.51). Regarding the changes in CO induced by the supine-to-LLD transition, the concordance rate in a four-quadrant plot was 98.3% (95% CI, 91.1 to 99.9%).
Conclusion
Our study showed a poor reliability of finger plethysmography for static measurement of CO. Nevertheless, finger plethysmography had a reasonably high concordance rate for the detection of CO changes secondary to positional changes in late-pregnant individuals.
Study registration date
www.clinicaltrials.gov (NCT03735043); registered 8 November 2018.
Résumé
Objectif
Les personnes en fin de grossesse sont à risque de variations hémodynamiques importantes, en particulier pendant un accouchement par césarienne. Bien que le monitorage non invasif puisse permettre la détection précoce des variations du débit cardiaque (DC), la validation clinique de ce type de monitorage fait défaut.
Méthode
Dans une étude prospective monocentrique, nous avons mesuré le DC simultanément avec la pléthysmographie au doigt et l’échocardiographie transthoracique chez 100 femmes au troisième trimestre de leur grossesse en décubitus dorsal et en décubitus latéral gauche (DLG).
Résultats
Une analyse de Bland-Altman a révélé un biais moyen (écart type) de 1,36 (1,04) L·min–1 en décubitus dorsal (limites d’agrément à 95 %, -0,68 à 3,4 L·min–1; pourcentage d’erreur, 26,6 %), indiquant une surestimation lorsque mesuré par pléthysmographie au doigt. Le coefficient de corrélation intraclasse était de 0,43 (intervalle de confiance [IC] à 95 %, 0,33 à 0,51). En ce qui concerne les changements de DC induits par la transition du décubitus dorsal au décubitus latéral gauche, le taux de concordance dans un diagramme à quatre quadrants était de 98,3 % (IC 95 %, 91,1 à 99,9 %).
Conclusion
Notre étude a montré une faible fiabilité de la pléthysmographie au doigt pour la mesure statique du DC. Néanmoins, la pléthysmographie au doigt avait un taux de concordance raisonnablement élevé pour la détection des changements de DC secondaires aux changements de position chez les patientes en fin de grossesse.
www.clinicaltrials.gov (NCT03735043); enregistrée le 8 novembre 2018.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
It is well known that pregnancy induces changes in the body’s hemodynamics. Although the plasma volume reportedly increases as early as the first trimester of pregnancy, cardiac output (CO) may decrease as a result of compression of the inferior vena cava (IVC) by the gravid uterus when the pregnant individual is in the supine position (IVC syndrome), which decreases venous return to the heart. This decrease in CO can usually be corrected by moving into the left lateral decubitus (LLD) position.1 The risk of IVC syndrome and hemodynamic variations is greatest after 32 weeks of amenorrhea.2
Hemodynamic changes are accentuated by venous vasoplegia following epidural anesthesia for Cesarean delivery. It has been suggested that a decrease in CO could have major consequences on maternal and fetal homeostasis, and might be associated with greater fetal morbidity and mortality,1,3,4,5,6,7 even though robust data regarding this association are lacking. Furthermore, postpartum hemorrhage, one of the possible obstetrical complications, is associated with marked decreases in CO. Recent guidelines have recommended considering timely CO monitoring during the acute postpartum hemorrhage phase according to the severity of blood loss.8 Cardiac output monitoring therefore appears to be a core component of obstetric anesthesia practice.
Maternal hemodynamic monitoring is currently based on non-invasive blood pressure (BP) measurement. Nevertheless, BP is poorly correlated with CO,9 and decreases in CO are sometimes detected late as a result of physiologic compensation mechanisms and long time intervals between two successive non-invasive BP measurements. Another non-invasive technique, transthoracic echocardiography (TTE), has been validated for use during pregnancy.10,11,12 Interestingly, measurement of CO by TTE seems to remain accurate during the third trimester of pregnancy.13,14 Nevertheless, bedside operating conditions, requirement for a trained operator, discontinuous nature of the measurements, and a fixed measurement time are major limitations of TTE for continuous hemodynamic monitoring.
The ccNexfin™ finger plethysmograph (Edwards Lifesciences, Irvine, CA, USA) is a non-invasive device for continuous, operator-independent CO measurement, based on the volume clamp method and a digital pulse waveform contour analysis. The data currently available for male and non-pregnant female individuals suggest that the ccNexfin provides moderately reliable measurement of CO, with Bland–Altman analysis showing a mean (standard deviation [SD]) bias of 0.51 (1.1) L·min-1 and limits of agreement of -1.6 to 2.6 L·min-1, with a percentage error of 39%.15 In contrast, studies of pregnant people suggested that finger plethysmography is not accurate enough to measure CO. Nevertheless, these studies had moderate sample sizes16,17 or did not assess trending ability (i.e., a device’s ability to track CO variations).16
The main objectives of the present study were therefore to 1) compare CO measurements obtained simultaneously with TTE and the ccNexfin in a larger cohort of late-pregnant individuals at rest in the supine position, and 2) assess and compare CO variations induced by movement into the LLD position.
Methods
Ethics
Ethical approval for this study was provided by the Comité de Protection des Personnes Sud Méditerranée V (4 Avenue Reine Victoria Bat Victoria CS 91179 – 06003 Nice, France; protocol number, 2018-AOI089-46; Chair, Philippe Babe) on 2 January 2019. Written informed consent was obtained from all participants. The protocol was registered at www.ClinicalTrials.gov on 8 November 2018 (registration number, NCT03735043; principal investigator, Alexandre Gaudet). Registration of the study occurred prior to the start of the trial and patient enrollment.
Study design and participants
This prospective study was conducted in a French tertiary maternity hospital (Maternité Jeanne de Flandre, Lille University Medical Centre, Lille, France). Study participants had to meet all of the following criteria: age 18 yr or over, 32 or more weeks of amenorrhea upon enrollment, health insurance coverage, and the provision of written consent to participate in the study. The main exclusion criteria were a history of heart disease, poor echocardiography window, disability, the need to remain in the supine position alone or the LLD position alone, inability to understand study information or provide written consent, refusal to give consent, and being subject to legal guardianship. Potentially eligible participants were identified and enrolled based on convenience sampling among women hospitalized in the Department of Obstetrics between 2 July 2019 and 28 May 2020. The following data were collected upon enrollment: demographic variables, term of pregnancy, pre-existing conditions, and treatments initiated prior to and during the hospital stay.
Procedures and measurements
Patients underwent simultaneous CO monitoring with ccNexfin and TTE (Vivid I™, GE Healthcare, Wauwatosa, WI, USA). All measurements were performed at rest in the patient’s hospital room. An appropriately sized ccNexfin finger cuff was applied to the mid-phalanx of the middle finger of the right hand. The ccNexfin was operated according to the manufacturer’s instructions.
The investigators making the TTE measurements were blinded to the values obtained with the ccNexfin. Cardiac output was measured first in the supine position and then after the participant had been in the LLD position for one minute, so that the weight of the uterus was fully supported by the mattress. All TTE measurements were performed by the same trained operator. The trained operator was an anesthesiologist with daily practice in echocardiography, certified by a degree in ultrasound techniques in anesthesiology and critical care (specialization: hemodynamic/University of Lille).
Values recorded simultaneously with the ccNexfin and TTE were averaged over ten consecutive heartbeats, and the CO was calculated as follows. For the TTE, the left ventricular stroke volume (LVSV) was calculated as the product of the left ventricular outflow tract (LVOT) area and the velocity time integral (VTI) of LVOT blood flow. We used the 2D parasternal long-axis view to measure the diameter of LVOT during systole, and the apical five-chamber view to measure the VTI of LVOT blood flow by pulse-wave Doppler. Next, VTI measurements were averaged over ten consecutive heart beats, and CO was calculated as the product of the LVSV and the heart rate. For the ccNexfin, the LVSV and CO values (averaged over ten consecutive heart beats) were read off the monitor’s display.
Objectives
The study’s primary objective was to evaluate the level of agreement between maternal supine CO measurements performed with TTE and the ccNexfin. The secondary objectives were to 1) assess the level of agreement between changes in LVSV and CO upon the transition from the supine position to the LLD position, as measured with TTE and the ccNexfin, and 2) assess the level of agreement between maternal LLD CO measurements performed with TTE and the ccNexfin.
Guidelines
This manuscript adheres to the applicable Standards for Reporting Diagnostic Accuracy Studies (STARD) guidelinesFootnote 1 (Electronic Supplementary Material, eAppendix).
Statistical analysis
The primary endpoint was the intra-class correlation coefficient (ICC) for the agreement between maternal supine CO values assessed simultaneously with TTE and the ccNexfin in each position (supine and LLD). With an expected ICC of 0.85, a type I error at 0.025, and a type II error of 0.2, we calculated that a sample size of 100 participants would be necessary to show an ICC above 0.75 (one-sided test).
The degree of agreement between the two methods was studied further with a Bland–Altman plot; this gave the mean of differences (calculated as CONexfin − COTTE) defining bias, the SD, and the limits of agreement (LOA) calculated as a bias (1.96 SD). The percent error (PE) was calculated using Critchley’s method18 as follows: PE = (upper LOA − lower LOA)/([mean COTTE + mean CONexfin]/2). The supine-LLD concordance rate between the two methods was calculated from a four-quadrant plot, as follows: 1) we calculated ΔCO as 1 − COsupine/COLL for ccNexfin and TTE; 2) data points in the central area of the four-quadrant plot with a change below 10% were considered to be noise and were excluded; 3) we calculated the concordance rate as the rate of points that have the same sign for ΔCO assessed by ccNexfin and ΔCO assessed by TTE. Confidence intervals were computed using the exact Clopper–Pearson method. Good trending ability was defined as a concordance rate of more than 90%.19 Lastly, values measured in the supine and LLD positions were compared in Wilcoxon’s signed rank test.
Categorical variables were expressed as the frequency (percentage). The normality of distribution of continuous variables was checked graphically and by using the Shapiro–Wilk test. Skewed continuous variables were expressed as the median [interquartile range (IQR)]. Normally distributed continuous variables were expressed as the mean (SD).
Statistical analysis was performed by the Biostatistical Methodology Unit at Lille University Medical Centre (Lille, France) using SAS software (version 9.4, SAS Institute, Inc., Cary; NC; USA). The threshold for statistical significance was set to P < 0.05.
Results
Characteristics of the study participants
We screened 112 participants between 2 July 2019 and 28 May 2020; six were excluded because of a history of heart disease and six refused to participate. All of the 100 participants enrolled in the study were included in the final analysis (Fig. 1). The mean (SD) age was 31.1 (6.1) yr, and the mean gestational age was 36.7 (2.8) weeks of amenorrhea. There were 93 (93%) singleton pregnancies, six (6%) twin pregnancies, and one (1%) triplet pregnancy. The mean body mass index was 29.7 (5.4) kg·m-2. The study participants’ characteristics are summarized in the Table.
Hemodynamic variables
All the patients had a satisfactory TTE window and ccNexfin reading. The mean (SD) heart rate (measured with the ccNexfin) was 87 (14) bpm in the supine position and 87 (13) bpm in the LLD position. The CO in the supine position was 7.0 (1.3) L·min-1 according to TTE and 8.3 (1.3) L·min-1 according to the ccNexfin (N = 100 pairs of measurement). After a move to the LLD position, the CO was 7.4 (1.4) L·min-1 according to TTE and 8.9 (1.6) L·min-1 according to the ccNexfin (N = 100 pairs of measurement). The LVSV measured in the supine position was 81 (11) mL according to TTE and 97 (16) mL according to the ccNexfin. After a move to the LLD position, the LVSV was 86 (11) mL according to TTE and 105 (15) mL according to the ccNexfin.
Agreement between CO values measured simultaneously with TTE and the ccNexfin
In the supine position, the ICC for CO values evaluated simultaneously with TTE and the ccNexfin was 0.43 (95% CI, 0.33 to 0.51).
In the LLD position, the ICC for CO values measured simultaneously with TTE and the ccNexfin was 0.50 (95% CI, 0.41 to 0.57),
The agreement between TTE and the ccNexfin for the measurement of CO was then evaluated in a Bland–Altman analysis. In the supine position, the mean (SD) bias was 1.36 (1.04) L·min-1 (95% LOA, -0.68 to 3.4 L·min-1; PE, 26.6%), indicating overestimation by the ccNexfin. In the LLD position, this bias was 1.52 (1.06) L·min-1 (95% LOA, -0.56 to 3.60 L·min-1; PE, 25.4%), indicating overestimation by the ccNexfin. In the supine position, the measured CO was higher for the ccNexfin than for TTE in 91 of the 100 participants, and lower in seven of the 100 participants. In the LLD position, the measured CO was higher for the ccNexfin than for TTE in 89 of the 100 participants and lower in nine of the 100 participants (Fig. 2).
Bland–Altman plots of the agreement between CO values measured with ccNexfin™ and TTE in the supine position (A) and in the LLD position (B).
For each dot, the mean CO values measured with ccNexfin and TTE are represented on the x-axis, and differences between the values are shown on the y-axis. The mean difference (bias) and the 95% confidence interval for the difference (limits of agreement) between the two methods are represented by blue and green dashed lines, respectively. CO = cardiac output; TTE = transthoracic echocardiography
Hemodynamic variables as a function of the position
With TTE, a move to the LLD position resulted in a median [IQR] increase of 9.0 [4.3–15.2]% in CO and a median [IQR] increase of 7.8 [4.56–15.0]% in LVSV. According to TTE, the CO increased in 69/100 participants and decreased in 28/100 participants. With the ccNexfin, a move to the LLD position resulted in a median [IQR] increase of 9.9 [4.1–17.2]% in CO and a median [IQR] increase of 9.5 [5.2–14.7]% in LVSV. According to the ccNexfin, the CO increased in 74/100 participants and decreased in 22/100 participants. Values for CO and LVSV were higher in LLD position than in supine position (Wilcoxon’s signed rank test, P < 0.001) (Fig. 3).
Box plots of CO measured with TTE (A) and the ccNexfin (B), and the LVSV measured with TTE (C) and the ccNexfin (D) in the supine position and in the LLD position. The box plot shows the median (horizontal line) and interquartile range [IQR] (box). The whiskers show the data within 1.5 IQR of the lowest quartile and those within 1.5 IQR of the highest quartile. Data more than 1.5 IQR outside the upper or lower quartiles are depicted as dots. The mean value is shown as a dot in the box. P values are reported for paired Wilcoxon test. CO = cardiac output; LVSV = left ventricular stroke volume; TTE = transthoracic echocardiography
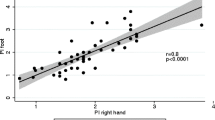
Concordance between position-related changes in hemodynamic variables
The hemodynamic variations observed simultaneously with TTE and the ccNexfin during the transition from the supine position to the LLD position are shown in Fig. 4. The concordance rate for TTE and the ccNexfin was 98.3% (95% CI, 91.1 to 99.9) for CO and 94.9% (95% CI, 85.9 to 98.9) for the LVSV. Patients with discordant variations for CO and LVSV were the same.
Four-quadrant plots of concordance in variations of CO (A) and LVSV (B) induced by a change in position, measured simultaneously with TTE and the ccNexfin. For each dot, the variation in the measured values is represented on the x-axis for TTE and on the y-axis for the ccNexfin. Variations below 10% (gray dots in the exclusion zone represented by the inner rectangle) were excluded from the analysis. CO = cardiac output; LLD = left lateral decubitus; LVSV = left ventricular stroke volume; TTE = transthoracic echocardiography
Discussion
Our present results show a systematic bias in the measurement of CO between the ccNexfin and TTE, with wide LOA between the two devices. Nevertheless, we observed a very high concordance rate between the ccNexfin and TTE for the variations in CO caused by a change of position. Thus, our data suggest that the ccNexfin is unreliable for static CO measurement in the third trimester of pregnancy. Nevertheless, ccNexfin appears to detect concordant changes of CO secondary to position changes. Accordingly, it may be used to detect directional changes of CO and, in conjunction with other monitoring such as maternal BP and fetal heart rate characteristics, may lead to faster implementation of resuscitative measures.
A number of researchers have addressed the non-invasive monitoring of CO in late pregnancy, including techniques based on bioreactance. Even though some studies suggest that bioreactance devices are sufficiently accurate,20,21 the published data are still subject to debate.22 The few published studies of finger-cuff-based plethysmography in late pregnancy have reported a low level of accuracy for monitoring static CO values. Indeed, Duclos et al. reported the systematic overestimation of CO measured with finger cuff plethysmography (relative to TTE), with a mean bias of 2.7 (95% CI, 2.3 to 3.0) L·min-1; LOA, -0.1 to 5.4 L·min-1), which is consistent with our results.16
One possible explanation for this CO discrepancy between the ccNexfin and TTE relates to the fact that CO measurement by ccNexfin is sensitive to the tonus of the digital artery, and can subsequently be affected by the physiologic decrease of vascular resistance that occurs during pregnancy.23 In addition, the algorithm used by the ccNexfin to calculate the LVSV considers the patient’s weight, sex, and height. Nevertheless, the weight measured during pregnancy includes the weight of the fetus and blood volume expansion, in addition to the individual’s true weight. These changes may therefore be responsible for the systematic bias observed in the estimation of LVSV and thus CO. Evaluations of the ccNexfin in morbidly obese patients gave similar results, i.e., a positive, systematic bias for the ccNexfin relative to transpulmonary thermodilution.24,25 Interestingly, the fact that this bias became null when “adjusted weight” was used25 suggests that a similar correction should be applied with pregnant individuals. Alternatively, using the body weight measured at the start of pregnancy might avoid overestimation of the CO by the ccNexfin.
Interestingly, we were able to detect increases and decreases in CO after a move to the LLD position, which is consistent with the literature.1 The ccNexfin therefore shows excellent trending ability for detecting CO variations; hence, this device might be valuable for hemodynamic monitoring in late pregnancy.
The present study had several limitations. Firstly, we studied pregnant individuals who were not in labor, and the reported conditions may have differed from those encountered during Cesarean delivery. Indeed, the algorithm used by the ccNexfin to calculate the LVSV is based on arterial vascular tone; consequently, the use of vasopressor drugs or regional anesthesia is likely to interfere with the device’s measurements. This is an important limitation for interpreting hemodynamic monitoring by ccNexfin during Cesarean delivery, which is frequently associated with spinal anesthesia and necessary vasopressor therapy. Secondly, even though previously published studies had smaller sample sizes than ours, the overall number of data points were similar. Nonetheless, the greater sample size used in our study may have lowered the risk of variations caused by interindividual factors such as weight uptake during pregnancy or vascular tone, which may diverge from one individual to another. Thirdly, the TTE reference method for measuring CO is known to be operator-dependent26 and is thus different from a previous methodology that relies on LiDCO™ (Masimo Corporation, Irvine, CA, USA) for CO measurement.17 Nevertheless, the use of TTE in our study was supported by the excellent agreement reported in the literature between CO measurements obtained by TTE and pulmonary artery catheterization in pregnant women, with an intra-class correlation coefficient of 0.94.11 Because the accuracy was very high and because guidelines and recommendations were followed,12 we considered that TTE could be used as a reference for validating finger plethysmography. In addition, our CO and LVSV values were very close to those published in the literature, which strengthens the reliability of our measurements.27,28 Fourthly, our study focused mainly on the ccNexfin’s ability to detect increases in CO. Although our data suggested that the ccNexfin is equally able to detect increases and decreases in CO, this question needs to be addressed in a larger study. Fifthly, trending ability was only assessed by two points in our study, which limits the reliability of our results on the ability of ccNexfin to track changes in CO. Lastly, our study did not address the threshold of CO variation beyond which a therapeutic action must be initiated. Consequently, the corrective actions to be undertaken for a given value of CO variation remain uncertain. Further studies are needed to address this question.
Conclusions
The findings of our study indicate that ccNexfin had a large systematic overestimation of CO measurement compared with TTE. Our results suggest that ccNexfin is not a reliable static CO measurement in third-trimester pregnant individuals. Nevertheless, our study also found that ccNexfin had a reasonably high concordance rate for detecting CO changes secondary to positional changes. This latter finding suggests that the ccNexfin may be helpful in informing about directional changes of CO in third-trimester pregnant individuals.
Notes
Equator Network. STARD 2015: An updated list of essential items for reporting diagnostic accuracy studies, 2021. Available from URL: https://www.equator-network.org/reporting-guidelines/stard/ (accessed June 2022).
References
Lee AJ, Landau R. Aortocaval compression syndrome: time to revisit certain dogmas. Anesth Analg 2017; 125: 1975–85. https://doi.org/10.1213/ANE.0000000000002313
Constans B, Langlois S, Vallet B. Influence du terme et de la position sur l’hémodynamique maternelle. intérêt des mesures non invasives. Ann Fr Anesth Réanimation 2014; 33: A321–2. https://doi.org/10.1016/j.annfar.2014.07.542
Rout CC, Rocke DA, Levin J, Gouws E, Reddy D. A reevaluation of the role of crystalloid preload in the prevention of hypotension associated with spinal anesthesia for elective cesarean section. Anesthesiology 1993; 79: 262–9. https://doi.org/10.1097/00000542-199308000-00011
Mercier FJ, Diemunsch P, Ducloy-Bouthors AS, et al. 6% Hydroxyethyl starch (130/0.4) vs Ringer’s lactate preloading before spinal anaesthesia for Caesarean delivery: the randomized, double-blind, multicentre CAESAR trial. Br J Anaesth 2014; 113: 459–67. https://doi.org/10.1093/bja/aeu103
Cyna AM, Andrew M, Emmett RS, Middleton P, Simmons SW. Techniques for preventing hypotension during spinal anaesthesia for caesarean section. Cochrane Database Syst Rev 2006; 18: CD002251. https://doi.org/10.1002/14651858.CD002251.pub2
Ebner H, Barcohana J, Bartoshuk AK. Influence of postspinal hypotension on the fetal electrocardiogram. Am J Obstet Gynecol 1960; 80: 569–72. https://doi.org/10.1016/s0002-9378(16)36516-4
Corke BC, Datta S, Ostheimer GW, Weiss JB, Alper MH. Spinal anaesthesia for Caesarean section. The influence of hypotension on neonatal outcome. Anaesthesia 1982; 37: 658–62. https://doi.org/10.1111/j.1365-2044.1982.tb01278.x
Muñoz M, Stensballe J, Ducloy-Bouthors AS, et al. Patient blood management in obstetrics: prevention and treatment of postpartum haemorrhage. A NATA consensus statement. Blood Transfus 2019; 17: 112–36. https://doi.org/10.2450/2019.0245-18
Le Manach Y, Hofer CK, Lehot JJ, et al. Can changes in arterial pressure be used to detect changes in cardiac output during volume expansion in the perioperative period? Anesthesiology 2012; 117: 1165–74. https://doi.org/10.1097/ALN.0b013e318275561d
Tsiaras S, Poppas A. Cardiac disease in pregnancy: value of echocardiography. Curr Cardiol Rep 2010; 12: 250–6. https://doi.org/10.1007/s11886-010-0106-9
Cornette J, Laker S, Jeffery B, et al. Validation of maternal cardiac output assessed by transthoracic echocardiography against pulmonary artery catheterization in severely ill pregnant women: prospective comparative study and systematic review. Ultrasound Obstet Gynecol 2017; 49: 25–31. https://doi.org/10.1002/uog.16015
Bijl RC, Valensise H, Novelli GP, et al. Methods and considerations concerning cardiac output measurement in pregnant women: recommendations of the International Working Group on Maternal Hemodynamics. Ultrasound Obstet Gynecol 2019; 54: 35–50. https://doi.org/10.1002/uog.20231
Lee W, Rokey R, Cotton DB. Noninvasive maternal stroke volume and cardiac output determinations by pulsed Doppler echocardiography. Am J Obstet Gynecol 1988; 158: 505–10. https://doi.org/10.1016/0002-9378(88)90014-2
Belfort MA, Rokey R, Saade GR, Moise KJ JR. Rapid echocardiographic assessment of left and right heart hemodynamics in critically ill obstetric patients. Am J Obstet Gynecol 1994; 171: 884–92. https://doi.org/10.1016/s0002-9378(94)70055-9
van der Spoel AGE, Voogel AJ, Folkers A, Boer C, Bouwman RA. Comparison of noninvasive continuous arterial waveform analysis (Nexfin) with transthoracic Doppler echocardiography for monitoring of cardiac output. J Clin Anesth 2012; 24: 304–9. https://doi.org/10.1016/j.jclinane.2011.09.008
Duclos G, Hili A, Resseguier N, et al. ClearsightTM use for haemodynamic monitoring during the third trimester of pregnancy - a validation study. Int J Obstet Anesth 2018; 36: 85–95. https://doi.org/10.1016/j.ijoa.2018.04.009
Omenås IN, Tronstad C, Rosseland LA. Accuracy and trending abilities of finger plethysmographic blood pressure and cardiac output compared to invasive measurements during caesarean delivery in healthy women: an observational study. BMC Anesthesiol 2020; 20: 157. https://doi.org/10.1186/s12871-020-01078-8
Critchley LA, Critchley JA. A meta-analysis of studies using bias and precision statistics to compare cardiac output measurement techniques. J Clin Monit Comput 1999; 15: 85–91. https://doi.org/10.1023/a:1009982611386
Critchley LA, Lee A, Ho AM. A critical review of the ability of continuous cardiac output monitors to measure trends in cardiac output. Anesth Analg 2010; 111: 1180–92. https://doi.org/10.1213/ANE.0b013e3181f08a5b
Doherty A, El-Khuffash A, Monteith C, et al. Comparison of bioreactance and echocardiographic non-invasive cardiac output monitoring and myocardial function assessment in primagravida women. Br J Anaesth 2017; 118: 527–32. https://doi.org/10.1093/bja/aex045
Ling HZ, Gallardo-Arozena M, Company-Calabuig AM, Nicolaides KH, Kametas NA. Clinical validation of bioreactance for the measurement of cardiac output in pregnancy. Anaesthesia 2020; 75: 1307–13. https://doi.org/10.1111/anae.15110
McLaughlin K, Wright SP, Kingdom JCP, Parker JD. Clinical validation of non-invasive cardiac output monitoring in healthy pregnant women. J Obstet Gynaecol Can 2017; 39: 1008–14. https://doi.org/10.1016/j.jogc.2017.02.015
Melchiorre K, Sharma R, Khalil A, Thilaganathan B. Maternal cardiovascular function in normal pregnancy: evidence of maladaptation to chronic volume overload. Hypertens 2016; 67: 754–62. https://doi.org/10.1161/HYPERTENSIONAHA.115.06667
Schraverus P, Kuijpers MM, Coumou J, Boly CA, Boer C, van Kralingen S. Level of agreement between cardiac output measurements using Nexfin® and thermodilution in morbidly obese patients undergoing laparoscopic surgery. Anaesthesia 2016; 71: 1449–55. https://doi.org/10.1111/anae.13627
Boly CA, Schraverus P, van Raalten F, Coumou JW, Boer C, van Kralingen S. Pulse-contour derived cardiac output measurements in morbid obesity: influence of actual, ideal and adjusted bodyweight. J Clin Monit Comput 2018; 32: 423–8. https://doi.org/10.1007/s10877-017-0053-8
Jozwiak M, Mercado P, Teboul JL, et al. What is the lowest change in cardiac output that transthoracic echocardiography can detect? Crit Care 2019; 23: 116. https://doi.org/10.1186/s13054-019-2413-x
Kager CCM, Dekker GA, Stam MC. Measurement of cardiac output in normal pregnancy by a non-invasive two-dimensional independent Doppler device. Aust N Z J Obstet Gynaecol 2009; 49: 142–4. https://doi.org/10.1111/j.1479-828x.2009.00948.x
Meah VL, Cockcroft JR, Backx K, Shave R, Stöhr EJ. Cardiac output and related haemodynamics during pregnancy: a series of meta-analyses. Heart 2016; 102: 518–26. https://doi.org/10.1136/heartjnl-2015-308476
Author contributions
Paul Bonnin contributed to data acquisition, analysis and interpretation, and drafted the manuscript. Alexandre Gaudet contributed to data acquisition, analysis and interpretation and drafted the manuscript. Alain Duhamel contributed to data analysis and interpretation. Maéva Kyheng contributed to data analysis and interpretation. Anne-Sophie Ducloy-Bouthors, Max Gonzalez Estevez, Benoit Tavernier contributed to data acquisition and interpretation, and revised the manuscript. Benjamin Constans contributed to data acquisition, analysis and interpretation and revised the manuscript.
Disclosures
The authors have no conflict of interest to declare.
Funding statement
None.
Editorial responsibility
This submission was handled by Dr. Stephan K. W. Schwarz, Editor-in-Chief, Canadian Journal of Anesthesia/Journal canadien d’anesthésie.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bonnin, P., Constans, B., Duhamel, A. et al. Accuracy and trending ability of finger plethysmographic cardiac output monitoring in late pregnancy. Can J Anesth/J Can Anesth 69, 1340–1348 (2022). https://doi.org/10.1007/s12630-022-02297-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-022-02297-y