Abstract
Introduction
The current study describes real-world clinical outcomes and factor usage among patients with haemophilia B switching from standard half-life factor IX (SHL FIX) treatment to recombinant factor IX Fc fusion protein (rFIXFc) prophylaxis in European treatment centres.
Methods
This non-interventional, retrospective, multicentre chart review evaluated medical records from adult and paediatric patients with haemophilia B in Denmark, Germany and the UK. Patients had documented SHL FIX treatment, on-demand or prophylaxis, for ≥ 6 months before starting rFIXFc prophylaxis, and subsequent data for ≥ 6 months afterwards (up to 24 months). Primary endpoints included annualised bleeding rates (ABRs), prophylactic factor consumption and injection frequency.
Results
Data from 30 patients (24/30 [80.0%] with severe disease) showed overall mean (standard deviation, SD) ABRs of 4.7 (6.3) on SHL FIX treatment and 1.7 (2.3) after switching to rFIXFc prophylaxis. The reduction in mean (SD) ABRs was greater when switching from SHL FIX on-demand treatment (n = 6), with a decrease from 10.5 (9.9) to 2.6 (4.5), than when switching from SHL FIX prophylaxis (n = 24), with a decrease from 3.3 (4.3) to 1.5 (1.4). Among prior SHL FIX prophylaxis patients, switching to rFIXFc prophylaxis increased the proportion of those with zero bleeds from 21.7% to 45.8% during the 6 months before and after switching, respectively. In the total population, five of six target joints (83.3%) present when patients started rFIXFc prophylaxis subsequently resolved. In patients switching from SHL FIX prophylaxis to rFIXFc prophylaxis, mean (SD) weekly injection frequency was reduced by 1.0 (0.7) and mean (SD) factor consumption was reduced by 27.7 (49.6) IU/kg/week.
Conclusion
This study demonstrates the effectiveness of rFIXFc prophylaxis in real-world clinical practice. Improvements in both clinical effectiveness and factor usage associated with rFIXFc prophylaxis may potentially reduce patient burden and improve quality of life.
Similar content being viewed by others
Why carry out this study? |
As clinical trials evaluate drugs in an environment that controls for external ‘real-life’ factors, they are limited by, for example, restrictions in the study population and mandated dose/treatment intervals. |
Data on the effectiveness and usage of recombinant factor IX Fc fusion protein (rFIXFc) prophylaxis in patients with haemophilia B in the real-world clinical setting are beneficial to add to efficacy data from clinical trials. |
What was learned from the study? |
The current study describes clinical outcomes and factor usage among patients with haemophilia B switching from standard half-life factor IX (SHL FIX) treatment to rFIXFc prophylaxis in European treatment centres. |
During rFIXFc prophylaxis, compared to previous SHL FIX treatment, patients had reduced bleeding, with consequent benefits for joints; factor consumption and injection frequency were reduced compared to prior SHL FIX prophylaxis. |
These real-word data demonstrate the effectiveness of rFIXFc prophylaxis for up to 24 months, in line with results from clinical trials. |
Introduction
Severe haemophilia B is characterised by frequent and spontaneous bleeding episodes primarily affecting joints and muscles; repeated bleeds can lead to haemophilic arthropathy, progressive chronic joint damage and overall reduced quality of life (QoL) [1]. Impaired QoL will disrupt many aspects of a patient’s life [2], and evidence showing lower than optimal QoL in those with haemophilia B highlights unmet needs in the management of such individuals [3].
For those with severe haemophilia B, as well as patients with moderate haemophilia and a severe bleeding phenotype, prophylaxis is the standard of care, aiming to prevent bleeds, maintain musculoskeletal health and benefit QoL [1]. However, prophylaxis with standard half-life (SHL) factor IX (FIX) therapies requires frequent injections, imposing an inherent burden that can affect treatment adherence [1]. Recombinant FIX (rFIX) products that exhibit an extended half-life can maintain higher factor levels for longer periods of time and provide prolonged protection from bleeding [4]. One such product is rFIX Fc fusion protein (rFIXFc)—approved for the treatment and prophylaxis of bleeding in patients with haemophilia B in all age groups [5, 6].
Data from the pivotal phase 3 trials, B-LONG [7] (ClinicalTrials.gov identifier NCT01027364) and Kids B-LONG (ClinicalTrials.gov identifier NCT01440946) [8], have demonstrated the efficacy and safety of rFIXFc in both adult and paediatric patients. Results from the B-LONG study showed rFIXFc to have a prolonged half-life compared with rFIX (82.1 vs 17.0 h in individuals aged ≥ 12 years) [7], with consequent reduced injection frequency when switching from prophylaxis with conventional products [9]. Prophylaxis with rFIXFc significantly reduced annualised bleeding rates (ABRs) compared to on-demand treatment (P < 0.001), and one injection was able to resolve the majority of bleeding episodes (90.4%) [7]. Improved bleed protection allows a more active lifestyle with reduced pain [10]. Both studies involved previously treated patients with no detected inhibitors, and adverse events were consistent with those expected in the general haemophilia population [7, 8].
The long-term efficacy and safety of rFIXFc were subsequently confirmed in the B-YOND extension study (Clinicaltrials.gov identifier NCT01425723), which enrolled subjects completing the B-LONG and Kids B-LONG trials, who received cumulative (range) treatment durations of 5.2 (0.7–6.5) and 3.4 (0.9–4.8) years, respectively [11]. ABRs remained low with extended dosing intervals throughout this follow-up. In addition, B-LONG data also showed rFIXFc to provide effective bleed control in patients with haemophilia B undergoing minor and major surgeries [7]. The PUPs B-LONG trial [12] (Clinicaltrials.gov identifier NCT02234310) demonstrated the product to be well tolerated, with an adverse event profile, including hypersensitivity and inhibitor formation, to be similar to that expected in previously untreated patients with haemophilia B; rFIXFc was effective for prophylaxis and bleed treatment in this previously untreated population.
Clinical trials evaluate drugs in an environment that controls for external ‘real-life’ factors and, as such, are limited by, for example, restrictions in the study population and mandated dose/treatment intervals. Data on the real-world effectiveness and usage of rFIXFc prophylaxis in a clinical setting are beneficial to add to the evidence from clinical trials in routine clinical practice, and a number of real-world evaluations of rFIXFc have been performed [13,14,15,16,17,18,19,20].
The present study aimed to build on the current evidence that has demonstrated the efficacy of rFIXFc prophylaxis. It used real-world data from paediatric, adolescent and adult patients, reflecting the haemophilia B treated population, and facilitated extended assessment, with up to 24 months of follow-up. The study objectives were to describe clinical outcomes and factor usage for patients switching from SHL FIX to rFIXFc prophylaxis in haemophilia treatment centres (HTCs) in Europe.
Methods
Study Design
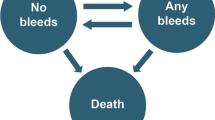
This was a non-interventional, retrospective, multicentre chart review based on the medical records of patients with haemophilia B who had switched from a SHL FIX therapy to rFIXFc prophylaxis. It was conducted in accordance with the Guidelines for Good Pharmacoepidemiology Practices issued by the International Society for Pharmacoepidemiology [21], with country-specific ethics committee/institutional review board/health authority approval obtained, as appropriate. Submissions involved the Regional Udvikling-Region Hovedstaden (Centre for Regional Development-Capital Region of Denmark) and the Regional Udvikling-Region Midtjylland (Centre for Regional Development-Central Denmark Region) in Denmark, the Ethics Committee at the Medical Faculty of the Rheinische Friedrich-Wilhelms-Universität Bonn in Germany, and the Health Research Authority (HRA) in the UK. Patient informed consent forms were required in Denmark and Germany, but, as the study was a retrospective patient chart review with anonymised data, not in the UK. In Denmark and Germany, patients received the informed consent forms together with information letters. Patients were asked for permission to use anonymised data from their medical records in the study. Completed forms were mandatory prior to data collection, before any data were accessed for study purposes.
Between July 2021 and February 2022, data were obtained from HTCs in Denmark, Germany and the UK. Data relating to a time period of at least 6 months (up to 12 months) prior to switching until at least 6 months after the switch (up to 24 months of rFIXFc prophylaxis, or until death or loss to follow-up, whichever occurred first) were collected for each patient.
Study Population
The study included adult and paediatric patients with a clinical diagnosis of haemophilia B who had documented treatment with SHL FIX, administered either on-demand or as prophylaxis, for at least 6 months prior to the time at which rFIXFc prophylaxis was initiated (the index date), and a further minimum of 6 months’ records thereafter.
Patients were excluded if their medical records were not available for review, they had FIX inhibitors (current or historic), or had received treatment for haemophilia B as part of an investigational medicinal product trial during the observation period.
Study Objectives
The objectives of the study were to describe real-world clinical outcomes and change in factor usage for patients switching from SHL FIX to rFIXFc prophylaxis; and describe the characteristics of patients switching. Primary endpoints evaluated ABRs, factor consumption and injection frequency, before and after switching from SHL FIX treatment to prophylaxis with rFIXFc. Secondary endpoints included annualised joint bleeding rates (AjBRs) and annualised spontaneous bleeding rates (AsBRs) before and after switching to rFIXFc prophylaxis. Other secondary endpoints were the duration of rFIXFc prophylaxis treatment together with change in ABR over time; target joint development and resolution; changes in injection frequency and factor consumption after switching to rFIXFc prophylaxis for those patients previously on SHL FIX prophylaxis. Target joints were defined on the basis of International Society on Thrombosis and Haemostasis criteria [22], being joints affected by at least three spontaneous bleeds over six consecutive months. Resolution was considered to have occurred if a target joint was subsequently affected by two or fewer bleeds over 12 consecutive months. Reasons for switching to rFIXFc prophylaxis were also collected. No safety data were obtained.
Statistical Analyses
The primary and secondary endpoints were summarised for the total population (including all countries). Data were also stratified by country, age group and according to the most recent SHL FIX regimen received prior to rFIXFc prophylaxis.
Descriptive statistics were used to provide summary data. Continuous data were summarised according to the number of observations, means, standard deviations (SD), medians, interquartile ranges (IQR), and maximum and minimum values. Categorical variables were summarised using counts and percentages.
Results
Patient Population
Data relating to a total of 31 patients were collected for this study, but one patient did not fulfill the inclusion criteria, having less than 6 months’ documented follow-up on rFIXFc, and was excluded from the analyses. Of the remaining 30 patients, 9 were from Denmark, 9 from Germany and 12 from the UK.
The characteristics of the study population are summarised in Supplementary Table 1.
Twenty-six patients were 12 years or older and four were between 0 and 11 years old. All patients were male and the majority 24/30 (80.0%) had severe disease. Most (24/30 [80.0%]) had previously received SHL FIX prophylaxis—the majority of these (20/24 [83.3%]) were treated twice a week (13/24 [54.2%]) or more often (7/24 [29.2%]); 4/24 patients (16.7%) were treated once a week. Six patients switched from previous SHL FIX on-demand treatment—most were at least 18 years of age (5/6 [83.3%]) and had severe haemophilia (5/6 [83.3%]).
The mean (SD) number of follow-up months during the pre-index period for the total population was 12.3 (3.6): 14.9 (0.1) in Denmark, 13.7 (1.6) in Germany and 9.3 (3.8) in the UK. The most frequently used product prior to switching was nonacog alfa (27/30 [90.0%] patients); the other patients (3/30 [10%]) had received plasma-derived FIX. The most common reasons for switching to rFIXFc prophylaxis were reduced injection frequency while maintaining protection from bleeds (22/30 patients [73.3%]), followed by improved protection from bleeds (18/30 patients [60.0%]). Adherence issues (2/30 patients [6.7%]) and difficulties with venous access (2/30 patients [6.7%]) were also indicated as reasons for switching, as was psychological stress related to injection frequency (1/30 patients [3.3%]). The mean (SD) number of follow-up months post-rFIXFc for the total population was 22.3 (3.2): 23.4 (1.7) in Denmark, 23.5 (1.5) in Germany and 20.8 (4.3) in the UK.
Clinical Outcomes
The median (IQR) ABRs before and after switching to rFIXFc prophylaxis for the total population (n = 30) were 2.0 (0.9, 6.5) and 1.0 (0.5, 2.0), respectively (Fig. 1). The mean (SD) ABR values for the total population were 4.7 (6.3) before switching and 1.7 (2.3) during rFIXFc prophylaxis, a reduction of 63.8%. The change in mean ABRs was greater in patients who switched from SHL FIX on-demand treatment (n = 6), with a 75.2% reduction (mean [SD] 10.5 [9.9] decreasing to 2.6 [4.5]), than in patients previously treated with SHL FIX prophylaxis (n = 24). However, a 54.5% reduction in mean ABR values after switching to rFIXFc was still reported in those who had previously received SHL FIX prophylaxis (mean [SD]) 3.3 [4.3] decreasing to 1.5 [1.4]).
Annualised bleeding rates (overall ABR, AjBR and AsBR) in patients (n = 30) before and after switching to rFIXFc prophylaxis. Box plots show medians with IQRs. Whiskers show maximum and minimum values. ABR annualised bleeding rate, AjBR annualised joint bleeding rate, AsBR annualised spontaneous bleeding rate, FIX factor IX, IQR interquartile range, rFIXFc recombinant factor IX Fc fusion protein, SHL standard half-life
AjBRs and AsBRs were also reduced or maintained after switching to rFIXFc (Fig. 1). For both outcomes, the mean values across all patients were reduced by 75.0% (mean [SD] values of 2.8 [5.5] and 2.0 [3.7], respectively, before switching, decreasing to 0.7 [0.9] and 0.5 [1.4], respectively).
Longitudinal results showed the benefits of rFIXFc prophylaxis over time (Supplementary Table 2). For the total population, the ABR between 12 and 24 months after switching to rFIXFc prophylaxis (n = 20) was lower than during the first 12 months of rFIXFc treatment (n = 30) (mean [SD] 1.1 [1.3] versus 2.2 [2.6]; median [IQR] 1.0 [0.0, 1.0] versus 1.5 [0.2, 3.0]).
Among patients who had previously received SHL FIX prophylaxis (n = 24), switching to rFIXFc prophylaxis increased the proportion of those with zero bleeds, from 21.7% (5/23) during the last 6 months prior to switching, up to 45.8% (11/24) during the following 6 months (Fig. 2). One patient, who had 5.9 months of previous SHL FIX treatment, was not included in the calculation of zero bleeds during the 6 months before switching.
Six target joints were present when patients started on rFIXFc prophylaxis (four in patients who had previously received on-demand therapy [elbow n = 2, wrist n = 1 and knee n = 1] and two in those previously treated with SHL FIX prophylaxis [ankle n = 2]). Five of these six (83.3%) target joints subsequently resolved within the follow-up period. The target joint that did not resolve was in the wrist of a patient previously treated with on-demand therapy; this patient also had a target joint in his elbow, which did resolve. No new target joints developed in patients on rFIXFc prophylaxis.
The clinical benefits of rFIXFc prophylaxis were observed consistently across countries (Table 1).
Factor Usage
In patients previously treated with SHL FIX prophylaxis (n = 24), after switching to rFIXFc prophylaxis, mean (SD) weekly injection frequency was reduced by 1.0 (0.7) and mean (SD) factor consumption was reduced by 27.7 (49.6) IU/kg/week (Table 1). Across age groups, mean (SD) weekly injection and factor consumption were reduced by 1.2 (0.3) and 13.4 (29.2) IU/kg/week, respectively, for patients aged less than 12 years (n = 3), versus 1.0 (0.7) and 127.5 (52.4) IU/kg/week, respectively, in those aged 12 years or older (n = 21).
Before switching, the mean (SD) weekly factor consumption for those on SHL FIX prophylaxis was 110.4 (59.8) IU/kg/week in Denmark (n = 7), 83.4 (67.6) IU/kg/week in Germany (n = 7) and 45.4 (21.5) IU/kg/week in the UK (n = 10) (Table 1). After switching, the mean (SD) factor consumption was reduced by 54.3 (60.0) IU/kg/week for patients in Denmark, 23.5 (63.0) IU/kg/week in Germany and 12.0 (20.3) IU/kg/week in the UK.
The mean (SD) annualised injection frequency was 106.4 (32.4) for patients receiving SHL FIX prophylaxis (n = 24) and 53.6 (9.9) during rFIXFc prophylaxis (n = 29). Mean (SD) values for annualised factor consumption were 3924.1 (2889.0) and 2393.7 (858.1) IU/kg/year, before and after switching, respectively.
For patients who had previously received SHL FIX prophylaxis, comparison of injection frequency before and at initiation of rFIXFc is shown in Fig. 3. Nearly all patients (23/24 [95.8%]) started with once-weekly dosing when switching to rFIXFc (Denmark 100.0% [7/7], Germany 100.0% [7/7] and the UK 90.0% [9/10]). One patient (1/24 [4.2%]), in the UK, received rFIXFc every 14 days at the time of switch. After patients switched to rFIXFc, considering the full follow-up period, injection frequency reduced for nearly all patients (20/24 [83.3%]), did not change for three patients (12.5%) and increased for one patient (4.2%) compared to prior SHL prophylaxis. The low injection frequency was maintained through to 18 to 24 months after switching (mean [SD] of 1.0 [0.3]) injections per week in the 20 patients being followed up at this point; Supplementary Table 2).
Discussion
The results of this study describe the real-world effectiveness of switching from SHL FIX therapies to rFIXFc prophylaxis in patients with haemophilia B, complementing results from clinical trials. The current data show that rFIXFc prophylaxis was effective in reducing bleeding rates in adult and paediatric patients previously treated with SHL FIX either on-demand or prophylactically (overall 63.8% reduction in mean values before and after switching). The most pronounced reduction in ABRs was seen in patients previously treated with SHL FIX on-demand (75.2% reduction in mean values before and after starting rFIXFc prophylaxis). Longitudinal data confirmed the effectiveness of rFIXFc prophylaxis for up to 24 months, with ABRs remaining low in all patients and a reduced injection frequency being maintained, in line with results from the B-YOND extension study [11].
Among patients who had previously received SHL FIX prophylaxis, switching to rFIXFc prophylaxis increased the proportion of those with zero bleeds. During rFIXFc prophylaxis, all but one of six pre-existing target joints resolved and no new target joints emerged.
Patients received fewer injections on rFIXFc prophylaxis than pre-switch on SHL prophylaxis (mean [SD] annualised values of 53.6 [9.9] and 106.4 [32.4], respectively) and had a reduction in factor consumption (mean [SD] annualised values of 2393.7 [858.1] and 3924.1 [2889.0] IU/kg/year, respectively). Country-specific data (albeit for small patient numbers, thereby precluding firm country-specific conclusions) showed that although rFIXFc consumption was lower in the UK than in Denmark and Germany, haemostatic benefits were apparent across all three countries.
Our results are in line with those from other real-word studies. For example, other retrospective analyses of patients with haemophilia B in the USA [17], Australia [19], each study involving 64 adult and paediatric patients, and a study in Ireland [14], evaluating data from 28 adult patients, have also considered the effects of switching to rFIXFc prophylaxis from previous FIX treatment, both prophylactic and on-demand. All three studies found switching to rFIXFc prophylaxis to reduce ABRs and factor consumption. Additional real-world data, evaluating treatment with rFIXFc or rFIX albumin fusion protein (rIX-FP) in the UK [20], rIX-FP in Italy, Belgium and the UK [23], as well as rIX-FP in Germany [24], and involving 20, 84 and 81 adult and paediatric patients with haemophilia B, respectively, have also shown the benefits of extended half-life FIX prophylaxis. This provided protection from bleeding, evaluated via ABR, while enabling reduced dosing frequency/lower product consumption.
In our study, around half of the patients who previously received SHL FIX prophylaxis were not on a regimen that would provide coverage for a whole week: 4/24 (16.7%) and 13/24 (54.2%) individuals were treated weekly and twice weekly, respectively. Only around one-fifth (21.7%) of the patients on SHL FIX prophylaxis experienced zero bleeds during the last 6 months of such treatment. Improved protection was a main reason for switching to rFIXFc prophylaxis and this was achieved, as evidenced by the decrease in ABR, the increase in proportion of patients with zero bleeds, and the resolution of target joints. These benefits were generally attained with decreased injection frequency and reduced factor consumption. The data show that intensified prophylaxis can be achieved with rFIXFc, an approach that is particularly warranted in patients with target joints, where the goal is to reduce inflammation.
With the extended half-life of rFIXFc permitting weekly or longer dosing intervals [5], this regimen can benefit those for whom more frequent injections may be discouraging and support the use of prophylaxis in some who need on-demand treatment. The decreased burden of treatment (i.e. reduced injection frequency) associated with rFIXFc prophylaxis compared to prophylaxis with SHL FIX products may help to improve patient adherence. Although this was not evaluated in the current study, previous real-world data have shown adherence to be an important consideration when physicians consider switching patients to rFIXFc [25], and that adherence rates improve after switching [17, 19]. Other previously published real-world data have shown that rFIXFc may help to improve QoL, not only as consequence of a reduced treatment burden but also by reducing pain and improving activities of daily living [13].
As a retrospective chart review study, potential limitations include selection bias arising from not including all eligible patients treated at the haemophilia centres involved, and bleeds not being accurately documented in medical records. Notably, as with other studies involving longitudinal data, patient numbers decreased over time, and the possibility of selective dropout should also be considered. The study had a relatively small sample size, which is particularly relevant when considering the paediatric data and longitudinal results towards the end of the post-index period, and additionally can affect endpoint comparison before and after switching. Given the small sample size, this was a descriptive study, with no statistical testing, and the results require cautious interpretation in relation to their generalisability to the wider population of individuals with haemophilia. As a retrospective study, data routinely collected in standard practice were analysed, but information pertaining to the clinical situation outside routine clinical practice did not fall within the scope of the study. Consequently, only the prescribed prophylactic factor consumption was recorded. Other product uses, such as for surgery, were excluded, and there were no data describing treatment of bleeds or QoL, which would be of interest for further research.
The strengths of the current study include the consideration of data from across three European countries, while the inclusion of paediatric, adolescent and adult patients reflects the treated haemophilia B population. The extended assessment period, with up to 24 months of follow-up, provided adequate time to observe changes in outcomes. In addition, real-world evidence provides information on outcomes observed in clinical practice beyond the restraints imposed by clinical trials.
Conclusion
Findings from this real-world study in patients with haemophilia B in Denmark, Germany and the UK demonstrate the long-term effectiveness of rFIXFc prophylaxis, in line with results from clinical trials. During rFIXFc prophylaxis patients exhibited numerically reduced ABRs compared to previous SHL FIX treatment (overall 63.8% reduction in mean values before and after switching), which were sustained over time; the proportion of patients with zero bleeds increased; all but one pre-existing target joint resolved and no new target joints emerged. In addition, numerical reductions in factor consumption and injection frequency were observed compared to previous prophylaxis with SHL FIX. Improvements in both clinical effectiveness and factor usage after switching from SHL FIX to rFIXFc prophylaxis have the potential to reduce patient burden and improve patients’ QoL.
References
Srivastava A, Santagostino E, Dougall A, et al. WFH guidelines for the management of hemophilia, 3rd edition. Haemophilia. 2020;26(Suppl. 6):1–158.
Buckner TW, Witkop M, Guelcher C, et al. Impact of hemophilia B on quality of life in affected men, women, and caregivers—assessment of patient-reported outcomes in the B-HERO-S study. Eur J Haematol. 2018;100(6):592–602.
Berntorp E, LeBeau P, Ragni MV, et al. Quality of life in a large multinational haemophilia B cohort (The B-Natural study)—unmet needs remain. Haemophilia. 2022;28(3):453–61.
Mannucci PM. Hemophilia therapy: the future has begun. Haematologica. 2020;105(3):545–53.
European Medicines Agency. Alprolix® Summary of Product Characteristics 2021. https://www.ema.europa.eu/en/documents/product-information/alprolix-epar-product-information_en.pdf. Accessed 23 Mar 2023.
Bioverativ Therapeutics Inc. Alprolix® Prescribing Information 2020. http://products.sanofi.us/Alprolix/alprolix.pdf. Accessed 23 Mar 2023.
Powell JS, Pasi KJ, Ragni MV, et al. Phase 3 study of recombinant factor IX Fc fusion protein in hemophilia B. N Engl J Med. 2013;369(24):2313–23.
Fischer K, Kulkarni R, Nolan B, et al. Recombinant factor IX Fc fusion protein in children with haemophilia B (Kids B-LONG): results from a multicentre, non-randomised phase 3 study. Lancet Haematol. 2017;4(2):e75–82.
Powell J, Shapiro A, Ragni M, et al. Switching to recombinant factor IX Fc fusion protein prophylaxis results in fewer infusions, decreased factor IX consumption and lower bleeding rates. Br J Haematol. 2015;168(1):113–23.
Astermark J, Hermans C, Ezzalfani M, et al. rFIXFc prophylaxis improves pain and levels of physical activity in haemophilia B: post hoc analysis of B-LONG using haemophilia-specific quality of life questionnaires. Haemophilia. 2022;28(1):18–26.
Pasi KJ, Fischer K, Ragni M, et al. Long-term safety and sustained efficacy for up to 5 years of treatment with recombinant factor IX Fc fusion protein in subjects with haemophilia B: results from the B-YOND extension study. Haemophilia. 2020;26(6):e262–71.
Nolan B, Klukowska A, Shapiro A, et al. Final results of the PUPs B-LONG study: evaluating safety and efficacy of rFIXFc in previously untreated patients with hemophilia B. Blood Adv. 2021;5(13):2732–9.
O’Donovan M, Quinn E, Johnston K, et al. Recombinant factor IX-Fc fusion protein in severe hemophilia B: patient-reported outcomes and health-related quality of life. Res Pract Thromb Haemost. 2021;5(7):e12602.
O’Donovan M, Bergin C, Quinn E, et al. Real-world outcomes with recombinant factor IX Fc fusion protein (rFIXFc) prophylaxis: longitudinal follow-up in a national adult cohort. Haemophilia. 2021;27(4):618–25.
O’Donovan M, Singleton E, Roche S, et al. Single centre, real-world experience of perioperative rFIXFc use in adult patients with haemophilia B undergoing major and minor surgery. Haemophilia. 2021;27(6):e690–7.
Lehtinen AE, Baghaei F, Astermark J, Holme PA. Surgical outcomes in patients with haemophilia A or B receiving extended half-life recombinant factor VIII and IX Fc fusion proteins: real-world experience in the Nordic countries. Haemophilia. 2022;28(5):713–9.
Shapiro A, Chaudhury A, Wang M, et al. Real-world data demonstrate improved bleed control and extended dosing intervals for patients with haemophilia B after switching to recombinant factor IX Fc fusion protein (rFIXFc) for up to 5 years. Haemophilia. 2020;26(6):975–83.
Peyvandi F, Garagiola I, Boscarino M, Ryan A, Hermans C, Makris M. Real-life experience in switching to new extended half-life products at European haemophilia centres. Haemophilia. 2019;25(6):946–52.
Brennan Y, Parikh S, McRae S, Tran H. The Australian experience with switching to extended half-life factor VIII and IX concentrates: on behalf of the Australian Haemophilia Centre Directors’ Organisation. Haemophilia. 2020;26(3):529–35.
Rampotas A, Desborough MJR, Raza-Burton S, et al. A single centre retrospective study of low dose prophylaxis with extended half-life factor IX for severe haemophilia B. Haemophilia. 2020;26(2):278–81.
International Society for Pharmacoepidemiology (ISPE). Guidelines for good pharmacoepidemiology practices (GPP). Revision 3: June 2015. https://www.pharmacoepi.org/resources/policies/guidelines-08027/. Accessed 23 Mar 2023.
Blanchette VS, Key NS, Ljung LR, Manco-Johnson MJ, van den Berg HM, Srivastava A. Definitions in hemophilia: communication from the SSC of the ISTH. J Thromb Haemost. 2014;12(11):1935–9.
Hermans C, Marino R, Lambert C, et al. Real-world utilisation and bleed rates in patients with haemophilia B who switched to recombinant factor IX fusion protein (rIX-FP): a retrospective international analysis. Adv Ther. 2020;37(6):2988–98.
Oldenburg J, Yan S, Maro G, Krishnarajah G, Tiede A. Assessing bleeding rates, related clinical impact and factor utilization in German hemophilia B patients treated with extended half-life rIX-FP compared to prior drug therapy. Curr Med Res Opin. 2020;36(1):9–15.
van der Sluijs M, Huyghe N, Wood C, Tawil S. A survey of physicians’ treatment switching practice in people on long-term prophylaxis for hemophilia in five European countries. Curr Med Res Opin. 2022;38(1):65–73.
Acknowledgements
Funding
The Kids B-LONG, B-LONG, and B-YOND studies were sponsored by Sobi and Sanofi. This analysis was funded by Sobi, who also funded the journal’s Rapid Service and Open Access Fees. Sobi and Sanofi reviewed and provided feedback on the manuscript.
Medical Writing and Editorial Assistance
Medical writing and editorial support, funded by Sobi, was provided by Andy Lockley, PhD, Bioscript Group, Macclesfield, UK, based on the authors’ input and direction, and in accordance with Good Publication Practice (GPP3) guidelines (http://www.ismpp.org/gpp3).
Authorship
All the authors of this article meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship and take responsibility for the integrity of the work as a whole. All the authors have given their approval for this version of the article to be published.
Author Contributions
Eva Funding, Gillian Lowe, Lone H Poulsen, Susan Shapiro and Johannes Oldenburg collected the data on which the study is based, contributed to the interpretation of the data, and directed the writing of the manuscript, reviewing the drafts for intellectual content and approving the final version of the article. Daniel Eriksson, Aletta Falk and Carly Rich contributed to the study concept/design and interpretation of the data, and directed the writing of the manuscript, reviewing the drafts for intellectual content and approving the final version of the article.
Disclosures
Eva Funding has received speakers fee from BMS and conference support from AOP orphan pharmaceuticals. Gillian Lowe has received honoraria for participating in educational events from Novartis, Leo, Sobi, Alexion, Takeda, Novo Nordisk and Sanofi. Lone H. Poulsen has received honoraria for educational activity from Sobi, speaker fees and meeting support from Novo Nordisk, as well as medical writing support from Bayer and Novo Nordisk for reporting clinical trials. Susan Shapiro has received conference support from Sobi, CSL Behring, Takeda; speaker fees from Sobi, Takeda, Roche; and participated in advisory boards for Sobi, Shire and Pfizer. Johannes Oldenburg reports receiving grants for studies and research from Bayer, Biotest, CSL Behring, Octapharma, Pfizer, Swedish Orphan Biovitrum and Takeda Pharmaceutical, and travel support as well as personal fees for lectures and advisory board meetings from Bayer, Biogen Idec, Biomarin, Biotest, CSL Behring, Chugai, Freeline, Grifols, Novo Nordisk, Octapharma, Pfizer, Roche, Sanofi, Sparks, Swedish Orphan Biovitrum and Takeda Pharmaceutical. Daniel Eriksson, Aletta Falk and Carly Rich are employees of Sobi. Aletta Falk is also a shareholder of Sobi.
Compliance with Ethics Guidelines
The study was conducted in accordance with the Guidelines for Good Pharmacoepidemiology Practices issued by the International Society for Pharmacoepidemiology, with country-specific ethics committee/institutional review board/health authority approval obtained, as appropriate. Submissions involved the Regional Udvikling – Region Hovedstaden (Centre for Regional Development – Capital Region of Denmark) and the Regional Udvikling – Region Midtjylland (Centre for Regional Development – Central Denmark Region) in Denmark, the Ethics Committee at the Medical Faculty of the Rheinische Friedrich-Wilhelms-Universität Bonn in Germany, and the Health Research Authority (HRA) in the UK. Patient informed consent forms were required in Denmark and Germany, but, as the study was a retrospective patient chart review with anonymised data, not in the UK.
Data Availability
The data sets analysed during the current study are available from the corresponding author on reasonable request. Sobi is committed to responsible and ethical sharing of data on the participant level and summary data for medicines and indications approved by the European Medicines Agency and/or Food and Drug Administration, while protecting individual participant integrity and compliance with applicable legislation. Data access will be granted in response to qualified research requests. All requests are evaluated by a cross‐functional panel of experts within Sobi and a decision on sharing will be based on the scientific merit and feasibility of the research proposal, maintenance of personal integrity and commitment to publication of the results. To request access to study data, a data sharing request form (available on www.sobi.com) should be sent to medical.info@sobi.com. Further information on Sobi’s data sharing policy and process for requesting access can be found at https://www.sobi.com/en/policies.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Funding, E., Lowe, G., Poulsen, L.H. et al. Real-World Effectiveness of rFIXFc Prophylaxis in Patients with Haemophilia B Switched from Standard Half-Life Therapy in Three European Countries. Adv Ther 40, 3770–3783 (2023). https://doi.org/10.1007/s12325-023-02559-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-023-02559-1