Abstract
Purpose
In the preceding 20 years, many randomized-controlled trials and meta-analyses have compared direct Macintosh laryngoscopy with videolaryngoscopy. The videolaryngoscope blades have included both traditional Macintosh blades and hyperangulated blades. Macintosh and hyperangulated blades differ in their geometry and technique for tracheal intubation; certain patient populations may benefit from one blade type over another. The primary objective of this systematic review was to assess whether published meta-analyses comparing direct Macintosh laryngoscopy to videolaryngoscopy have accounted for the videolaryngoscope blade type. Secondary objectives evaluated heterogeneity among practitioner experience and specialty, clinical context, patient population, and original primary study outcomes.
Source
A search was performed across Ovid Medline, Ovid Embase, ClinicalKey, PubMed, TRIP, AccessAnesthesiology, Google Scholar, and ANZCA discovery. A systematic review identified meta-analyses which compared direct Macintosh laryngoscopy to videolaryngoscopy. There were no patient age or clinical specialty restrictions. Exclusion criteria included non-English language, studies comparing non-Macintosh blade to videolaryngoscopy, and studies in awake patients.
Principal findings
Twenty-one meta-analyses were identified that were published between 1 January 2000 and 7 May 2020. Macintosh and hyperangulated videolaryngoscope blades were combined in most studies (16/21; 76%). Heterogeneity was also present among practitioner experience (20/21; 95%), clinician specialty (15/21; 71%), and clinical locations (10/21; 48%). Adult and pediatric patients were combined or not defined in 5/21 studies (24%). The primary outcomes of the meta-analyses varied, with the most common (7/21; 33%) being first-pass tracheal intubation success.
Conclusions
Heterogeneity across important clinical variables is common in meta-analyses comparing direct Macintosh laryngoscopy to videolaryngoscopy. To better inform patient care, future videolaryngoscopy research should differentiate blade type, clinical context, and patient-related primary outcomes.
Résumé
Objectif
Au cours des 20 dernières années, de nombreuses études randomisées contrôlées et méta-analyses ont comparé la laryngoscopie avec lame Macintosh à la vidéolaryngoscopie. Les lames de vidéolaryngoscope ont inclus à la fois des lames Macintosh traditionnelles et des lames hyperangulées. Les lames Macintosh et les lames hyperangulées diffèrent de par leur géométrie et leur technique pour l’intubation endotrachéale; certaines populations de patients pourraient bénéficier davantage d’un type de lame par rapport à une autre. L’objectif principal de cette revue systématique était d’examiner si les méta-analyses publiées comparant la laryngoscopie directe avec lame Macintosh à la vidéolaryngoscopie avaient tenu compte du type de lame du vidéolaryngoscope. Les objectifs secondaires évaluaient l’hétérogénéité entre l’expérience et la spécialité des praticiens, le contexte clinique, la population de patients et les critères d’évaluation principaux originaux.
Source
Une recherche a été effectuée dans les bases de données Ovid Medline, Ovid Embase, ClinicalKey, PubMed, TRIP, AccessAnesthesiology, Google Scholar et ANZCA discovery. Une revue systématique a identifié les méta-analyses comparant la laryngoscopie directe avec lame Macintosh à la vidéolaryngoscopie. Aucune restriction n’a été établie en matière d’âge des patients ou de spécialité clinique. Les critères d’exclusion comprenaient la langue non anglaise, les études comparant les lames autres que Macintosh à la vidéolaryngoscopie, et les études chez les patients éveillés.
Constatations principales
Vingt et une méta-analyses publiées entre le 1er janvier 2000 et le 7 mai 2020 ont été identifiées. Les lames de vidéolaryngoscope Macintosh et hyperangulées ont été combinées dans la plupart des études (16/21; 76 %). L’hétérogénéité était également présente en ce qui touchait à l’expérience des praticiens (20/21; 95 %), à la spécialité des cliniciens (15/21; 71 %) et aux départements cliniques (10/21; 48 %). Les patients adultes et pédiatriques étaient combinés ou non définis dans 5/21 études (24 %). Les critères d’évaluation principaux des méta-analyses étaient variés, les plus fréquents (7/21; 33 %) étant le succès de l’intubation trachéale à la première tentative.
Conclusion
L’hétérogénéité de plusieurs variables cliniques importantes est fréquente dans les méta-analyses comparant la laryngoscopie directe avec lame Macintosh à la vidéolaryngoscopie. Pour mieux guider les soins aux patients, la recherche future sur la vidéolaryngoscopie devrait différencier le type de lame, le contexte clinique et les critères d’évaluation principaux liés au patient.
Similar content being viewed by others
Videolaryngoscopy (VL) is increasingly recommended in airway management guidelines to facilitate tracheal intubation.1,2 The ongoing coronavirus disease (COVID-19) pandemic has compounded this interest3,4 with COVID-19 airway guidelines recommending VL use as a first approach to improve first-pass success and enable increased distance of the intubator from the patient’s airway.5 As more experts call for the liberal (and even exclusive) use of VL,6 the clinician must turn to the published literature for evidence of a clear benefit for VL over traditional direct laryngoscopy using a Macintosh blade (Mac-DL). Literature comparing VL to Mac-DL often describes an improved glottic view,7,8,9,10,11,12,13,14,15,16 and either the same or improved tracheal intubation success with VL.7,8,9,10,11,12,14,16,17,18,19,20,21,22,23,24,25,26,27,28,29 Additionally, several studies describe fewer complications with VL, including fewer esophageal intubations14,21,26,30 and glottic trauma.12,20,27
Many clinical trials have been published that compare VL with Mac-DL. The large number of published studies has allowed a number of meta-analyses to be performed. The quality and reliability of these findings depends on the quality of the constituent studies and whether they are similar enough to produce meaningful outcomes when combined.31 For example, combining hyperangulated VL (HA-VL) with Macintosh-VL (Mac-VL) studies into a pooled VL group may be inappropriate given the significant differences in indications and techniques between these blades. Such meta-analyses would not inform which blade type to utilize to support first-pass tracheal intubation success. In addition, content expertise is required to determine whether differences in patients recruited, practitioner experience, clinical specialty, location, and context of care are too different to be combined in a meta-analysis. If substantial heterogeneity is evident, highlighting such potential methodological weaknesses could inform future research and help avoid critical confounders that prevent meaningful conclusions.
The aim of this study was to examine published meta-analyses of VL for heterogeneity. The primary objective was to quantify the extent to which meta-analyses account for blade type in their comparison of VL to DL. The secondary objectives included quantifying any heterogeneity of practitioner experience and specialty, clinical location, patient population, and original primary study outcomes (e.g., view of the vocal cords, time to intubation, or first attempt success).
Methods
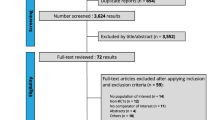
We performed a systematic review to identify meta-analyses comparing any form of VL with Mac-DL. The search was conducted by a medical librarian (Australia and New Zealand College of Anaesthetists Library) across the following databases: Ovid Medline, Ovid Embase, ClinicalKey, PubMed, TRIP, AccessAnesthesiology, Google Scholar, and ANZCA discovery on 1 June 2019 and redone on 7 May 2020. The search strategy is presented in the Appendix. The systematic review was conducted using the PRISMA checklist; it was not registered on PROSPERO. As VL emerged in the early 2000s, we searched literature that was published between 1 January 2000 and 7 May 2020, inclusive. The included meta-analyses contained patients of all ages, and there were no clinical specialty restrictions. Exclusion criteria included studies comparing the Miller blade to VL, studies using awake intubation, and non-English language studies. We captured details of heterogeneity including VL blade type, clinician experience and speciality, clinical location, and patient population.31
Our primary and secondary endpoints were determined and defined a priori. The primary outcome assessed was the number of meta-analyses during the study period that did not account for blade type in their comparison of VL with DL (i.e., two or more blade types in the VL group). Secondary outcomes included evaluation of heterogeneity of practitioner experience and specialty, clinical location, patient population, and study outcomes (e.g., first attempt success vs view of the vocal cords). Heterogeneity among specialty was considered present when there were differences in training background across anesthesia, intensive care, emergency, or prehospital. Heterogeneity in experience was considered present where medical students, learners, or trainees were grouped with consultant practitioners. Heterogeneity in location was considered present when the location of airway management differed (e.g., operating room, emergency department, intensive care, or critical care settings or prehospital). Pediatric patients were defined as < 18 yr of age. A difficult airway was defined as a known difficult intubation based on previous records or suspected difficult airway based on clinical considerations. Preferable study outcomes were those that were patient-centred (e.g., first-pass tracheal intubation success) vs surrogate (e.g., view of the glottis).
Data were abstracted using a uniform data collection form by one author (A.D.). Meta-analyses found were reviewed by all authors and any question as to inclusion or exclusion of retrieved meta-analyses was discussed amongst all authors (A.D., L.V.D., J.A.L.) on regular video-conference meetings. Percentages and proportions of primary and secondary outcomes were then tabulated. As this was a systematic review of published meta-analyses, the risk of bias could not be assessed.
Results
Of the 83 potentially eligible publications identified, 21 meta-analyses met our criteria (flow diagram, Fig. 2). Of the 21 meta-analyses, the majority (16/21; 76%) combined HA-VL and Mac-VL blade types and did not account for the dissimilarities of these blade types in their findings.7,8,9,12,14,17,18,20,22,23,24,25,26,28,29,32 Heterogeneity in clinical experience was found in most meta-analyses (20/21; 95%).7,8,9,10,14,16,17,18,20,22,23,24,25,26,28,29,30,32,33,34 Heterogeneity of practitioner specialty (prehospital, emergency, intensive care, or anesthesia) occurred in 15 of the 21 (71%) meta-analyses.7,8,9,10,14,16,17,18,22,23,24,25,26,28,34 Heterogeneity across locations (e.g., prehospital, emergency, intensive care, and operating theatre) occurred in ten of the 21 (48%) meta-analyses.8,9,10,16,17,23,24,28,30,34 Only one of the 21 (5%) meta-analyses focused on a relatively homogeneous patient population, that of adult patients with known difficult airways.12 Adult and pediatric patient populations were combined (or not defined) in five of the 21 (24%) meta-analyses.25,26,28,29,30 The primary outcomes of individual meta-analyses varied with the most common being first attempt tracheal intubation success, present in seven of the 21 (33%) studies.17,18,20,22,23,26,30 Findings of heterogeneity of primary and secondary outcomes can be found in Table 1.
Discussion
The primary objective of our systematic review identified that the majority of meta-analyses (16/21; 76%) combined HA-VL and Mac-VL blade types in their comparison with Mac-DL. Combining VL blade types in meta-analysis risks an overall result that may not accurately apply to both HA-VL and Mac-VL blade types. This could mislead the clinician seeking to determine which VL is best to employ for an individual patient. For example, the Cochrane meta-analysis published by Lewis et al. in 2016 concluded that VL reduced failed tracheal intubations, compared with DL.18 Nevertheless, a subgroup analysis of only the HA-VL studies did not reach the same conclusion. Given the recommendations for and widespread adoption of VL-guided intubation, it is time to untangle such confounders (Table 2).
Videolaryngoscopes are available with a variety of blade shapes. Many VL blades are hyper-angulated or hyper-curved, with an overall angulation of around 60°. Mac-VL blades are also available, with an angulation along the blade, as with Mac-DL, of closer to 30°35 (Fig. 1). These two distinct blade types require two distinct techniques for use. Mac-VL, like its Mac-DL counterpart, involves sweeping the tongue from right to left and lifting the sublingual tissues, allowing either a direct line-of-sight view, or a view of the larynx on the video screen. In contrast, HA-VL blades are designed to pass down the midline of the tongue. The camera on the HA-VL blade “looks around the corner” to the larynx, often producing a better laryngeal view than that afforded by Mac-DL. The 60° anterior curvature attains an “indirect view” of the larynx as it can generally only be visualized on the video screen.
Unlike its Mac-DL counterpart, an improved laryngeal view obtained using HA-VL does not necessarily translate to improved first-pass tracheal intubation success. The more acute angle of HA-VL also requires more acute angulation of the tracheal tube to traverse the oropharynx to the larynx. This angulation is generally created by use of a rigid or malleable stylet within the tracheal tube. Once through the glottis, the endotracheal tube tip may abut the anterior tracheal wall at an almost perpendicular angle, making further endotracheal tube passage difficult. This is often experienced by many airway managers—i.e., the ability to see the glottis on screen yet the inability to pass the endotracheal tube (Fig. 2).
Although this study analyzed combining HA-VL and Mac-VL in meta-analyses, the current landscape of blade types is further complicated by an array of VL blades between these two extremes; these are the intermediate-angled blades. For example, the McGrath “Mac” blade has a curvature between that of a true Macintosh (30°) and a hyperangulated (60°) blade (Fig. 3). These intermediate blades may also confound the results of meta-analyses; their unique curvature should be considered distinct to Mac-VL blades.
One of the striking findings of this systematic review was the mixing of experience among airway managers (from learners to experienced consultants) that occurred in all but one meta-analysis (20/21; 95%). This is problematic because stated findings of a meta-analysis might not then apply to all clinicians. The clinical location where VL was employed was also mixed in eight (38%) and undefined in two (10%), leaving readers uncertain of whether the findings can be applied to their clinical practice.
Heterogeneity was also present in the patient populations with only one meta-analysis having dealt with patients with known difficult airways.12 This likely means that patients with known difficult airways were mixed throughout the remaining meta-analyses. The most successful laryngoscope to use in this subset of challenging patients currently eludes the airway practitioner. There is value in delineating the most successful laryngoscope in patients with known difficult airways since the best device may be different to that in patients without difficult airways. Additionally, adult and pediatric patient populations were combined or not defined in five of the 21 (24%) publications. As a result, it is unclear if the findings of these meta-analyses can be extended to both adults and children.
Among the 21 retrieved meta-analyses there were a variety of primary outcomes, in addition, eight meta-analyses (38%) did not define a primary outcome. First-pass success, now being recognized as an important determinant to avoid complications and patient harm,36 was defined as the primary outcome in seven (33%) meta-analyses, and was the most common primary outcome. Other primary outcomes of the meta-analyses included view of the vocal cords, time to tracheal intubation, overall success, hemodynamic changes at 60-sec post-tracheal intubation, airway complications, and difficult or failed tracheal intubation with varied definitions. We suggest future research focus on primary patient-centred outcomes such as first-pass tracheal intubation success and patient harm.
An additional specific source of heterogeneity to consider is the use of neuromuscular blocking agents. Neuromuscular blockade is associated with more effective face mask ventilation37 and tracheal intubation.38 Therefore, mixing primary studies without controlling for neuromuscular blocking agent use is a potential confounder.
Comparison of VL vs the Miller blade or combinations of Miller and Macintosh blades also occurs. We excluded four meta-analyses involving the Miller blade from our systematic review.11,15,19,21 Of note, three of these four were pediatric studies,11,15,19 highlighting the heterogeneity related to Macintosh and Miller blades in the pediatric airway literature. As a straight blade, Miller blade DL is generally different from the Mac-DL technique. Therefore, DL should be defined as Mac-DL where appropriate.
There are other variables that likely display similar heterogeneity to the variables measured in our study (e.g., definition of difficult airway, time to intubation, VL brand). For reasons of practicality, we chose to focus on the five pre-specified variables. Additionally, we acknowledge that our data set excluded five Japanese-language publications and as such may omit relevant data.
Our study findings highlight the heterogeneity appearing in meta-analyses comparing Mac-DL and VL. There is mounting momentum towards VL use, yet there is no clear answer as to what the best VL device is to use for patients and settings. Currently, it is reasonable to match the expected airway anatomy to that of the blade type (e.g., selecting HA-VL for patients with known or expected difficult Mac-DL).
In conclusion, although most currently published meta-analyses suggest a superiority of VL to DL, many do not clearly offer meaningful information on which type of VL blade (Mac-VL or HA-VL) the findings pertain to. Other sources of heterogeneity in these meta-analyses further limit their applicability. Future meta-analyses of VL studies should ask targeted questions with adequately compared devices among specific patient groups. For example, one class of VL blade (e.g., Mac-VL or HA-VL, but not both combined) should be compared with Mac-DL. In settings evolving towards universal VL use, future studies could focus on different blade types on the same VL system. Additionally, homogeneity should extend across the airway manager population (e.g., novice vs experienced practitioners), the patient population (e.g., reassuring or non-reassuring patient airway anatomy), and clinical context (emergency vs elective intubation). Finally, the outcome should be clinically relevant, the most useful being successful tracheal intubation (e.g., first attempt success) rather than surrogate outcomes such as time to intubation or the view of the vocal cords. Attention to the avoidance of heterogeneity in meta-analyses through carefully considered study methodology has the potential to better inform optimal clinical practice.
References
Frerk C, Mitchell VS, McNarry AF, et al. Difficult Airway Society 2015 guidelines for management of unanticipated difficult intubation in adults. Br J Anaesth 2015; 115: 827-48.
Higgs A, McGrath BA, Goddard C, et al. Guidelines for the management of tracheal intubation in critically ill adults. Br J Anaesth 2018; 120: 323-52.
Cook TM, El-Boghdadly K, McGuire B, McNarry AF, Patel A, Higgs A. Consensus guidelines for managing the airway in patients with COVID-19. Anaesthesia 2020; DOI:https://doi.org/10.1111/anae.15054.
Australian Society of Anaesthetists. Airway Management Guidelines. Anaesthesia and caring for patients during the COVID-19 outbreak. Available from URL: https://asa.org.au/covid-19-updates/ (accessed November 2020).
Hall D, Steel A, Heij R, Eley A, Young P. Videolaryngoscopy increases ‘mouth-to-mouth’ distance compared with direct laryngoscopy. Anaesthesia 2020; DOI:https://doi.org/10.1111/anae.15047.
Cooper RM. Implementing universal videolaryngoscopy: how to do it and what to expect. Br J Anaesth 2018; 120: 13-5.
Hoshijima H, Denawa Y, Tominaga A, Nakamura C, Shiga T, Nagasaka H. Videolaryngoscope versus Macintosh laryngoscope for tracheal intubation in adults with obesity: a systematic review and meta-analysis. J Clin Anesth 2018; 44: 69-75.
Hoshijima H, Mihara T, Maruyama K, et al. C-MAC videolaryngoscope versus Macintosh laryngoscope for tracheal intubation: a systematic review and meta-analysis with trial sequential analysis. J Clin Anesth 2018; 49: 53-62.
Hoshijima H, Mihara T, Maruyama K, et al. McGrath videolaryngoscope versus Macintosh laryngoscope for tracheal intubation: A systematic review and meta-analysis with trial sequential analysis. J Clin Anesth 2018; 46: 25-32.
Hoshijima H, Kuratani N, Hirabayashi Y, Takeuchi R, Shiga T, Masaki E. Pentax Airway Scope® vs Macintosh laryngoscope for tracheal intubation in adult patients: a systematic review and meta-analysis. Anaesthesia 2014; 69: 911-8.
Abdelgadir IS, Phillips RS, Singh D, Moncreiff MP, Lumsden JL. Videolaryngoscopy versus direct laryngoscopy for tracheal intubation in children (excluding neonates). Cochrane Database Syst Rev 2017; DOI:https://doi.org/10.1002/14651858.CD011413.pub2.
Pieters BM, Maas EH, Knape JT, Van Zundert AA. Videolaryngoscopy vs. direct laryngoscopy use by experienced anaesthetists in patients with known difficult airways: a systematic review and meta-analysis. Anaesthesia 2017; 72: 1532-41.
Suppan L, Tramèr MR, Niquille M, Grosgurin O, Marti C. Alternative intubation techniques vs Macintosh laryngoscopy in patients with cervical spine immobilization: systematic review and meta-analysis of randomized controlled trials. Br J Anaesth 2016; 116: 27-36.
De Jong A, Molinari N, Conseil M, et al. Video laryngoscopy versus direct laryngoscopy for orotracheal intubation in the intensive care unit: a systematic review and meta-analysis. Intensive Care Med 2014; 40: 629-39.
Sun Y, Lu Y, Huang Y, Jiang H. Pediatric video laryngoscope versus direct laryngoscope: a meta-analysis of randomized controlled trials. Paediatr Anaesth 2014; 24: 1056-65.
Griesdale DE, Liu D, McKinney J, Choi PT. Glidescope® video-laryngoscopy versus direct laryngoscopy for endotracheal intubation: a systematic review and meta-analysis. Can J Anesth 2012; 59: 41-52.
Arulkumaran N, Lowe J, Ions R, Mendoza M, Bennett V, Dunser MW. Videolaryngoscopy versus direct laryngoscopy for emergency orotracheal intubation outside the operating room: a systematic review and meta-analysis. Br J Anaesth 2018; 120: 712-24.
Bhattacharjee S, Maitra S, Baidya DK. A comparison between video laryngoscopy and direct laryngoscopy for endotracheal intubation in the emergency department: a meta-analysis of randomized controlled trials. J Clin Anesth 2018; 47: 21-6.
Lingappan K, Arnold JL, Fernandes CJ, Pammi M. Videolaryngoscopy versus direct laryngoscopy for tracheal intubation in neonates. Cochrane Database Syst Rev 2018; DOI:https://doi.org/10.1002/14651858.CD009975.pub3.
Liu TT, Li L, Wan L, Zhang CH, Yao WL. Videolaryngoscopy vs. Macintosh laryngoscopy for double-lumen tube intubation in thoracic surgery: a systematic review and meta-analysis. Anaesthesia 2018; 73: 997-1007.
Rombey T, Schieren M, Pieper D. Video versus direct laryngoscopy for inpatient emergency intubation in adults. Dtsch Arztebl Int 2018; 115: 437-44.
Huang HB, Peng JM, Biao X, Liu GY, Du B. Video laryngoscopy for endotracheal intubation of critically ill adults: a systematic review and meta-analysis. Chest 2017; 152: 510-7.
Jiang J, Ma D, Li B, Yue Y, Xue F. Video laryngoscopy does not improve the intubation outcomes in emergency and critical patients - a systematic review and meta-analysis of randomized controlled trials. Crit Care 2017; DOI:https://doi.org/10.1186/s13054-017-1885-9.
Lewis SR, Butler AR, Parker J, Cook TM, Smith AF. Videolaryngoscopy versus direct laryngoscopy for adult patients requiring tracheal intubation. Cochrane Database Syst Rev 2016; DOI:https://doi.org/10.1002/14651858.CD011136.pub2.
Savino PB, Reichelderfer S, Mercer MP, Wang RC, Sporer KA. Direct versus video laryngoscopy for prehospital intubation: a systematic review and meta-analysis. Acad Emerg Med 2017; 24: 1018-26.
Zhao BC, Huang TY, Liu KX. Video laryngoscopy for ICU intubation: a meta-analysis of randomised trials. Intensive Care Med 2017; 43: 947-8.
Carlson JN, Brown CA 3rd. Does the use of video laryngoscopy improve intubation outcomes? Ann Emerg Med 2014; 64: 165-6.
Lee YK, Chen CC, Wang TL, Lin KJ, Su YC. Comparison of video and direct laryngoscope for tracheal intubation in emergency settings: a meta-analysis. J Acute Med 2012; 2: 43-9.
Su YC, Chen CC, Lee YK, Lee JY, Lin KJ. Comparison of video laryngoscopes with direct laryngoscopy for tracheal intubation: a meta-analysis of randomised trials. Eur J Anaesthesiol 2011; 28: 788-95.
Lu Y, Jiang H, Zhu YS. Airtraq laryngoscope versus conventional Macintosh laryngoscope: a systematic review and meta-analysis. Anaesthesia 2011; 66: 1160-7.
Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 2009; https://doi.org/10.1136/bmj.b2535.
Jiang J, Ma DX, Li B, Wu AS, Xue FS. Videolaryngoscopy versus direct laryngoscopy for nasotracheal intubation: a systematic review and meta-analysis of randomised controlled trials. J Clin Anesth 2019; 52: 6-16.
Hoshijima H, Maruyama K, Mihara T, Mieda T, Shiga T, Nagasaka H. Airtraq® reduces the hemodynamic response to tracheal intubation using single-lumen tubes in adults compared with the Macintosh laryngoscope: a systematic review and meta-analysis of randomized control trials. J Clin Anesth 2018; 47: 86-94.
Mihai R, Blair E, Kay H, Cook TM. A quantitative review and meta-analysis of performance of non-standard laryngoscopes and rigid fibreoptic intubation aids. Anaesthesia 2008; 63: 745-60.
Nishikawa K. Understanding the original shape of the Macintosh laryngoscope. J Anesth Clin Res 2014; DOI:https://doi.org/10.4172/2155-6148.1000387.
Sakles JC, Chiu S, Mosier J, Walker C, Stolz U. The importance of first pass success when performing orotracheal intubation in the emergency department. Acad Emerg Med 2013; 20: 71-8.
Soltész S, Alm P, Mathes A, Hellmich M, Hinkelbein J. The effect of neuromuscular blockade on the efficiency of facemask ventilation in patients difficult to facemask ventilate: a prospective trial. Anaesthesia 2017; 72: 1484-90.
Lundstrøm LH, Duez CH, Nørskov AK, et al. Effects of avoidance or use of neuromuscular blocking agents on outcomes in tracheal intubation: a Cochrane systematic review. Br J Anaesth 2018; 120: 1381-93.
Author contributions
Andrew W. Downey, Laura V. Duggan, and J. Adam Law contributed to all aspects of this manuscript, including study conception and design; acquisition, analysis, and interpretation of data; and drafting the article.
Disclosures
None.
Funding statement
None.
Editorial responsibility
This submission was handled by Dr. Hilary P. Grocott, Former Editor-in-Chief, Canadian Journal of Anesthesia.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix Systematic review search strategy
Appendix Systematic review search strategy
# | Search statement | Results |
|---|---|---|
1 | direct laryngoscop*.mp. | 2338 |
2 | Meta-Analysis as Topic/ or meta-analys*.mp. | 177819 |
3 | videolaryngoscop*.mp. | 1047 |
4 | video laryngoscop*.mp. | 965 |
5 | Laryngoscopy.mp. or exp LARYNGOSCOPY/ | 15759 |
6 | exp Video Recording/ | 39054 |
7 | 3 or 4 or 6 | 40329 |
8 | Laryngoscopy/ or Laryngoscopes/ | 14089 |
9 | 1 or 8 | 15032 |
10 | 3 or 4 or 6 | 40329 |
11 | 1 or 8 | 15032 |
12 | 1 and 2 and 10 | 17 |
13 | 10 and 11 | 2268 |
14 | limit 13 to (english language and yr=“2000 -Current”) | 1813 |
15 | limit 14 to meta analysis | 21 |
16 | 3 or 4 | 1941 |
17 | 1 and 16 | 463 |
18 | limit 17 to (english language and yr=“2000 -Current”) | 425 |
19 | limit 18 to meta analysis | 14 |
20 | 8 and 10 | 2151 |
21 | limit 20 to (english language and yr=“2000 -Current”) | 1707 |
22 | limit 21 to meta analysis | 21 |
23 | 2 and 20 | 30 |
24 | limit 23 to (english language and yr=“2000 -Current”) | 26 |
25 | Glidescope.mp. | 592 |
26 | Macintosh.mp. | 1904 |
27 | 25 or 26 | 2333 |
28 | 2 and 27 | 24 |
29 | limit 28 to (english language and yr=“2000 -Current”) | 17 |
30 | limit 29 to meta analysis | 14 |
31 | limit 27 to meta analysis | 21 |
32 | limit 31 to (english language and yr=“2000 -Current”) | 14 |
33 | c-mac.mp. | 196 |
34 | mcgrath.mp. | 338 |
35 | 25 or 26 or 33 or 34 | 2669 |
36 | limit 35 to (yr=“2000 -Current” and meta analysis) | 22 |
37 | from 32 keep 1-14 | 14 |
38 | from 36 keep 1-22 | 22 |
39 | 2 and 35 | 26 |
40 | 1 or 5 or 8 or 26 | 18541 |
41 | 3 or 4 or 6 or 25 or 33 or 34 | 40707 |
42 | 40 and 41 | 2683 |
43 | 2 and 42 | 34 |
44 | Pentax Airway Scope.mp. or exp flexible laryngoscope/ | 43 |
45 | 25 or 33 or 34 or 44 | 1085 |
46 | 1 or 26 | 3969 |
47 | 45 and 46 | 442 |
48 | limit 47 to (english language and meta analysis and yr=“2000 -Current”) | 8 |
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Downey, A.W., Duggan, L.V. & Adam Law, J. A systematic review of meta-analyses comparing direct laryngoscopy with videolaryngoscopy. Can J Anesth/J Can Anesth 68, 706–714 (2021). https://doi.org/10.1007/s12630-021-01921-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-021-01921-7