Abstract
Background
Closing the gap between child mortality in low- and middle-income countries (LMICs) and high-income countries is a priority set by the WHO in sustainable development goals (SDGs). We aimed to examine poor nutrition and prenatal and postnatal care that could increase the risk of child mortality in LMICs.
Methods
The Demographic and Health Survey (DHS) was used to examine data from 26 countries to compare prenatal, postnatal, nutritional, and demographic factors across LMICs. Outcome of child death was classified into death before one month of age, between 1 to 11 months, between one to two years, between three to five years, and overall death before five years. Chi-square analyses identified differences in prenatal care, postnatal care, nutrition, and demographic factors between children who died and those who survived. Logistic regression identified factors that increased child mortality risk.
Results
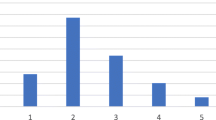
The majority of deaths occurred before the ages of one month and one year. Considerably poorer quality of prenatal care, postnatal care, and nutrition were found in low-income and low-middle-income countries in the contemporary 2020s. High child mortality and poor quality of prenatal and postnatal care coincide with low income. Children in LMICs were exposed to less vitamin A-rich foods than children in higher-middle-income countries. The use of intestinal parasite drugs and the absence of postpartum maternal vitamin A supplementation significantly increased child mortality risk. Significant socio-demographic risk factors were associated with an increased mortality rate in children, including lack of education, maternal marital status, family wealth index, living rurally, and financial problems hindering access to healthcare.
Conclusions
Poor nutrition remains a vital factor across all LMICs, with numerous children being exposed to foods low in iron and vitamin A. Significantly, most deaths occur in neonates and infants, indicating an urgent need to address risk factors associated with early child death.


Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author upon reasonable request.
References
UNICEF. Under-five mortality. 2021. https://data.unicef.org/topic/child-survival/under-five-mortality/. Accessed 22 July, 2022.
Perin J, Mulick A, Yeung D, Villavicencio F, Lopez G, Strong KL, et al. Global, regional, and national causes of under-5 mortality in 2000&2013;19: an updated systematic analysis with implications for the Sustainable Development Goals. Lancet Child Adolesc Health. 2022;6:106–15.
Arntzen A, Moum T, Magnus P, Bakketeig LS. Marital status as a risk factor for fetal and infant mortality. Scand J Soc Med. 1996;24:36–42.
Chytil F, Vitamin A. Deficiency: health, survival and vision. Am J Clin Nutr. 1997;65:173–4.
Unicef. Fed to Fail?: The Crisis of Children’s Diets in Early Life: 2021 Child Nutrition Report. 2021. https://data.unicef.org/wp-content/uploads/2021/09/Fed-to-Fail-FULL-REPORT-Child-Nutrition-Report-2021-FINAL.pdf. Accessed 22 July, 2022.
Leslie HH, Spiegelman D, Zhou X, Kruk ME. Service readiness of health facilities in Bangladesh, Haiti, Kenya, Malawi, Namibia, Nepal, Rwanda, Senegal, Uganda and the United Republic of Tanzania. Bull World Health Organ. 2017;95:738–48.
Kiross GT, Chojenta C, Barker D, Tiruye TY, Loxton D. The effect of maternal education on infant mortality in Ethiopia: a systematic review and meta-analysis. PLoS ONE. 2019;14:e0220076.
Lartey ST, Khanam R, Takahashi S. The impact of household wealth on child survival in Ghana. J Health Popul Nutr. 2016;35:38.
Tunçalp Ӧ, Pena-Rosas J, Lawrie T, Bucagu M, Oladapo O, Portela A, et al. WHO recommendations on antenatal care for a positive pregnancy experience—going beyond survival. BJOG Int J Obstet Gynaecol. 2017;124:860–2.
Abu-Ouf NM, Jan MM. The impact of maternal iron deficiency and iron deficiency anemia on child’s health. Saudi Med J. 2015;36:146–9.
Rodríguez-Morales AJ, Barbella RA, Case C, Arria M, Ravelo M, Perez H, et al. Intestinal parasitic infections among pregnant women in Venezuela. Infect Dis Obstet Gynecol. 2006;2006:23125.
Walia B, Kmush BL, Lane SD, Endy T, Montresor A, Larsen DA. Routine deworming during antenatal care decreases risk of neonatal mortality and low birthweight: A retrospective cohort of survey data. PLOS Negl Trop Dis. 2021;15:e0009282.
Elliott AM, Ndibazza J, Mpairwe H, Muhangi L, Webb EL, Kizito D, et al. Treatment with anthelminthics during pregnancy: what gains and what risks for the mother and child? Parasitology. 2011;138:1499–507.
King CL. Is ivermectin safe in pregnancy? Lancet Glob Health. 2020;8:e12–3.
Salam RA, Mansoor T, Mallick D, Lassi ZS, Das JK, Bhutta ZA. Essential childbirth and postnatal interventions for improved maternal and neonatal health. Reprod Health. 2014;11:S3.
World Health Organization. WHO recommendations on antenatal care for a positive pregnancy experience. 2016. https://www.who.int/publications/i/item/9789241549912. Accessed 22 July, 2022.
World Health Organization. Vitamin A supplements: a guide to their use in the treatment of vitamin A deficiency and xerophthalmia/prepared by a WHO/UNICEF/IVACG task force. 1997. https://apps.who.int/iris/handle/10665/41947. Accessed 22 July, 2022.
Martin CR, Ling PR, Blackburn GL. Review of infant feeding: key features of breast milk and infant formula. Nutrients. 2016;8:279.
World Health Organization. Guideline: vitamin A supplementation in postpartum women. 2011. https://apps.who.int/iris/handle/10665/44623. Accessed 22 July, 2022.
Oliveira-Menegozzo JM, Bergamaschi DP, Middleton P, East CE. Vitamin A supplementation for postpartum women. Cochrane Database Syst Rev. 2010;3:Cd005944.
Gannon BM, Jones C, Mehta S. Vitamin A Requirements in Pregnancy and Lactation. Curr Dev Nutr. 2020;4:nzaa142.
Vitamin A supplementation: who, when and how. Community Eye Health J. 2013;26:71.
Schoeps A, Lietz H, Sié A, Savadogo G, De Allegri M, Müller O, et al. Health insurance and child mortality in rural Burkina Faso. Glob Health Action. 2015;8:27327.
Sosnaud B. Inequality in infant mortality: cross-state variation and medical system institutions. Soc Probl. 2017;66:108–27.
Bennett T, Braveman P, Egerter S, Kiely JL. Maternal marital status as a risk factor for infant mortality. Fam Plann Perspect. 1994;26:271.
World Bank Country and Lending Groups, 2022. https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups. Accessed 22 July, 2022.
de Silva NR, Sirisena JL, Gunasekera DP, Ismail MM, de Silva HJ. Effect of mebendazole therapy during pregnancy on birth outcome. Lancet. 1999;353:1145–9.
Gannon BM, Rogers LM, Tanumihardjo SA. Metabolism of neonatal vitamin A supplementation: a systematic review. Adv Nutr. 2021;12:942–58.
Asif MF, Pervaiz Z, Afridi JR, Safdar R, Abid G, Lassi ZS. Socio-economic determinants of child mortality in Pakistan and the moderating role of household’s wealth index. BMC Pediatr. 2022;22:3.
Arsenault C, Jordan K, Lee D, Dinsa G, Manzi F, Marchant T, et al. Equity in antenatal care quality: an analysis of 91 national household surveys. Lancet Glob Health. 2018;6:e1186–95.
Kiross GT, Chojenta C, Barker D, Loxton D. The effects of health expenditure on infant mortality in sub-Saharan Africa: evidence from panel data analysis. Health Econ Rev. 2020;10:5.
Lambon-Quayefio M, Owoo NS. Determinants and the impact of the National Health Insurance on neonatal mortality in Ghana. Health Econ Rev. 2017;7:34.
Acknowledgements
Dataset analysed in this study was collected by the Demographic and Health Survey (DHS) program.
Funding
No funding was obtained for this study.
Author information
Authors and Affiliations
Contributions
LK: conceptualization, formal analysis, writing–original draft. CS: visualization, writing–original draft. SJ: supervision, writing–review and editing.
Corresponding author
Ethics declarations
Conflict of interest
No financial or non-financial benefits have been received or will be received from any party related directly or indirectly to the subject of this article.
Ethical approval
Open dataset from the Demographic and Health Survey (DHS) was used, permission was provided to the principal supervisor and all collaborators for use, so no ethics application was required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lin, K., Chern, S. & Sun, J. Mapping the quality of prenatal and postnatal care and demographic differences on child mortality in 26 low to middle-income countries. World J Pediatr 19, 835–850 (2023). https://doi.org/10.1007/s12519-022-00668-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12519-022-00668-5