Abstract
Introduction
For individuals with lumbar spinal stenosis (LSS), minimally invasive procedures such as an interspinous spacer device without decompression or fusion (ISD) or open surgery (i.e., open decompression or fusion) may relieve symptoms and improve functions when patients fail to respond to conservative therapies. This research compares longitudinal postoperative outcomes and rates of subsequent interventions between LSS patients treated with ISD and those with open decompression or fusion as their first surgical intervention.
Methods
This retrospective, comparative claims analysis identified patients age ≥ 50 years with LSS diagnosis and with a qualifying procedure during 2017–2021 in the Medicare database which includes healthcare encounters in inpatient and outpatient settings. Patients were followed from the qualifying procedure until end of data availability. The outcomes assessed during the follow-up included subsequent surgical interventions, including subsequent fusion and lumbar spine surgeries, long-term complications, and short-term life-threatening events. Additionally, the costs to Medicare during a 3-year follow-up were calculated. Cox proportional hazards, logistic regression, and generalized linear models were used to compare outcomes and costs, adjusted for baseline characteristics.
Results
A total of 400,685 patients who received a qualifying procedure were identified (mean age 71.5 years, 50.7% male). Compared to ISD patients, patients receiving open surgery (i.e., decompression and/or fusion) were more likely to have a subsequent fusion [hazard ratio (HR), 95% confidence intervals (CI): 1.49 (1.17, 1.89)–2.54 (2.00, 3.23)] or other lumbar spine surgery [HR (CI): 3.05 (2.18, 4.27)–5.72 (4.08, 8.02)]. Short-term life-threatening events [odds ratio (CI): 2.42 (2.03, 2.88)–6.36 (5.33, 7.57)] and long-term complications [HR (CI): 1:31 (1.13, 1.52)–2.38 (2.05, 2.75)] were more likely among the open surgery cohorts. Adjusted mean index costs were lowest for decompression alone (US$7001) and highest for fusion alone ($33,868). ISD patients had significantly lower 1-year complication-related costs than all surgery cohorts and lower 3-year all-cause costs than fusion cohorts.
Conclusions
ISD resulted in lower risks of short- and long-term complications and lower long-term costs than open decompression and fusion surgeries as a first surgical intervention for LSS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Multiple treatments are available for patients with symptomatic lumbar spinal stenosis, ranging from minimally invasive procedures to more invasive surgical options; however, few investigations have compared the postoperative outcomes of procedures in a real-world setting. |
This study sought to longitudinally compare the rates of safety events and subsequent spinal surgeries of patients who received interspinous devices (without decompression or fusion) versus patients treated with either open decompression or fusion as their first surgical intervention. |
What was learned from the study? |
Compared with patients who received open surgery, those treated with interspinous devices were less likely to have a subsequent fusion or other lumbar spine surgery. |
Patients who were treated with interspinous devices had lower rates of short- and long-term complications than open decompression or fusion surgery as well as lower long-term costs than fusion surgery. |
Introduction
Lumbar spinal stenosis (LSS) is a condition that affects 1 out of 10 people in the general population and nearly half of those over the age of 60 years [1, 2]. A common presentation of LSS is neurogenic intermittent claudication (NIC), manifesting as pain, numbness, and/or subjective weakness in the back and legs with difficulty walking [3]. The goal of treatment is to relieve symptoms and improve function, where the first-line treatment for these symptoms is typically categorized as being “conservative” and includes physical therapy, pain medication, and/or epidural injections [3].
Patients who fail to respond to these modalities may be appropriate candidates for minimally invasive procedures such as the placement of stand-alone interspinous devices (ISD) without a direct decompression or fusion [4]. These spacers are inserted posteriorly between the spinous processes and bring about an “indirect” decompression of the neural elements by limiting lumbar extension, a position known to decrease the cross-sectional area of the spinal canal, and which can exacerbate symptoms of neurogenic claudication. Studies have shown patients receiving ISDs exhibit reductions in pain and improvements in both function and quality of life [4,5,6,7]. In addition, minimally invasive strategies such as ISDs may be a good option for patients with medical comorbidities or other contraindications for surgery [8].
Depending upon the pathology, the surgical treatment for patients with LSS may involve decompression to remove bony or soft tissue structures that may be contributing to the stenosis , a fusion to stabilize the spine, or both procedures [3]. However, lumbar fusion is a more invasive operation that may not result in better outcomes relative to decompression alone, and is associated with an increased risk of complications and adverse events [9]. ISDs are indicated to treat skeletally mature patients with NIC who have undergone at least 6 months of non-operative treatment, and are implanted at one or two adjacent lumbar levels from L1 to L5 [10]. The minimally-invasive nature of ISDs may reduce rehabilitation time compared to more invasive surgical procedures [11], although some have reported higher re-operation rates for ISDs compared with traditional decompression surgery [12].
While there are previous studies that utilize large databases or prospective studies to compare outcomes between decompression and fusion [13, 14], there is currently a paucity of real-world data directly comparing the outcomes of patients treated with ISDs without decompression or fusion with patients treated with conventional surgical options for lumbar stenosis. Previous works have compared decompression/fusion surgery to an ISD that requires decompression [15] and to an ISD that is no longer available for use [16, 17]. However, controlled trials require strict inclusion and exclusion criteria, potentially limiting their generalizability to wider use in real-world practice. Additionally, while the safety and efficacy of the most recently approved ISD have previously been established [18, 19], no studies have directly compared postoperative outcomes and subsequent interventions between patients treated with the currently approved ISD and those treated with either open decompression and/or fusion as their first surgical treatment for LSS. Thus, the primary objectives of this longitudinal study were to compare the rates of safety events and rates of subsequent spinal surgeries of patients who received an ISD compared to either open decompression (with or without concomitant fusion) or fusion alone as their first operative intervention, using the most recent real-world claims data available.
Methods
Study Design and Data Source
This study is a retrospective cohort analysis comparing postoperative complications, rates of subsequent interventions, and costs between patients receiving an implant of ISD and patients treated with open decompression without fusion, open decompression with fusion, and fusion surgeries as their first surgical intervention. This analysis used claims data from the 100% Medicare Standard Analytical Files (SAFs), which include enrollment, demographic, and encounter data for Medicare beneficiaries. Specifically, these data reflect encounters that occur in either the inpatient or outpatient setting such as an inpatient hospital, outpatient hospital, skilled nursing facility, and home health services, but the SAFs do not include pharmacy data, even for beneficiaries with Medicare medication coverage. Sample selection and the creation of analytic variables were performed using the Instant Health Data software (Panalgo, Boston, MA, USA). Statistical analyses were generated using StataCorp 2021 (College Station, TX, USA). This study does not involve human participants, so neither independent review board approval nor patient consent was required. We had permission to access and analyze the data used in this study through the CMS Data Use Agreement.
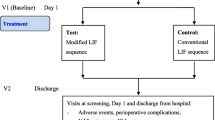
The study was longitudinal in nature such that an index date was created for each patient when they were first treated with placement of an ISD, decompression, or fusion between January 1, 2017 and December 31, 2021. Patients were followed from their index date until the end of the study period, the end of their Medicare coverage, or death, whichever occurred first. Patient demographic and clinical characteristics were identified during a baseline period of 12 months prior to the index date.
Study Population and Outcome Measures
Health encounters in the SAFs include patient diagnoses and procedures that are documented using the International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM) or Procedure Coding System (ICD-10-PC) codes and Current Procedural Terminology 4th edition (CPT) and Healthcare Common Procedure Coding System (HCPCS) codes, respectively. These data reflect information from beneficiaries with Part A/B coverage but not those covered by Medicare Part C (MA).
Patients were included if they had at least one claim for an ISD, open decompression, or spinal fusion during the study period (codes included in Supplementary Material Table 1); were at least 50 years of age as of the index date with at least 12 months of continuous enrollment with Medicare coverage during the baseline period; and had a diagnosis of LSS during the study period. However, individuals who had undergone prior lumbar spine surgeries during the baseline period were excluded from the analysis.
During the follow-up period, subsequent spinal interventions specific to LSS were evaluated as well as those related to other spinal conditions. Subsequent surgical interventions for LSS included ISD, minimally invasive lumbar decompression (i.e., MILD), open decompression with or without fusion, fusion alone, and placement of an interspinous spacer with an open decompression. Other surgical interventions included removal of implants from the lumbar spine (whether or not they were related to the index procedure), insertion of a spinal cord stimulator or drug delivery device, and other lumbar spine surgeries consisting of disc procedures, endoscopic decompressions, repair of a cerebrospinal fluid leak, vertebral excision, and cement augmentation of vertebral bodies (i.e., vertebroplasty, kyphoplasty). Furthermore, a re-operation was defined as having an open decompression, fusion, and or device removal within 3 months of the index procedure [11].
Safety events included any postoperative complications and/or life-threatening events. Long-term complications were evaluated during the follow-up period, including mechanical complications of a device, allergic reaction to an implant, injury to the lumbosacral spine or nerve root, cerebrospinal fluid leak, wound infection or dehiscence, hematoma, thrombophlebitis, and closed/collapsed lumbar fracture, including those involving the spinous process. Life-threatening events relevant to surgical operations [20,21,22,23] were evaluated within 30 days of the index procedure, and included sepsis, pneumonia, cardiac arrest, pulmonary embolism, deep venous thrombosis, ischemic stroke, acute myocardial infarction, blood transfusions related to blood loss, and inpatient re-admission. Readmission due to postoperative or life-threatening complications occurring up to 3 months after the index procedure was also reported (codes included in Supplementary Material Table 1).
Healthcare costs included the costs associated with the index procedure, all-cause (i.e., those incurred from all medical services) for up to 3 years, and any complications for up to 1 year after the index procedure. The costs were adjusted for inflation using the medical care component of the Consumer Price Index and standardized to 2021 US dollars [24].
Statistical Analysis
The baseline characteristics available for each patient included demographics (i.e., age, gender, race, geographic region), Elixhauser comorbidity index score [25], and relevant clinical conditions (codes included in S1). Categorical variables are presented as the count and percent of patients in each category, while continuous variables are recorded as mean and standard deviation (SD). Cox proportional hazards regression was used to examine the times to several events, including subsequent open surgery (decompression and/or fusion), and any long-term complication, adjusted for baseline characteristics. Logistic regression was used to examine the likelihood of suffering a life-threatening event within 30 days of the index procedure, a 90-day re-admission due to a complication, and a 90-day re-operation, adjusted for the baseline characteristics. Generalized linear models with a gamma log-link were employed to compare costs between cohorts. An alpha of 0.05 was used to signal statistical significance.
Results
Study Population
A total of 400,685 subjects were identified, including 4183 (1.0%) who received placement of an ISD, 211,014 (52.7%) treated with decompression alone, 76,935 (19.2%) treated with decompression with a concomitant fusion, and 108,553 (27.1%) who received a fusion alone. The average length of follow-up was 19.4 months for the ISD patients and 24.9–31.4 months for the decompression and/or fusion patients. Compared with the decompression and/or fusion patients, patients who received ISD were older (p < 0.0001 vs. all three surgery groups) with a higher comorbidity burden as evidenced by a higher Elixhauser score (p < 0.0001 vs. all groups) and increased prevalence of several comorbidities including hypertension, osteoarthritis, diabetes, obesity, chronic obstructive pulmonary disease, atrial fibrillation, osteoporosis, and congestive heart failure (Table 1).
Subsequent Spinal Surgeries
Adjusted Cox models revealed that patients in the surgery cohorts were 1.5–2.5 times more likely to have a subsequent fusion [hazard ratio (HR) 95% confidence intervals (CI): 1.49 (1.17, 1.89)–2.54 (2.00, 3.23), all p ≤ 0.001] compared to those who had been treated with an ISD (Table 2). The patients in the surgery cohorts were also more likely to have undergone other lumbar spine surgeries [HR (CI): 3.05 (2.18, 4.27)–5.72 (4.08, 8.02), all p < 0.001], but less likely to have a drug delivery implant [HR (CI): 0.41 (0.28, 0.61)–0.44 (0.30, 0.66), all p < 0.001]. The patients in the decompression without fusion cohort was 1.3 times more likely to have a subsequent decompression [HR (CI): 1.26 (1.05, 1.50), p = 0.011], but those in the fusion cohorts were less likely to have had a subsequent decompression [HR (CI): 0.47 (0.39, 0.57)–0.56 (0.47, 0.67), p < 0.001] compared to patients who received an ISD. Patients in the fusion cohorts were also 6.4–6.5 times more likely to have undergone a subsequent surgery for removal of an implant [HR (CI): 6.37 (4.64, 8.73)–6.54 (4.77–8.96), p < 0.001].
Among patients with ≥ 3 months of follow-up, the re-operation rates at 3 months were 1.7%, 1.6%, and 2.5% for the decompression, decompression with fusion, and fusion cohorts, respectively, which were significantly higher than the 0.6% re-operation rate observed for the ISD cohort (all p < 0.001) (Table 3). Adjusted logistic regression confirmed the patients in the decompression cohorts (with or without fusion) were 2.6–2.8 times more likely to have a re-operation at 3 months than those in the ISD cohort [odds ratio (OR) (CI): 2.62 (1.74, 3.93)–2.77 (1.85, 4.15), all p < 0.001], whereas the re-operation rate for the fusion cohort was 3.9 times greater [OR (CI): 3.90 (2.60, 5.84), p < 0.001] (Fig. 1). Full model results are presented in Supplementary Material Table 2.
Safety Outcomes
Adjusted logistic regression showed patients that received decompression and fusion were 2.4–6.4 times more likely to experience a life-threatening complication within 30 days compared with those who received ISD [OR (CI): 2.42 (2.03, 2.88)–6.36 (5.33, 7.57), all p < 0.001] (Fig. 1), driven primarily by re-admission and blood loss associated with fusion procedures (Table 3). The long-term unadjusted incidence rates of any complication (per 10,000 person-years) were 280.3 for ISD versus 264.4 for decompression alone, 489.1 for decompression with fusion, and 469.6 for fusion alone. The rates of closed/collapsed lumbar vertebra fractures including those specifically involving the spinous process fracture were 94.2, 98.8, 173.3, and 174.5 for ISD, decompression alone and with fusion, and fusion alone, respectively. Patients in the decompression and fusion cohorts were 1.3–2.4 times more likely to have a long-term complication [OR (CI): 1.31 (1.13, 1.52)–2.38 (2.05, 2.75), all p < 0.001] and 1.6–3.0 times more likely to have sustained a spinous process fracture [OR (CI): 1.61 (1.25, 2.06)–3.03 (2.36, 3.89), all p < 0.001] (Fig. 1).
The rates of re-admission due to any complication at 3 months was 1.3% for the ISD cohort, which was lower than that of the surgery cohorts (2.2% for decompression, 3.7% for decompression with fusion, and 4.0% for fusion, Table 3). Adjusted logistic regression also revealed that compared to ISD cohort, patients who received decompression were 2.0 times [OR (CI): 1.98 (1.50, 2.62), p < 0.001] and those receiving decompression with fusion and only fusion were 3.6–3.9 times [OR (CI): 3.62 (2.73, 4.79)–3.86 (2.92, 5.10), all p < 0.001] more likely to have a re-admission due to a complication (Fig. 1; Supplementary Material Table 3).
Cost Outcomes
Adjusted mean index costs [standard deviation (SD)] ranged from $7001 ($1105) for decompression alone to $33,868 ($5392) for fusion alone, with ISD [$12,742 ($2069)] and decompression plus fusion [$32,488 ($5102)] falling within that range. The average 1-year costs of decompression plus fusion [$17,039 ($8762)] and fusion alone [$18,506 ($9534)] were statistically significantly higher than that recorded for the ISD cohort [$14,232 ($7681)] (both p < 0.001, Table 4 and Supplementary Material Table 4); however, the average 1-year costs for patients who received decompression alone [$12,344 ($6200)] were not statistically different from those who received ISD (p = 0.760). A similar pattern was also observed for the 3-year costs. The complication-related costs for the first year were lowest in ISD patients [mean $655 ($282)] and significantly higher for all three surgical cohorts (means ranging from $1487 ($714) to $7888 ($4051), p < 0.001].
Discussion
Compared with patients who received open surgery (i.e., decompression and/or fusion) as a treatment for symptomatic LSS, patients who received ISD were less likely to receive a subsequent fusion or other lumbar spine operation, but were more likely to be treated with an ISD/MILD procedure. Not surprisingly, both short- and long-term complications were more frequently observed among the open surgery cohorts. The costs of the index procedure were highest for surgeries involving a fusion and lowest for decompression alone. Placement of an ISD was associated with lower 1-year complication-related and 3-year all-cause costs. Given the large sample size and geographically diverse sample over a lengthy follow-up period, these results represent meaningful findings, given the heterogeneity observed in the approaches adopted by clinicians to treat LSS.
Few published studies in the literature have directly compared the use of ISD to lumbar decompression and/or fusion for LSS. A retrospective cohort analysis of LSS patients treated with decompression surgery with or without fusion documented 90-day re-operation and re-admission rates of 4.7% and 7.2%, respectively [26]. Similarly, a Medicare claims study of subjects who had undergone a lumbar fusion between 2005 and 2009 reported that 10.9% had a re-operation at 3 months and the re-admission rate for complications during that period was 11.1% [27]. In contrast, the current analysis revealed lower 3-month re-operation and re-admission rates for patients who received open surgery and ISD. The incidence of re-operation at 3 months was 0.6% for ISD patients, which was lower than the 1.6–2.5% observed for patients who received decompression and/or fusion surgery. These rates reflect re-operations on the same or a different level of the spine, which cannot be separated due to the lack of clinical information in claims data; thus, the true re-operation rate on the index level is at most 2.5% and may be lower if some of the re-operations were performed at a different level. Likewise, the re-admission rate due to a complication was also lower among the patients treated with an ISD (1.3%) compared to the surgery cohorts (2.2–4.0%).
Multiple systematic reviews and meta-analyses have attempted to compare decompression alone versus decompression with fusion. Chang et al. (2017) concluded that performing a concomitant fusion produced no clinical improvements relative to decompression alone over 2 years of follow-up but gave rise to a higher risk of complications, longer operative times, and greater blood loss [28]. Shen et al. (2022) evaluated a series of patients with LSS with degenerative spondylolisthesis and found the addition of a fusion resulted in similar clinical results compared to decompression alone but was associated with poorer safety outcomes [29].
The strengths of this study include the large and geographically diverse dataset with relatively lengthy follow-ups, as well as the use of multiple methods to compare the incidence and risk of various events. However, several limitations should be acknowledged, including those inherent to these types of claims analyses, such as the potential for coding or data entry errors and the omission of details not needed to justify payment. For instance, diagnosis codes identified in claims data lack the clinical information such as the severity of LSS or postoperative complications, so the severity of LSS at the time of index procedure could not be determined, nor could outcomes be examined by severity. Additionally, the inability of claims to capture imaging data or patient-reported outcomes, such as visual or numeric pain scores and the Zurich Claudication Questionnaire, make it impossible to assess the efficacy of the procedure. Furthermore, this analysis is limited to individuals with Medicare coverage, so they may not be generalizable to other patients; however, this may be less of a concern because the vast majority of symptomatic LSS cases are adults aged 65 years and older who generally have Medicare coverage.
Conclusions
This analysis indicates that an implantation of ISD was safer than decompression and/or fusion surgeries as a first surgical treatment for LSS, due to lower rates of short- and long-term complications. Patients who received an ISD had lower costs 3 years after intervention and were less likely to require a subsequent fusion when compared to patients who received an open decompression alone, open decompression with fusion, or fusion surgery. Future investigations on clinical data, opioid and pain-related medication use, and healthcare utilizations would provide additional understanding of how spinal procedures impact the healthcare system and patient outcomes.
References
Jensen RK, Jensen TS, Koes B, Hartvigsen J. Prevalence of lumbar spinal stenosis in general and clinical populations: a systematic review and meta-analysis. Eur Spine J. 2020;29(9):2143–63.
Kalichman L, Cole R, Kim DH, Li L, Suri P, Guermazi A, et al. Spinal stenosis prevalence and association with symptoms: the Framingham Study. Spine J. 2009;9(7):545–50.
Deer T, Sayed D, Michels J, Josephson Y, Li S, Calodney AK. A review of lumbar spinal stenosis with intermittent neurogenic claudication: disease and diagnosis. Pain Med. 2019;20(Suppl 2):S32-s44.
Bini W, Miller LE, Block JE. Minimally invasive treatment of moderate lumbar spinal stenosis with the superion interspinous spacer. Open Orthop J. 2011;5:361–7.
Nunley PD, Deer TR, Benyamin RM, Staats PS, Block JE. Interspinous process decompression is associated with a reduction in opioid analgesia in patients with lumbar spinal stenosis. J Pain Res. 2018;11:2943–8.
Nunley PD, Patel VV, Orndorff DG, Lavelle WF, Block JE, Geisler FH. Interspinous process decompression improves quality of life in patients with lumbar spinal stenosis. Minim Invasive Surg. 2018;2018:1035954.
Shabat S, Miller LE, Block JE, Gepstein R. Minimally invasive treatment of lumbar spinal stenosis with a novel interspinous spacer. Clin Interv Aging. 2011;6:227–33.
Hartman J, Granville M, Jacobson RE. The use of vertiflex(r) interspinous spacer device in patients with lumbar spinal stenosis and concurrent medical comorbidities. Cureus. 2019;11(8): e5374.
Deyo RA, Mirza SK, Martin BI, Kreuter W, Goodman DC, Jarvik JG. Trends, major medical complications, and charges associated with surgery for lumbar spinal stenosis in older adults. JAMA. 2010;303(13):1259–65.
US Department of Health and Human Services; US Food and Drug Administration. Premarket approval (PMA): Superion Interspinous Spacer. fda.gov; 2015.
Cairns K, Deer T, Sayed D, van Noort K, Liang K. Cost-effectiveness and safety of interspinous process decompression (Superion). Pain Med. 2019;20(Suppl 2):S2–8.
Wu AM, Zhou Y, Li QL, Wu XL, Jin YL, Luo P, et al. Interspinous spacer versus traditional decompressive surgery for lumbar spinal stenosis: a systematic review and meta-analysis. PLoS ONE. 2014;9(5): e97142.
Försth P, Ólafsson G, Carlsson T, Frost A, Borgström F, Fritzell P, et al. A randomized, controlled trial of fusion surgery for lumbar spinal stenosis. N Engl J Med. 2016;374(15):1413–23.
Lurie JD, Tosteson TD, Tosteson A, Abdu WA, Zhao W, Morgan TS, et al. Long-term outcomes of lumbar spinal stenosis: eight-year results of the spine patient outcomes research trial (SPORT). Spine (Phila Pa 1976). 2015;40(2):63–76.
Davis RJ, Errico TJ, Bae H, Auerbach JD. Decompression and coflex interlaminar stabilization compared with decompression and instrumented spinal fusion for spinal stenosis and low-grade degenerative spondylolisthesis: two-year results from the prospective, randomized, multicenter, food and drug administration investigational device exemption trial. Spine (Phila Pa 1976). 2013;38(18):1529–39.
Strömqvist BH, Berg S, Gerdhem P, Johnsson R, Möller A, Sahlstrand T, et al. X-stop versus decompressive surgery for lumbar neurogenic intermittent claudication: randomized controlled trial with 2-year follow-up. Spine (Phila Pa). 2013;38(17):1436–42.
Zhao XW, Ma JX, Ma XL, Li F, He WW, Jiang X, et al. Interspinous process devices (IPD) alone versus decompression surgery for lumbar spinal stenosis (LSS): a systematic review and meta-analysis of randomized controlled trials. Int J Surg. 2017;39:57–64.
Nunley PD, Patel VV, Orndorff DG, Lavelle WF, Block JE, Geisler FH. Superion interspinous spacer treatment of moderate spinal stenosis: 4-year results. World Neurosurg. 2017;104:279–83.
Tekmyster G, Sayed D, Cairns KD, Raso LJ, Kim C, Block JE. Interspinous process decompression with the Superion(R) spacer for lumbar spinal stenosis: real-world experience from a device registry. Med Devices (Auckl). 2019;12:423–7.
Canet J, Mazo V. Postoperative pulmonary complications. Minerva Anestesiol. 2010;76(2):138–43.
Manekk RS, Gharde P, Gattani R, Lamture Y. Surgical complications and its grading: a literature review. Cureus. 2022;14(5): e24963.
Vogel TR, Dombrovskiy VY, Carson JL, Graham AM, Lowry SF. Postoperative sepsis in the United States. Ann Surg. 2010;252(6):1065–71.
Wang MF, Li FX, Feng LF, Zhu CN, Fang SY, Su CM, et al. Development and validation of a novel risk assessment model to estimate the probability of pulmonary embolism in postoperative patients. Sci Rep. 2021;11(1):18087.
US Bureau of Labor Statistics. Consumer Price Index Databases 2023. Available from https://www.bls.gov/cpi/data.htm
Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27.
Ilyas H, Golubovsky JL, Chen J, Winkelman RD, Mroz TE, Steinmetz MP. Risk factors for 90-day re-operation and readmission after lumbar surgery for lumbar spinal stenosis. J Neurosurg Spine. 2019;31(1):20–6.
Ong KL, Auerbach JD, Lau E, Schmier J, Ochoa JA. Perioperative outcomes, complications, and costs associated with lumbar spinal fusion in older patients with spinal stenosis and spondylolisthesis. Neurosurg Focus. 2014;36(6):E5.
Chang W, Yuwen P, Zhu Y, Wei N, Feng C, Zhang Y, et al. Effectiveness of decompression alone versus decompression plus fusion for lumbar spinal stenosis: a systematic review and meta-analysis. Arch Orthop Trauma Surg. 2017;137(5):637–50.
Shen Z, Guan X, Wang R, Xue Q, Zhang D, Zong Y, et al. Effectiveness and safety of decompression alone versus decompression plus fusion for lumbar spinal stenosis with degenerative spondylolisthesis: a systematic review and meta-analysis. Ann Transl Med. 2022;10(12):664.
Acknowledgements
Funding
The study was sponsored by Boston Scientific. The rapid service fee and the open access fee are funded by Boston Scientific.
Medical Writing and/or Editorial Assistance
Editorial assistance in the preparation of this article was provided by Craig Solid and Ally Pachelli of Solid Research Group. Support for this assistance was funded by Boston Scientific.
Author Contributions
Oth Tran, Peter Whang, and Howard Rosner contributed to the design and implementation of the research, to the review of the descriptive and multivariate results, and to the writing of the draft and final version of the manuscript. Oth Tran constructed the dataset and analyzed the outcomes.
Disclosures
Oth Tran is a full-time employee of BSC. Peter Whang and Howard Rosner were not compensated for their participation in this study and have no competing interests to declare.
Compliance with Ethics Guidelines
This study does not involve human participants, so neither independent review board approval nor patient consent was obtained. We had permission to access and analyze the data used in this study through the CMS Data Use Agreement.
Data Availability
The datasets generated during and/or analyzed during the current study are not publicly available due to the CMS Data Use Agreement. These data are available to any entity who can meet CMS's criteria regarding the study purpose and the ability to house and manage the fully de-identified data.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Whang, P.G., Tran, O. & Rosner, H.L. Longitudinal Comparative Analysis of Complications and Subsequent Interventions Following Stand-Alone Interspinous Spacers, Open Decompression, or Fusion for Lumbar Stenosis. Adv Ther 40, 3512–3524 (2023). https://doi.org/10.1007/s12325-023-02562-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-023-02562-6