Abstract
Introduction
This ongoing post-marketing surveillance monitors the long-term safety and effectiveness of vedolizumab in routine clinical practice in patients with moderate-to-severe ulcerative colitis (UC) in Japan. This interim analysis assessed induction-phase data, covering the initial three doses of vedolizumab.
Methods
Patients were enrolled via a web-based electronic data capture system from approximately 250 institutions. Incidence of adverse events and treatment responses were assessed by the physicians after the patient had received three doses of vedolizumab or when the drug was discontinued, whichever occurred first. Therapeutic response was defined as any treatment response, including remission or improvement of complete or partial Mayo score, and was assessed in the total and stratified patient populations according to prior tumor necrosis factor alpha (TNFα) inhibitor treatments and/or baseline partial Mayo score.
Results
The total incidence of adverse drug reactions (ADRs) was 4.10% (11/268). Common ADRs were dizziness, nausea, and arthralgia, each reported in 0.75% of patients (2/268). Serious ADRs were herpes zoster oticus and UC, each reported in 0.37% of patients (1/268). Therapeutic response was reported in 84.5% (218/258) of all patients, 85.8% (127/148) of TNFα inhibitor-naïve patients, and 82.7% (91/110) of TNFα inhibitor-experienced patients. Among patients with partial Mayo score of ≥ 4 at baseline, partial Mayo score remission in patients without or with prior TNFα inhibitor treatment was 62.5% (60/96) and 45.6% (36/79), respectively.
Conclusion
The results confirm a safety and effectiveness profile of vedolizumab consistent with that observed in previous trials.
Clinical Trial Registration
JapicCTI-194603, NCT03824561.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Clinical trials have demonstrated the efficacy and safety of intravenously administered vedolizumab in patients with moderate-to-severe ulcerative colitis (UC) regardless of tumor necrosis factor alpha (TNFα) inhibitor exposure, but there is a lack of post-marketing surveillance data. |
This interim analysis of induction-phase data examined the effectiveness and safety of vedolizumab in Japanese patients with UC. |
What was learned from this study? |
The safety of vedolizumab was consistent with that reported in the clinical trials and no new safety signals were detected. |
The interim data showed that vedolizumab was effective in patients with moderate-to-severe active UC, regardless of prior TNFα inhibitor exposure. |
This is the largest post-marketing surveillance study to date on vedolizumab use in Asian patients with UC in routine clinical practice. |
Introduction
Ulcerative colitis (UC) is an inflammatory bowel disease characterized by repeated cycles of relapse and remission [1,2,3,4]. The primary goal of pharmacological treatment for UC is the induction and maintenance of remission [1, 2]. Biologic agents such as tumor necrosis factor (TNF) inhibitors, ustekinumab, and vedolizumab are recommended for the induction and maintenance of remission in patients with moderate-to-severe UC [1, 2, 4].
Vedolizumab is a recombinant humanized immunoglobulin G1 monoclonal antibody that binds specifically to α4β7 integrin on human lymphocytes [5, 6]. Vedolizumab inhibits invasion of inflammatory memory T cells by blocking binding of α4β7 integrin to its mucosal vascular addressin cell adhesion molecule 1 (MAdCAM-1) ligand on vascular endothelial cells in the intestine, thereby inhibiting intestinal inflammation through a gastrointestinal-selective immunoregulatory action that does not involve systemic immunosuppression [5, 6]. Clinical trials have demonstrated the efficacy and safety of intravenously administered vedolizumab in patients with moderate-to-severe UC [7,8,9] regardless of TNFα inhibitor exposure [10].
Within 4 years of vedolizumab first gaining marketing approval, more than 200,000 patient-years of vedolizumab exposure in the post-marketing setting had accumulated worldwide [11]. However, response to treatments for UC may vary across ethnic populations [8]. Although a study in Korea reported real-world effectiveness and safety outcomes of vedolizumab in patients with UC [12], post-marketing surveillance data for vedolizumab in Japanese patients is lacking.
The aim of this ongoing post-marketing surveillance study is to evaluate the long-term safety and effectiveness of intravenously administered vedolizumab, over 54 weeks, in patients with moderate-to-severe UC in routine clinical practice in Japan. Herein, we report results from an interim analysis, ahead of completion of the 54-week observation period, evaluating the safety and effectiveness of vedolizumab treatment during the induction phase after three doses of vedolizumab or when the drug was discontinued, in patients stratified by prior TNFα inhibitor treatment.
Methods
Study Setting and Data Collection
In this post-marketing surveillance study, patients with moderate-to-severe UC were enrolled centrally via a web-based electronic data capture system from approximately 250 institutions in Japan within 14 days after initiating treatment with vedolizumab. Participating investigators were asked to refer to medical records and other sources to complete case report forms for each patient. The patient data were entered in the electronic data capture system within a month after the third dose of vedolizumab at week 6 (in case report form 1) and within a month after completion of the 54-week observation period or after treatment discontinuation (in case report form 2). Collected data included baseline characteristics, treatment details (including use of vedolizumab, concomitant drugs, concomitant therapies, and surgical procedures), adverse events (AEs), presence/absence of treatment response, continuation of treatment, complete or partial Mayo score, a quality-of-life assessment, and laboratory tests. Severity of UC was defined according to the Evidence-based Clinical Practice Guidelines for Inflammatory Bowel Disease 2020 by the Japan Society of Gastroenterology [13]. Information on the patients’ race and ethnicity was not collected.
The study period started in February 2019 and runs until 31 October 2023. At the time of writing, data collection was ongoing. In this manuscript, we report results from the induction phase, as recorded in case report form 1. This interim analysis was planned to evaluate the safety and effectiveness of vedolizumab treatment during the induction phase, which was up to and including the third dose of vedolizumab.
This study was conducted in accordance with the Japanese guidelines for Good Post-Marketing Study Practice. In accordance with the Japanese regulations for post-marketing surveillance, it was not necessary to obtain institutional review board/ethics committee approval or written informed patient consent.
Prior to commencement, the study was registered with the Japan Pharmaceutical Information Center – Clinical Trials Information (JapicCTI-194603), as well as the National Institutes of Health Clinical Trial Registration System – ClinicalTrials.gov (NCT03824561), both of which have publicly accessible websites.
Patients and Treatment
Eligible patients had moderate-to-severe active UC (inclusion criterion), an inadequate response to conventional therapy (inclusion criterion), and no contraindications to vedolizumab (exclusion criterion).
The recommended dosage of vedolizumab for adults is 300 mg administered via intravenous infusion at 0, 2, and 6 weeks and every 8 weeks thereafter.
Outcome Measurements
Safety and effectiveness were assessed after patients received three doses of vedolizumab or when the drug was discontinued, whichever occurred first.
Measures of safety included frequency of AEs observed during vedolizumab induction, types of AEs observed, seriousness of the AEs, and causal relationship between vedolizumab treatment and the AEs. Serious AEs were defined as events causing death, events that required hospitalization or were life-threatening at onset, and events that could result in permanent or significant disability/dysfunction or congenital anomaly/birth defect. Adverse drug reactions (ADRs) were defined as AEs with plausible time relationship to vedolizumab intake or those for which a causal relationship to the drug was at least a reasonable possibility (i.e., the relationship could not be ruled out) as deemed by the physician. Worsening of UC, deemed by the physician as related to vedolizumab treatment, was considered an ADR.
Measures of effectiveness included the proportion of patients achieving therapeutic response during the induction phase, as defined by any therapeutic response assessed by the physicians, or improvement or remission of complete or partial Mayo score (Supplementary Material Table 1) [14, 15]. Complete Mayo score was calculated as the sum of all subscores (stool frequency, rectal bleeding, mucosal appearance at endoscopy, and physician rating of disease activity); and partial Mayo score was calculated as the sum of three subscores (stool frequency, rectal bleeding, and physician rating of disease activity). Remission of complete or partial Mayo score was defined as complete or partial Mayo score of 2 or less with no individual subscores being greater than 1. Improvement of complete or partial Mayo score was defined as decrease in complete Mayo score of at least 3 points and at least 30% from baseline or decrease in partial Mayo score of at least 2 points and at least 25% from baseline, with an accompanying decrease in rectal bleeding subscore of at least 1 point from baseline or an absolute rectal bleeding subscore of 1 or less. If at least one subscore was missing, the complete or partial Mayo score was treated as non-response and non-remission. Treatment responses were assessed in the total and stratified patient populations according to prior TNFα inhibitor treatments and/or baseline partial Mayo score (≥ 3, ≥ 4, or ≥ 5).
Quality of life was assessed via the Short Inflammatory Bowel Disease Questionnaire (SIBDQ), a 10-item questionnaire giving a total score of 10–70 points. Lower scores on the SIBDQ indicate more severe impairment in quality of life [16].
Sample Size
A sample size of 1000 was planned to achieve 95% or greater power in detecting at least one AE with a frequency of at least 0.3%. Of the 1000 patients, at least 300 TNFα inhibitor-naïve and 300 TNFα inhibitor-experienced patients were to be enrolled.
An interim analysis was performed when Mayo score data had been collected from at least 90 TNFα inhibitor-naïve and 90 TNFα inhibitor-experienced patients completing induction treatment with vedolizumab (i.e., received three doses or discontinued after one or two doses).
Statistical Analysis
All patients who received at least one dose of vedolizumab during the induction phase, who had no major protocol violations, and whose data in the case report form was fixed by the cutoff date (21 January 2021) were included in the safety analysis set. Of those included in the safety analysis set, patients who were evaluable for effectiveness were included in the effectiveness analysis set.
Descriptive analyses were performed for the entire patient cohort. In patients assessed for effectiveness, analyses were stratified according to prior TNFα inhibitor exposure and baseline partial Mayo score. Standard descriptive statistics were calculated for continuous variables: N, mean, standard deviation (SD), minimum, and maximum. Frequency tables with numbers and percentages were generated for categorical variables.
Results
Patients and Treatment
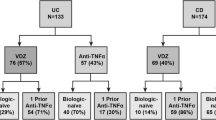
The cutoff date for this interim analysis was 21 January 2021, at which point 685 patients had been enrolled and data had been collected from 425 patients (Fig. 1). Of the 425 case report forms collected, data from 274 report forms were locked by the cutoff date. A total of 268 patients were eligible for assessment of safety. Of these, 10 patients were excluded because of inclusion criteria violation; thus, 258 patients were eligible for assessment of effectiveness (Fig. 1). AEs included in the safety analysis were those occurring during the induction phase of treatment. The median (range) number of patients enrolled by the same institution in each analysis set were as follows: effectiveness analysis set, 2 (1–31); and safety analysis set, 2 (1–32).
In the safety analysis set (n = 268), comprising patients enrolled from 72 institutions, mean (SD) patient age was 43.6 (17.6) years and 59.7% (160/268) of patients were male (Table 1). Disease severity was moderate in almost all (96.6%; 259/268) patients, and the majority (70.1%; 188/268) had extensive colitis. In the effectiveness analysis sets, 96.5% (249/258) of the patients had moderately active UC and 69.4% (179/258) of the patients had extensive colitis. The proportions of patients who had prior TNFα inhibitor exposure were 43.3% (116/268 patients) and 42.6% (110/258) in the safety analysis set and effectiveness analysis set.
Safety Outcomes
Eighteen ADR events were reported in 11/268 (4.10%) patients during the study period (Table 2). Dizziness, nausea, and arthralgia were each reported in 0.75% of patients (2/268). Herpes zoster oticus and worsening of UC were each reported in 0.37% of patients (1/268); these were considered to be serious ADRs. The outcomes of ADRs were “recovered/resolved” in 2.24% of patients (6/268), “recovering/resolving” in 1.12% of patients (3/268), and “not recovered/not resolved” in 0.75% of patients (2/268) at the interim cutoff date. The ADRs that were not recovered/not resolved were herpes zoster oticus and pruritus.
Effectiveness Outcomes
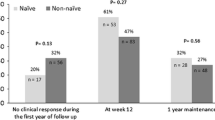
Therapeutic response was reported in 84.5% (218/258) of the overall patient population, with 85.8% (127/148) in TNFα inhibitor-naïve patients and 82.7% (91/110) in TNFα inhibitor-experienced patients during the induction phase (Table 3). Among the TNFα inhibitor-experienced patients who showed a therapeutic response, 83.1% (59/71) of patients used one kind of TNFα inhibitor and 82.1% (32/39) of patients used more than one kind of TNFα inhibitor (Table 3). Among the patients eligible for assessment of partial Mayo score after vedolizumab induction, the proportion with remission of partial Mayo score was 60.1% (137/228) and with improvement of partial Mayo score was 64% (146/228) (Table 3). On analysis by the institution with the largest number of eligible patients, the proportion of patients with remission or improvement of the partial Mayo score did not notably differ at 60% and 63.3%, respectively.
Mean (SD) partial Mayo score decreased from 5.0 (1.57) at baseline (n = 236) to 2.5 (2.16) after vedolizumab induction (n = 228), a mean change (n = 220) of − 2.5 (2.35). Changes in partial Mayo subscores are shown in Table 4. Mean (SD) stool frequency subscore decreased from 1.9 (1.01) at baseline (n = 236) to 1.1 (1.01) after vedolizumab induction (n = 228), a mean change (n = 220) of − 0.8 (1.17).
Among the patients with a partial Mayo score ≥ 4 at baseline (n = 190), mean (SD) partial Mayo score decreased from 5.6 (1.13) to 2.7 (2.22) after vedolizumab induction (n = 175), a mean change of − 3.0 (2.31). Partial Mayo score remission was achieved in 62.5% (60/96) of TNFα inhibitor-naïve patients and in 45.6% (36/79) of TNFα inhibitor-experienced patients. Partial Mayo score improvement was achieved in 77.1% (74/96) of TNFα inhibitor-naïve patients and in 69.6% (55/79) of TNFα inhibitor-experienced patients (Table 5). Of the TNFα inhibitor-experienced patients who achieved partial Mayo score remission, 40.4% (21/52) of patients used one kind of TNFα inhibitor and 55.6% (15/27) of patients used more than one kind of TNFα inhibitor. Of the TNFα inhibitor-experienced patients who achieved partial Mayo score improvement, 67.3% (35/52) of patients used one kind of TNFα inhibitor and 74.1% (20/27) of patients used more than one kind of TNFα inhibitor. Partial Mayo score remission and response rates were generally numerically higher in TNFα inhibitor-naïve patients, regardless of baseline patient characteristics. Similar results were observed when patients were analyzed according to a partial Mayo score ≥ 3 and ≥ 5 at baseline (data not shown).
Quality of Life
Patient quality of life was improved after vedolizumab induction, as demonstrated by an increase in mean (± SD) SIBDQ score from 44.2 (11.89) at baseline (n = 223) to 53.3 (11.05) after vedolizumab induction (n = 210), a mean change (n = 204) of 8.9 (12.53).
Discussion
This interim analysis of an ongoing surveillance study evaluated the safety and effectiveness of vedolizumab during the induction phase in patients with moderate-to-severe UC with and without prior TNFα inhibitor treatment.
In the safety analysis set, the incidence of ADRs during vedolizumab induction was 4.10% (11/268 patients). Although direct comparison is difficult because of differences in patient demographics and observation period, this rate was lower than that seen in the induction phase of a Japanese clinical trial of vedolizumab (10.4%; 17/164 patients) [8]. In this study, AEs reported in at least two patients were dizziness, nausea, and arthralgia, all occurring at a rate of 0.75% (2/268 patients). These AEs have been previously reported in clinical trials of vedolizumab [7, 8]. The incidence of serious adverse events in this study was 0.75% (2/268 patients), consisting of herpes zoster oticus and UC in one patient each.
In the effectiveness analysis set, the therapeutic response rate after vedolizumab induction was over 80%, with partial Mayo score remission and improvement being over 60% each. High rates of partial Mayo score remission and partial Mayo score improvement were achieved in both TNFα inhibitor-naïve and TNFα inhibitor-experienced patients; however, rates were generally numerically higher in TNFα inhibitor-naïve patients.
The robust therapeutic response, partial Mayo score remission, and improvement in both TNFα inhibitor-naïve and TNFα-experienced patients after vedolizumab induction were in line with the results of previously published studies. A post hoc analysis of GEMINI 1 [10], the pivotal clinical trial of vedolizumab in patients with UC, demonstrated significantly higher clinical response rates after vedolizumab induction at week 6 in both TNFα inhibitor-naïve (53.1%) and TNFα-experienced patients (39.0%) as compared with placebo in TNFα inhibitor-naïve (26.3%) and TNFα-experienced patients (20.6%). In a Korean real-world study of patients with UC whose disease had to failed to respond to TNFα inhibitor therapy, the week 6 clinical response rate was 51.1% in GEMINI 1–matched subjects [12]. A phase 3 clinical trial of vedolizumab in Japanese patients also showed a significantly higher clinical response rate at week 10 in TNFα inhibitor-naïve patients (53.2%) in comparison with placebo controls (36.6%). However, that trial did not find a significant difference in clinical response between vedolizumab and placebo in TNFα inhibitor-experienced patients (27.1% vs 29.3%); this may have been due to the high placebo response rate noted in this trial [8]. In the current study, partial Mayo score remission and improvement rates were high in comparison with the clinical response rates reported in the previous studies. This is likely because a different definition of clinical response was used in the previous studies (defined as a reduction in the complete Mayo score of at least 3 points and a decrease of at least 30% from the baseline score, with a decrease of at least 1 point on the rectal bleeding subscale or an absolute rectal bleeding score of 0 or 1). In contrast the present study defined therapeutic responses based on complete or partial Mayo scores, the latter of which does not incorporate endoscopic findings. This difference along with others such as baseline disease severity (the majority of patients assessed had UC of moderate severity) may have affected the results of this study.
Patient quality of life was improved after vedolizumab induction, as assessed by the SIBDQ scale, consistent with previous studies reporting improved health-related quality of life or fatigue [17, 18].
There are several limitations to this study. As an interim analysis, inclusion was based on order of data submission rather than order of patient enrollment. Given that complicated data take longer to submit, there is potential for inclusion of patients to be biased toward those with no or less severe AEs. The study only included patients from pre-specified institutions, rather than all patients treated with vedolizumab in Japan, which limits generalizability of the data. By their nature, post-marketing surveillance studies do not include a control group. The interim analysis only included data from vedolizumab induction, and the observation period was short. Only six patients were eligible for complete Mayo score assessment, owing to a lack of endoscopy data; thus, therapeutic response and partial Mayo score were used for the primary effectiveness analysis in the present study. Additionally, as the randomization could not be performed between subgroups, the difference in responses between subgroups could not be differentiated because of the biases of other background confounding factors. Moreover, the sample size was not enough to adjust the confounders and there may be unmeasured confounding factors. Finally, no objective biomarkers were used in the assessment of vedolizumab effectiveness. The protocol of this study specified the measurement of biomarkers (e.g., C-reactive protein and calprotectin); however, data collection was incomplete in daily clinical practice as a result of the limitations of the post-marketing study.
To our knowledge, this is the largest study conducted to date of vedolizumab use in Asian patients with UC in routine clinical practice. The final analysis of this study will present long-term safety and effectiveness data (after 54 weeks of treatment) for vedolizumab, including stratification of data according to prior TNFα inhibitor exposure.
Conclusion
We confirmed the safety of vedolizumab in the induction phase of this post-marketing study of patients with moderate-to-severe active UC in Japan. Our safety findings are consistent with those of published clinical trials [7, 8], and no new safety signals were detected. In addition, effectiveness of vedolizumab was observed in patients with moderate-to-severe active UC, regardless of prior TNFα inhibitor exposure, although the results were more favorable in TNF inhibitor-naïve patients when using the partial Mayo score assessment in a subpopulation with higher baseline disease activity (partial Mayo score of ≥ 4).
References
Ungaro R, Mehandru S, Allen PB, Peyrin-Biroulet L, Colombel JF. Ulcerative colitis. Lancet. 2017;389(10080):1756–70.
Rubin DT, Ananthakrishnan AN, Siegel CA, Sauer BG, Long MD. ACG clinical guideline: ulcerative colitis in adults. Am J Gastroenterol. 2019;114(3):384–413.
Kobayashi T, Siegmund B, Le Berre C, et al. Ulcerative colitis. Nat Rev Dis Primers. 2020;6(1):74.
Nakase H, Uchino M, Shinzaki S, et al. Evidence-based clinical practice guidelines for inflammatory bowel disease 2020. J Gastroenterol. 2021;56(6):489–526.
Wyant T, Fedyk E, Abhyankar B. An overview of the mechanism of action of the monoclonal antibody vedolizumab. J Crohns Colitis. 2016;10(12):1437–44.
Lamb CA, O’Byrne S, Keir ME, Butcher EC. Gut-selective integrin-targeted therapies for inflammatory bowel disease. J Crohns Colitis. 2018;12(suppl_2):S653–68.
Feagan BG, Rutgeerts P, Sands BE, et al. Vedolizumab as induction and maintenance therapy for ulcerative colitis. N Engl J Med. 2013;369(8):699–710.
Motoya S, Watanabe K, Ogata H, et al. Vedolizumab in Japanese patients with ulcerative colitis: a phase 3, randomized, double-blind, placebo-controlled study. PLoS ONE. 2019;14(2): e0212989.
Sands BE, Peyrin-Biroulet L, Loftus EV Jr, et al. Vedolizumab versus adalimumab for moderate-to-severe ulcerative colitis. N Engl J Med. 2019;381(13):1215–26.
Feagan BG, Rubin DT, Danese S, et al. Efficacy of vedolizumab induction and maintenance therapy in patients with ulcerative colitis, regardless of prior exposure to tumor necrosis factor antagonists. Clin Gastroenterol Hepatol. 2017;15(2):229-39 e5.
Cohen RD, Bhayat F, Blake A, Travis S. The safety profile of vedolizumab in ulcerative colitis and Crohn’s disease: 4 years of global post-marketing data. J Crohns Colitis. 2020;14(2):192–204.
Ye BD, Cheon JH, Song KH, et al. The real-world outcomes of vedolizumab in patients with ulcerative colitis in Korea: a multicenter retrospective study. Therap Adv Gastroenterol. 2021;14:17562848211024768.
Evidence-based Clinical Practice Guidelines for Inflammatory Bowel Disease (IBD) 2020. (2nd Edition). The Japan Society of Gastroenterology 2020. https://www.jsge.or.jp/guideline/guideline/pdf/ibd2020_.pdf. Accessed Nov 2020.
Lewis JD, Chuai S, Nessel L, et al. Use of the noninvasive components of the Mayo score to assess clinical response in ulcerative colitis. Inflamm Bowel Dis. 2008;14(12):1660–6.
Loftus EV Jr, Colombel JF, Feagan BG, et al. Long-term efficacy of vedolizumab for ulcerative colitis. J Crohns Colitis. 2017;11(4):400–11.
Jowett SL, Seal CJ, Barton JR, Welfare MR. The short inflammatory bowel disease questionnaire is reliable and responsive to clinically important change in ulcerative colitis. Am J Gastroenterol. 2001;96(10):2921–8.
Feagan BG, Patel H, Colombel JF, et al. Effects of vedolizumab on health-related quality of life in patients with ulcerative colitis: results from the randomised GEMINI 1 trial. Aliment Pharmacol Ther. 2017;45(2):264–75.
Borren NZ, Tan W, Colizzo FP, et al. Longitudinal trajectory of fatigue with initiation of biologic therapy in inflammatory bowel diseases: a prospective cohort study. J Crohns Colitis. 2020;14(3):309–15.
Acknowledgements
The authors thank the patients involved in this study.
Funding
The study was funded by Takeda Pharmaceutical Company Ltd. The publication fee was also funded by Takeda Pharmaceutical Company Ltd.
Medical Writing and/or Editorial Assistance
The authors thank the Japanese Society for Inflammatory Bowel Disease for their valuable advice on this study. The authors thank Hitomi Ooe of Biometrics, PRA Health Sciences K.K. for her help with analysis of the data. Medical writing support was provided by Ngaire White and Fumiko Shimizu on behalf of MIMS Co., Ltd., sponsored by Takeda Pharmaceutical Company Limited, in compliance with Good Publication Practice 3 ethical guidelines (Battisti et al. Ann Intern Med. 2015; 163: 461–4).
Author Contributions
Katsuyoshi Matsuoka, Tadakazu Hisamatsu, Yohei Mikami, Takayuki Yamamoto, Satoshi Motoya, Shinichiro Shinzaki, Ryuichi Iwakiri, Kenkichi Sugiura, Mika Kajita, and Jovelle L. Fernandez were involved in conceptualization and designing of the study. Kenkichi Sugiura and Kunihiko Nishimura analyzed the data and interpreted the data together with Katsuyoshi Matsuoka, Tadakazu Hisamatsu, Yohei Mikami, Takayuki Yamamoto, Satoshi Motoya, Shinichiro Shinzaki, Kenkichi Sugiura, and Mika Kajita. Katsuyoshi Matsuoka, Tadakazu Hisamatsu, Yohei Mikami, Takayuki Yamamoto, Satoshi Motoya, Shinichiro Shinzaki, Kunihiko Nishimura, Mika Kajita, and Jovelle L. Fernandez were involved in writing original draft, and all authors critically reviewed the subsequent drafts and approved the final draft of the manuscript.
Disclosures
Katsuyoshi Matsuoka reports grants from AbbVie G.K., Takeda Pharmaceutical Co. Ltd., EA Pharma Co. Ltd., Mochida Pharmaceutical Co., Ltd., Janssen Pharmaceutical K.K., Pfizer Japan Inc., KYORIN Pharmaceutical Co., Ltd., ZERIA Pharmaceutical Co., Ltd., Kissei Pharmaceutical Co., Ltd., Nippon Kayaku Co., Ltd., and JIMRO Co., Ltd., consulting fees from EA Pharma Co. Ltd., and honoraria from Takeda Pharmaceutical Co. Ltd., Mitsubishi Tanabe Pharma Corporation, Janssen Pharmaceutical K.K., AbbVie G.K., EA Pharma Co. Ltd., Mochida Pharmaceutical Co., Ltd., KYORIN Pharmaceutical Co., Ltd., ZERIA Pharmaceutical Co., Ltd., Kissei Pharmaceutical Co., Ltd., Nippon Kayaku Co., Ltd., JIMRO Co., Ltd., and Pfizer Japan Inc. Tadakazu Hisamatsu reports research grants from EA Pharma Co. Ltd., AbbVie G.K., Pfizer Japan Inc., Mitsubishi Tanabe Pharma Corporation, KYORIN Pharmaceutical Co., Ltd., JIMRO Co., Ltd., Mochida Pharmaceutical Co., Ltd., Daiichi Sankyo Co., Ltd., Takeda Pharmaceutical Co. Ltd., ZERIA Pharmaceutical Co., Ltd., and Nippon Kayaku Co., Ltd., consulting fees from EA Pharma Co. Ltd., AbbVie G.K., Pfizer Japan Inc., Mitsubishi Tanabe Pharma Corporation, Takeda Pharmaceutical Co. Ltd., Nichi-Iko Pharmaceutical Co., Ltd., Gilead Sciences K.K., Eli Lilly Japan K.K., and Janssen Pharmaceutical K.K., and honoraria from EA Pharma Co. Ltd., AbbVie G.K., Pfizer Japan Inc., Mitsubishi Tanabe Pharma Corporation, KYORIN Pharmaceutical Co., Ltd., JIMRO Co., Ltd., Mochida Pharmaceutical Co., Ltd., Daiichi Sankyo Co., Ltd., Takeda Pharmaceutical Co. Ltd., ZERIA Pharmaceutical Co., Ltd., Nippon Kayaku Co., Ltd., and Janssen Pharmaceutical K.K. Satoshi Motoya reports honoraria from Takeda Pharmaceutical Co. Ltd., Janssen Pharmaceutical K.K., AbbVie G.K., and Mitsubishi Tanabe Pharma Corporation. Shinichiro Shinzaki reports honoraria from Takeda Pharmaceutical Co. Ltd. and participation in an advisory board of Takeda Pharmaceutical Co. Ltd. Ryuichi Iwakiri, Kenkichi Sugiura, and Mika Kajita are employees of Takeda Pharmaceutical Co. Ltd., Kunihiko Nishimura and Jovelle L. Fernandez were employees of Takeda Pharmaceutical Company Limited at the time of this study. Jovelle L. Fernandez reports ownership of stock of GlaxoSmithKline PLC and Takeda Pharmaceutical Co. Ltd. Yohei Mikami and Takayuki Yamamoto report no conflict of interests related to this manuscript.
Compliance with Ethics Guidelines
This study was conducted in accordance with the Japanese guidelines for Good Post-Marketing Study Practice. In accordance with the Japanese regulations for post-marketing surveillance, it was not necessary to obtain institutional review board/ethics committee approval or written informed patient consent. Prior to commencement, the study was registered with the Japan Pharmaceutical Information Center – Clinical Trials Information (JapicCTI-194603), and the National Institutes of Health Clinical Trial Registration System – ClinicalTrials.gov (NCT03824561), both of which have publicly accessible websites.
Data Availability
The data sets, including the redacted study protocol, redacted statistical analysis plan, and individual participants data supporting the results of the completed study, will be made available after the publication of the final study results, within 3 months from initial request, to researchers who provide a methodologically sound proposal. The data will be provided after its de-identification, in compliance with applicable privacy laws, data protection, and requirements for consent and anonymization.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Matsuoka, K., Hisamatsu, T., Mikami, Y. et al. Safety and Effectiveness of Vedolizumab in Patients with Moderate-to-Severe Ulcerative Colitis: An Interim Analysis of a Japanese Post-Marketing Surveillance Study. Adv Ther 40, 2902–2914 (2023). https://doi.org/10.1007/s12325-023-02500-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-023-02500-6