Abstract
Irritable bowel syndrome with diarrhea (IBS-D) is a chronic disorder of gut–brain interaction, characterized by recurrent abdominal pain in association with more frequent, loose stools. The pathophysiology of irritable bowel syndrome (IBS) includes disordered gut motility, alterations in gut microbiota, neural-hormonal system abnormalities, immune reactivity, and visceral hypersensitivity. Timely diagnosis of IBS-D can be achieved easily using clinical criteria. Formal IBS diagnosis is important for optimizing treatment and patient outcomes and facilitating patient access to appropriate educational resources. Yet, given the symptom overlap with other gastrointestinal conditions, diagnosis of IBS-D often is perceived to be challenging. Treatment of IBS includes both nonpharmacologic and pharmacologic options. Rifaximin, alosetron, and eluxadoline are effective treatments indicated for IBS-D, but have limited availability internationally. Dietary approaches may also be indicated for certain patients with IBS-D. Psychological interventions may be effective in treating abdominal pain alone and global symptoms in IBS. We describe use of these diverse therapies and provide an overview to facilitate the primary care provider’s approach to distinguishing IBS-D from other conditions with symptom overlap.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Irritable bowel syndrome (IBS) is a commonly encountered disorder of gut–brain interactions characterized by recurrent abdominal pain and altered defecation |
Symptoms of IBS with diarrhea (IBS-D) overlap with other conditions frequently encountered by primary care providers |
Diagnosis of IBS-D relies primarily on symptom-based criteria, with the addition of minimal fecal and serologic testing to increase confidence in diagnosis |
IBS-D management strategies involve nonpharmacologic and pharmacologic therapies |
Introduction
Gastrointestinal (GI) symptoms have been associated with approximately 40.7 million US ambulatory visits (2014), with abdominal pain (21.8 million) and diarrhea (3.4 million) the symptoms most commonly reported [1]. Total expenses associated with abdominal pain were $10.2 billion in 2015, driven primarily by inpatient hospitalizations (77.9%) and diagnostic testing [1]. According to Rome IV diagnostic criteria, irritable bowel syndrome (IBS) is characterized by recurrent abdominal pain and changes in stool form and/or frequency [2, 3]. It is classified further by bowel habits (based on Rome IV criteria): IBS with constipation (IBS-C; 28.5%), with diarrhea (IBS-D; 35.0%), or with mixed bowel habits (IBS-M; 31.0%) [2]. The US prevalence of IBS has been estimated to range from 4.8% to 5.3%, versus 0.7% for celiac disease and 0.5% for inflammatory bowel disease (IBD) [4,5,6,7]. Optimal diagnostic and therapeutic strategies for IBS management consider the predominant symptoms (i.e., pain, discomfort, bloating) and the predominant bowel habit (i.e., diarrhea, constipation, or mixed) [8]. Accordingly, approaches for each IBS subtype may vary considerably. This review focuses on diagnosis and treatment of patients with diarrhea-predominant IBS, with an emphasis on US gastroenterology guidelines. However, when appropriate, attempts were made to highlight contrasting recommendations for European society guidelines. This review is based on previously conducted studies and does not contain any new data from human or animal studies conducted by any of the authors.
Pathophysiology
IBS-D is a chronic disorder of gut–brain interaction (previously regarded as functional bowel disorders) for which a distinct isolated structural pathology is not identified [3]. It is a heterogeneous condition with a multifactorial, evolving pathophysiology that includes alterations in visceral sensitivity, gut microbial changes, increased intestinal epithelial permeability, disrupted motility, and immune and neural-hormonal system involvement [3, 9,10,11,12,13,14,15]. GI-related infections can predispose to development of postinfectious IBS [16], a distinct condition in which IBS diagnostic criteria are met. Postinfectious IBS occurs after resolution of a GI-related infection (e.g., Campylobacter jejuni, Salmonella) without a prior history of IBS symptoms [8, 17,18,19].
Clinical pearl: IBS-D is a heterogenous condition with multifactorial etiologies.
Diagnosis of IBS
The evaluation of a patient with suspected IBS includes a detailed medical history and physical examination [2]. Rome IV criteria facilitate a confident IBS diagnosis based on the presence and/or history of abdominal symptoms (i.e., pain, discomfort, bloating), commonly occurring in the lower abdomen, and altered bowel habits in the absence of alarm symptoms [2]. The American College of Gastroenterology (ACG) guideline for IBS management strongly recommends a positive IBS diagnostic strategy, rather than a diagnosis of exclusion, to improve patient care and decrease health care costs [20]. The Bristol Stool Scale helps identify the most frequent stool consistency experienced by patients and aids in choosing subsequent treatment for the predominant bowel pattern [20]. Limited laboratory testing, such as measurement of C-reactive protein (CRP) and fecal calprotectin or fecal lactoferrin levels, is recommended to exclude IBD [20]. The rapidly obtained CRP may be more useful than fecal analyses, which are more challenging to collect. Finally, psychological markers (e.g., patient health questionnaire-15 score, anxiety and depression components of the Hospital Anxiety and Depression Scale) may have some utility for diagnosing IBS [21].
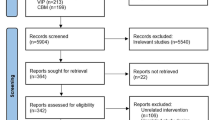
A prospective trial of patients with symptoms suggestive of IBS found that GI referral for colonoscopy is only warranted for patients with alarm symptoms and, as appropriate, for colon cancer screening (age 45 years or more to 75 years; Fig. 1) [8, 20, 22]. The diagnostic yield of colonoscopy for organic disease (i.e., colon cancer, IBD, microscopic colitis) was greater in patients with IBS-D than in patients with IBS-C and IBS-M [23]. In all cases, the pathologic findings were associated with red flag features, including unintended weight loss, recent antibiotic use, and hematochezia (Fig. 1) [8, 20, 22]. Referral to a gastroenterologist may occur at the patient’s request, usually when the patient fails treatment, when symptoms are severe, or when a diagnosis cannot easily be established [24].
Comorbid Disorders: Testing to Exclude IBS
Comorbid conditions are common in patients with IBS and can include anxiety and depression, chronic fatigue, fibromyalgia, and sleep disorders [25, 26]. Awareness of comorbidities may help guide management decisions and may lead to a multidisciplinary approach to best address all physical and psychological comorbidities [26]. Establishing a diagnosis of IBS-D is important for patient reassurance and to minimize undue cost to the patient or health care system [26]. Given the symptom overlap between IBS-D and other disorders often encountered in primary care practices, consideration of other conditions can guide clinicians (Table 1) [20, 27,28,29,30,31,32,33,34,35,36,37,38,39].
Other Diagnoses That May Mimic IBS-D
Celiac Disease
Celiac disease presents with diarrhea, abdominal pain, and bloating [20, 30]. Celiac disease is found in 1.1% of patients with IBS in the US [40]. Serologic testing for celiac disease with both serum IgA and tissue transglutaminase (TTG) should be conducted in patients with IBS-D symptoms, as a small percentage of patients with celiac disease are IgA deficient and could have a false negative TTG test result [31]. If IgA deficiency is found, follow-up testing should be performed with deaminated gliadin IgG antibodies; in some cases, an upper endoscopy and duodenal biopsies may be warranted [31] (Table 1).
IBD
Symptoms of IBS-D and IBD overlap, making it difficult to distinguish between the two conditions [41]. Blood CRP levels and fecal testing (i.e., calprotectin, lactoferrin) can be considered to exclude an IBD diagnosis (Table 1) [20, 35, 36].
Clinical pearl: Celiac disease and IBD should be considered in the differential diagnosis for IBS-D, and celiac antibody testing and inflammatory marker testing (CRP, fecal calprotectin/lactoferrin) are recommended to rule out the former.
Food Allergy Should Not Be Considered in IBS-D
Food contents can lead to GI symptoms (e.g., abdominal pain, bloating), which may, in part, be related to a local immune response to food antigens (i.e., gluten, milk, soy, wheat) [34]. Food allergies are estimated to affect 2.5% of the US population [42] and are a rapid (i.e., within several minutes), systemic, immune-mediated reaction to food (Table 1) [32,33,34]. Referral to a board-certified allergist is recommended for patients with obvious allergic reactions (i.e., angioedema, rash) [32]. The ACG guideline for IBS management does not recommend testing for food allergies in patients with IBS unless there is reproducible symptomatology suggesting a possible food allergy, given that current tests for food allergies have not been validated or standardized [20].
Carbohydrate Intolerances
Intolerances to carbohydrates, such as lactose and sucrose, can cause diarrhea [28, 29] and can be ruled out by food elimination trials or, if not confirmatory, by breath testing. Lactose intolerance is a common condition that may be misdiagnosed as IBS, given the similarity in symptoms (e.g., diarrhea, flatulence; Table 1) [28]. After consuming a lactose-free diet for 1 month, patients with IBS and lactose intolerance experienced a decrease from baseline in both IBS and lactose malabsorption symptom severity scale scores [28]. Sucrase-isomaltase (SI) deficiency also can cause symptoms of abdominal pain, bloating, and diarrhea [29], and SI gene variants have been associated with IBS in some patients [43, 44]. However, the prevalence of SI deficiency in IBS has not been determined [29].
Pelvic Floor Disorders
Dyssynergia is a defecatory disorder characterized by increased anal sphincter pressure (i.e., anal contraction; Table 1) for which biofeedback—using visual or auditory cues to improve muscle control—is efficacious [38, 45]. It is important to ascertain whether the patient has intermittent constipation or solid stools, in which case, diarrhea may reflect an “overflow” phenomenon. Diarrheal symptoms also may overlap with weak sphincter tone and fecal incontinence, as well as a structural abnormality (e.g., rectocele) [46]. The ACG guideline for IBS management suggests that anorectal physiology testing be performed in patients with IBS and symptoms of pelvic floor disorder, despite limited data supporting this testing [20].
Bile-Acid Malabsorption
Diarrhea is the primary symptom of bile-acid malabsorption [47], occurring when bile acids are not reabsorbed in the small intestine, such as with conditions causing bile-acid malabsorption (e.g., cholecystectomy, terminal ileal resection, radiation) or primary bile-acid diarrhea [27]. Bile-acid testing (i.e., fasting serum C4, fasting serum FGF19) is limited in the USA [20]; empiric treatment with bile-acid sequestrants can provide diagnostic insight but is not currently recommended by the ACG given the relative paucity of data currently supporting this approach (Table 1). However, in contrast, British Society of Gastroenterology (BSG) guidelines recommend that patients with symptoms of IBS-D with atypical features (e.g., prior cholecystectomy) undergo bile-acid testing to exclude bile-acid diarrhea [24].
Small Intestinal Bacterial Overgrowth
Prevalence of small intestinal bacterial overgrowth (SIBO) has been estimated at 38% in patients with IBS [48]. SIBO has several symptoms that overlap with IBS-D and the other IBS subtypes. In patients suspected to have SIBO (e.g., with prior abdominal surgery or systemic illnesses predisposed to development of SIBO), SIBO may be diagnosed via breath testing utilizing carbohydrate substrates (e.g., glucose, lactulose) [49]. Breath samples are collected from patients following an overnight fast and ingestion of a carbohydrate substrate to detect hydrogen and methane levels over a specific time period [49]. However, given the lack of standardization across breath tests (e.g., substrate dosing, test duration) and high false-positive rates, interpretation of findings is not straightforward and breath testing is not recommended for IBS-D [49].
Patient–Provider Relationship
Both the BSG and ACG guidelines emphasize the important role of a strong provider–patient relationship in effective management of IBS, highlighting its positive effects on patient treatment adherence, quality of life, and symptoms [20, 24]. Foundational elements of this relationship include clear communication, practical support, and compassion [24].
Dietary Interventions
Best practice guidance from the American Gastroenterological Association (AGA) is to give dietary advice to patients with IBS who have reported onset or worsening of GI symptoms (e.g., abdominal pain, altered bowel habits, bloating) after a meal [50]. The BSG recommends that providers offer dietary advice to all patients with IBS [24]. Further, survey data from patients with IBS in the Netherlands have indicated a preference for dietary interventions as first-line therapy compared with pharmacologic treatments [51].
Elimination Diets
Up to two-thirds of patients believe that diet plays a role in their IBS symptoms [52], and approximately one-third to two-thirds of patients have reported managing IBS symptoms with dietary modification [53]. Fermentable oligo-, di-, and monosaccharides and polyols (FODMAPs) were significantly associated with bloating in patients with IBS-D [54], and elimination of FODMAPs has led to improvement in global IBS symptoms [55]. Elimination diets involve withholding various foods for a short amount of time (i.e., days to weeks), rather than permanently. The ACG guideline for IBS management recommends a limited trial of a low FODMAP diet to evaluate improvement in global IBS symptoms, and this is the only diet endorsed by the ACG guideline committee (Table 2) [20, 24, 56]. The BSG recommends the low FODMAP diet as second-line therapy, with supervision from a trained dietician [24].
Although gluten-containing foods have been associated with diarrhea, abdominal cramping, and bloating, a gluten-free diet is not routinely recommended in the absence of celiac disease, and food containing glutens (e.g., wheat-based foodstuffs) often contain fructans, a FODMAP constituent [24, 57].
High Fiber Therapy in IBS
Survey data have indicated that 69.6% of primary care providers and gastroenterologists (n = 302) have recommended fiber supplementation to patients with IBS-D, although only 41.3% of patients reported being somewhat or very satisfied with this treatment [58]. The ACG guideline for IBS management strongly recommends soluble (e.g., barley, beans, oat bran, psyllium) rather than insoluble (e.g., wheat bran, whole grains, some vegetables) fiber for the treatment of global IBS symptoms, though the former class of agents may increase the incidence of bloating (Table 2) [20].
Probiotics, Prebiotics, and Synbiotics
A meta-analysis of 21 randomized, controlled studies of IBS (n = 1931 patients) has reported that combination probiotics significantly reduced IBS symptoms versus placebo (RR 0.8; 95% CI 0.7–0.9) [59]. The 2021 BSG guidelines recommend a trial of probiotics for up to 12 weeks, with discontinuation if no symptom improvement is observed [24]. Data for prebiotics (substrates selectively used by microorganisms [e.g., oligosaccharides] [60]) and synbiotics (combination of prebiotics and probiotics [61]) in IBS are limited, with a meta-analysis of prebiotics (n = 3 studies) and synbiotics (n = 2 studies) finding no benefit of either for reducing IBS symptoms [59]. Whether more-targeted probiotic therapy will be beneficial in treating all IBS subtypes remains to be seen. The 2021 ACG guideline for IBS management recommends against the use of probiotics for global IBS symptoms (Table 2) on the basis of inconsistencies in the types and strains of probiotics evaluated, heterogeneity among studies, and lack of studies examining US Food and Drug Administration (FDA) efficacy outcomes for IBS [20, 24].
Herbal/Supplement Therapies
Peppermint oil is an over-the-counter herbal therapy that has proven antispasmodic properties [62, 63]. A 2019 meta-analysis reported that enteric-coated peppermint oil improved global IBS symptoms (n = 7 studies; RR 2.4; 95% CI 1.9–3.0) and abdominal pain as compared with placebo (n = 6 studies; RR 1.8; 95% CI 1.4–2.2) [63]. The ACG guideline for IBS management suggests the use of peppermint oil for relief of global IBS symptoms on the basis of a low quality of evidence [20]. A randomized, double-blind, placebo-controlled trial of patients with postinfectious IBS-D with increased GI permeability showed that orally administered glutamine powder 5 g three times daily (n = 54) had 14-fold greater efficacy for improving the Irritable Bowel Syndrome Symptom Severity Scale scores from baseline versus placebo (n = 52) after 8 weeks of treatment (79.6% vs 5.8%, respectively; P < 0.0001) [64]. Further, patients receiving glutamine experienced significant improvements in daily bowel movement frequency and stool form and normalization of intestinal permeability versus placebo (P < 0.0001 for all comparisons) [64].
Antidiarrheal Agents
Over-the-counter loperamide is not recommended as first-line treatment for patients with IBS-D, as it is ineffective for improving global IBS symptoms and abdominal pain [20, 65], but it can be considered for intermittent use to control diarrheal symptoms as needed. Diphenoxylate/atropine, a prescription antidiarrheal agent, has been shown to significantly decrease stool frequency and weight in patients with chronic diarrhea and fecal incontinence versus placebo after 3 days (P < 0.02 and P < 0.001, respectively) [66, 67].
FDA-Approved Therapies for IBS-D
Rifaximin
Rifaximin is a nonsystemic antibiotic indicated for the treatment of adults with IBS-D and is administered as short-course therapy (one 550-mg tablet three times daily for 2 weeks) [68]. Patients may receive up to two additional rifaximin courses for symptom recurrence [68]. In two randomized, double-blind, clinical studies of patients with nonconstipation IBS (n = 1260), a significantly larger percentage of patients treated with rifaximin 550 mg three times daily for 2 weeks had adequate relief of global IBS symptoms versus placebo for at least two of the first 4 weeks post-treatment (40.7% vs 31.7%, respectively [pooled]; P < 0.001) [69].
In a repeat treatment trial, 44.1% of 2579 patients were open-label responders to rifaximin (patients with at least a 30% decrease from baseline in abdominal pain, plus at least a 50% reduction in frequency of loose stools for at least two of the first 4 weeks post-treatment) [70]. Initial responders with symptom recurrence entered a randomized, double-blind, placebo-controlled repeat treatment phase, wherein a significantly higher percentage of responders were observed with rifaximin (n = 328) versus placebo (n = 308) for 2 weeks (38.1% vs 31.5%, respectively; P = 0.03) [70]. Across all studies, rifaximin exhibited a favorable safety profile, with adverse events (AEs) comparable to those reported with placebo, including incidence of C. Clostridioides difficile colitis [69, 70]. The ACG guideline for IBS management recommends rifaximin for the treatment of global IBS-D symptoms [20]; however, rifaximin is not a guideline recommendation for treatment of IBS-D in some countries [24].
Alosetron
The selective serotonin (5-HT3) receptor antagonist alosetron is approved at a dose of 0.5 to 1.0 mg twice daily for the treatment of women with severe IBS-D with chronic (at least 6 months) IBS symptoms and a lack of adequate response to conventional therapy, under a modified risk evaluation and mitigation strategy program [71,72,73]. A systematic review reported that alosetron improved global IBS symptoms versus control treatment (three studies; RR 1.6; 95% CI 1.4–1.8), including improved abdominal pain/discomfort (eight studies; RR 1.24; 95% CI 1.2–1.3) [74]. However, AEs of ischemic colitis and complications of constipation, though rare, have occurred with alosetron [75]. Alosetron is an effective treatment for the relief of global IBS-D symptoms in women with moderate to severe IBS-D symptoms for whom conventional treatment has failed; however, access to this medication may be limited in the USA and other countries, related to the indication and risk evaluation and mitigation strategy program [71,72,73].
Eluxadoline
Eluxadoline is a peripherally acting mixed mu- and kappa-opioid receptor agonist/delta-opioid receptor antagonist indicated for the treatment of adults with IBS-D [76, 77]. Recommended eluxadoline dosing is 75–100 mg bid, taken with food [76]. In two randomized, double-blind, placebo-controlled trials of patients with IBS-D, eluxadoline 100 mg bid (n = 809) for up to 6 months resulted in a significantly greater percentage of patients achieving a decrease from baseline of at least 30% in the daily average worst abdominal pain for at least 50% of days and, on the same days, a stool consistency score less than 5 (score range, 1 [hard stool] to 7 [watery diarrhea]) versus placebo (n = 808; 31.0% vs 19.5%, respectively [pooled]; P < 0.001) [77]. The most common AEs in two clinical trials of eluxadoline 100 mg versus placebo were constipation (8.6% vs 2.5%, respectively), nausea (7.5% vs 5.1%), and abdominal pain (7.2% vs 4.1%) [77]. Eluxadoline is contraindicated in patients with IBS-D with prior sphincter of Oddi dysfunction or cholecystectomy, alcohol dependence, pancreatitis, or severe hepatic impairment [24, 76]. Use of eluxadoline is limited because of its lack of availability and approval in many countries [24]. The ACG guideline for IBS management and BSG guidelines both recommend mixed opioid agonists/antagonists for treatment of global IBS-D symptoms [20, 24].
While the therapies currently approved by the FDA for treatment of patients with IBS-D have comparable number needed to treat values (Table 3) [20, 59, 78,79,80], rifaximin has been shown to have the highest (superior) number needed to harm value (8971; i.e., 8971 patients need to be treated to observe one adverse event) [20, 78]. Though these medications differ by intended patient population, mechanism of action, and duration of treatment (short-term vs continuous) [68, 71, 76, 77], they play an important role in overall management of IBS-D for providers with access to these therapies.
Non-FDA-Approved Therapies for IBS-D
Neuromodulators
Levels of depression have been shown to be significantly greater in patients with IBS compared with healthy individuals [81,82,83]. Neuromodulators, including the more commonly termed antidepressants, may reduce symptoms of IBS, as indicated by a meta-analysis (n = 12 studies) reporting that 42.7% of 436 patients with IBS experienced no improvement in IBS symptoms with tricyclic antidepressants (TCAs) versus 63.8% of 351 patients receiving placebo [84]. Of note, the anticholinergic side effects of TCAs may be beneficial for some patients with IBS-D, as GI transit is slowed [85]. The Rome Foundation Working Group recommended use of peripherally acting agents (e.g., gabapentin) when pain is mild to moderate and intermittent in nature but recommended adding or substituting centrally acting agents (e.g., tricyclic antidepressants) when pain is severe or persistent [85]. Starting doses of TCAs typically range from 10 to 25 mg. TCAs should be titrated slowly over several weeks, and it may take several months to achieve maximal effects on IBS-D symptoms. The ACG guideline for IBS management strongly recommends TCAs for treatment of global IBS symptoms [20].
Antispasmodics
Antispasmodics are a broad therapeutic class of agents with multiple mechanisms of action, including smooth-muscle relaxants, calcium antagonists, and combination therapies [20]. Dicyclomine, hyoscine, and hyoscyamine are the three antispasmodics currently available in the USA [20]. Clinical trials of these agents are of low quality, dated, and limited by the small size of the patient populations; further, studies differed in design, inclusion criteria, and outcomes [20]. While the ACG guideline for IBS management recommends against the use of antispasmodics for treating global IBS symptoms in any IBS subtype, including IBS-D [20], the BSG guidelines, in contrast, suggest that some antispasmodics may be beneficial [24]. These conflicting recommendations, in part, reflect differences in availability of specific antispasmodic agents in international markets [20, 24].
Bile-Acid Sequestrants
Bile-acid sequestrants may have efficacy in patients with IBS-D who have bile-acid malabsorption [86,87,88]. A randomized controlled trial of patients with chronic, watery diarrhea or IBS-D and bile-acid malabsorption (n = 26) showed that clinical remission (i.e., mean of at most three stools per day in the week before the study visit, with fewer than one watery stool per day) was achieved by a greater percentage of patients receiving cholestyramine 4 g bid versus hydroxypropyl cellulose after 8 weeks, although the difference was not significant (53.8% vs 38.5%, respectively; P = 0.4) [88]. Bile-acid sequestrants currently are not recommended by the ACG for treatment of IBS-D but may be considered as a second-line approach for the management of diarrhea. By virtue of their mechanism of action, bile-acid sequestrants are expected to have less impact on abdominal pain symptoms.
Other Therapies
Exercise
Data from a randomized controlled trial of patients with IBS showed that an increase in physical activity improved both GI symptoms and the physical domains of the IBS Quality of Life questionnaire after 12 weeks [89]. The 2021 BSG guidelines state that regular exercise should be considered part of first-line therapy for patients with IBS [24].
Psychologic Therapies in IBS
Gut-directed psychotherapies (e.g., cognitive behavior therapy [CBT], hypnotherapy) effectively target the cognitive and affective factors that modulate IBS symptoms and can improve abdominal pain and altered bowel habits in patients with IBS [20]. Further, a systematic review and meta-analysis found CBT and hypnotherapy improved abdominal pain and overall response in patients with IBS compared with placebo, although differences between the interventions were not significant [90]. The ACG guideline for IBS management conditionally recommends GI-directed psychotherapies for the treatment of global IBS symptoms on the basis of very low-quality evidence [20].
Fecal Microbiota Transplantation
Fecal microbiota transplantation (FMT) involves the transfer of donor fecal matter by enema, endoscopy, or an oral pill [91]. A meta-analysis of seven randomized controlled studies reported that FMT did not significantly decrease global symptoms of IBS compared with placebo after 12 weeks (RR 0.8; 95% CI 0.4–1.3) [92]. For the three studies with 1-year follow-up data, FMT did not significantly improve global IBS symptoms compared with placebo (RR 0.9; 95% CI 0.7–1.1) [92]. Given that studies of FMT for treatment of IBS are limited, the ACG guideline for IBS management recommends against the use of FMT for treatment of global IBS symptoms [20]. Further, FMT is not an FDA-approved treatment for IBS-D.
Conclusions
Diagnosing IBS may be challenging, given that symptoms of IBS overlap with many other conditions that present in the primary-care setting. However, in the presence of symptoms, a “positive diagnostic strategy” establishing a diagnosis of IBS does not require extensive and costly laboratory testing [2]. Patients who are refractory to initial treatment approaches or those manifesting alarm symptoms should be referred to a gastroenterologist for further evaluation. A clear patient–provider relationship with reassurances regarding the nature of the condition and meaning of the diagnosis is needed, as this can improve outcomes and minimize unnecessary testing. Additionally, various nonpharmacologic and pharmacologic interventions are available and have shown varying degrees of success in patients with IBS-D. Providers will need to consider the profiles of the three FDA-approved agents for treatment of IBS-D. Some interventions (e.g., dietary modification, CBT) are best employed with the involvement of trained and experienced providers (i.e., dieticians, health psychologists).
Patients should be encouraged to communicate with their providers if they have an insufficient response to therapy or notice an increased impact on daily life, as these patients may require a gastroenterology referral. Furthermore, providers should refer patients with IBS with multiple comorbid conditions to a gastroenterologist, as these patients may experience more severe symptoms and tend to be more challenging to manage. Timely diagnosis of IBS-D and proper management, coupled with patient feedback on their symptom experiences and treatment responses, may optimize outcomes and reinforce the patient–provider relationship in individuals with this chronic condition.
References
Peery AF, Crockett SD, Murphy CC, et al. Burden and cost of gastrointestinal, liver, and pancreatic diseases in the United States: update 2018. Gastroenterology. 2019;156(1):254–72.
Lacy BE, Mearin F, Chang L, et al. Bowel disorders. Gastroenterology. 2016;150(6):1393–407.
Drossman DA. Functional gastrointestinal disorders: history, pathophysiology, clinical features, and Rome IV. Gastroenterology. 2016;150(6):1262–79.
Sperber AD, Bangdiwala SI, Drossman DA, et al. Worldwide prevalence and burden of functional gastrointestinal disorders, results of Rome Foundation Global Study. Gastroenterology. 2021;160(1):99–114.
Palsson OS, Whitehead W, Törnblom H, Sperber AD, Simren M. Prevalence of Rome IV functional bowel disorders among adults in the United States, Canada, and the United Kingdom. Gastroenterology. 2020;158(5):1262–73.
Choung RS, Unalp-Arida A, Ruhl CE, Brantner TL, Everhart JE, Murray JA. Less hidden celiac disease but increased gluten avoidance without a diagnosis in the United States: findings from the National Health and Nutrition Examination Surveys from 2009 to 2014. Mayo Clin Proc. 2017;92(1):30–8.
Ye Y, Manne S, Treem WR, Bennett D. Prevalence of inflammatory bowel disease in pediatric and adult populations: recent estimates from large national databases in the United States, 2007–2016. Inflamm Bowel Dis. 2020;26(4):619–25.
Chey WD, Kurlander J, Eswaran S. Irritable bowel syndrome: a clinical review. JAMA. 2015;313(9):949–58.
Linsalata M, Riezzo G, Clemente C, D’Attoma B, Russo F. Noninvasive biomarkers of gut barrier function in patients suffering from diarrhea predominant-IBS: an update. Dis Markers. 2020;2020:2886268.
Piche T, Barbara G, Aubert P, et al. Impaired intestinal barrier integrity in the colon of patients with irritable bowel syndrome: involvement of soluble mediators. Gut. 2009;58(2):196–201.
Pittayanon R, Lau JT, Yuan Y, et al. Gut microbiota in patients with irritable bowel syndrome–a systematic review. Gastroenterology. 2019;157(1):97–108.
Burns G, Carroll G, Mathe A, et al. Evidence for local and systemic immune activation in functional dyspepsia and the irritable bowel syndrome: a systematic review. Am J Gastroenterol. 2019;114(3):429–36.
Talley NJ, Alexander JL, Walker MM, et al. Ileocolonic histopathological and microbial alterations in the irritable bowel syndrome: a nested community case–control study. Clin Transl Gastroenterol. 2020;12(1): e00296.
Ford AC, Sperber AD, Corsetti M, Camilleri M. Irritable bowel syndrome. Lancet. 2020;396(10263):1675–88.
Simrén M, Tornblom H, Palsson OS, Van Oudenhove L, Whitehead WE, Tack J. Cumulative effects of psychologic distress, visceral hypersensitivity, and abnormal transit on patient-reported outcomes in irritable bowel syndrome. Gastroenterology. 2019;157(2):391–402.
Spiller R, Garsed K. Postinfectious irritable bowel syndrome. Gastroenterology. 2009;136(6):1979–88.
Barbara G, Grover M, Bercik P, et al. Rome foundation working team report on post-infection irritable bowel syndrome. Gastroenterology. 2019;156(1):46–58.
Scallan Walter EJ, Crim SM, Bruce BB, Griffin PM. Postinfectious irritable bowel syndrome after Campylobacter infection. Am J Gastroenterol. 2019;114(10):1649–56.
Schwille-Kiuntke J, Enck P, Zendler C, et al. Postinfectious irritable bowel syndrome: follow-up of a patient cohort of confirmed cases of bacterial infection with Salmonella or Campylobacter. Neurogastroenterol Motil. 2011;23(11):e479–88.
Lacy BE, Pimentel M, Brenner DM, et al. ACG Clinical Guideline: management of irritable bowel syndrome. Am J Gastroenterol. 2021;116(1):17–44.
Sood R, Gracie DJ, Law GR, Ford AC. Systematic review with meta-analysis: the accuracy of diagnosing irritable bowel syndrome with symptoms, biomarkers and/or psychological markers. Aliment Pharmacol Ther. 2015;42(5):491–503.
Shaukat A, Kahi CJ, Burke CA, Rabeneck L, Sauer BG, Rex DK. ACG clinical guidelines: colorectal cancer screening 2021. Am J Gastroenterol. 2021;116(3):458–79.
Asghar Z, Thoufeeq M, Kurien M, et al. Diagnostic yield of colonoscopy in patients with symptoms compatible with Rome IV functional bowel disorders. Clin Gastroenterol Hepatol. 2022;20(2):334-41.e3.
Vasant DH, Paine PA, Black CJ, et al. British Society of Gastroenterology guidelines on the management of irritable bowel syndrome. Gut. 2021;70(7):1214–40.
Petersen MW, Schröder A, Jørgensen T, et al. Irritable bowel, chronic widespread pain, chronic fatigue and related syndromes are prevalent and highly overlapping in the general population: DanFunD. Sci Rep. 2020;10(1):3273.
Shiha MG, Aziz I. Review article: physical and psychological comorbidities associated with irritable bowel syndrome. Aliment Pharmacol Ther. 2021;54(Suppl 1):S12–23.
Camilleri M. Bile acid diarrhea: prevalence, pathogenesis, and therapy. Gut Liver. 2015;9(3):332–9.
Catanzaro R, Sciuto M, Singh B, Pathak S, Marotta F. Irritable bowel syndrome and lactose intolerance: the importance of differential diagnosis A monocentric study. Minerva Gastroenterol (Torino). 2021;67(1):72–8.
Kim SB, Calmet FH, Garrido J, Garcia-Buitrago MT, Moshiree B. Sucrase-isomaltase deficiency as a potential masquerader in irritable bowel syndrome. Dig Dis Sci. 2020;65(2):534–40.
Lebwohl B, Rubio-Tapia A. Epidemiology, presentation, and diagnosis of celiac disease. Gastroenterology. 2021;160(1):63–75.
Rubio-Tapia A, Hill ID, Kelly CP, Calderwood AH, Murray JA. ACG clinical guidelines: diagnosis and management of celiac disease. Am J Gastroenterol. 2013;108(5):656–76.
Onyimba F, Crowe SE, Johnson S, Leung J. Food allergies and intolerances: a clinical approach to the diagnosis and management of adverse reactions to food. Clin Gastroenterol Hepatol. 2021;19(11):2230-40.e1.
Bischoff S, Crowe SE. Gastrointestinal food allergy: new insights into pathophysiology and clinical perspectives. Gastroenterology. 2005;128(4):1089–113.
Aguilera-Lizarraga J, Florens MV, Viola MF, et al. Local immune response to food antigens drives meal-induced abdominal pain. Nature. 2021;590(7844):151–6.
Menees SB, Powell C, Kurlander J, Goel A, Chey WD. A meta-analysis of the utility of C-reactive protein, erythrocyte sedimentation rate, fecal calprotectin, and fecal lactoferrin to exclude inflammatory bowel disease in adults with IBS. Am J Gastroenterol. 2015;110(3):444–54.
Sidhu R, Wilson P, Wright A, et al. Faecal lactoferrin–a novel test to differentiate between the irritable and inflamed bowel? Aliment Pharmacol Ther. 2010;31(12):1365–70.
Smalley W, Falck-Yttr C, Carrasco-Labra A, Wani S, Lytvyn L, Falck-Ytter Y. AGA clinical practice guidelines on the laboratory evaluation of functional diarrhea and diarrhea-predominant irritable bowel syndrome in adults (IBS-D). Gastroenterology. 2019;157(3):851–4.
Rao SS. Advances in diagnostic assessment of fecal incontinence and dyssynergic defecation. Clin Gastroenterol Hepatol. 2010;8(11):910–9.
Pimentel M, Saad RJ, Long MD, Rao SSC. ACG clinical guideline: small intestinal bacterial overgrowth. Am J Gastroenterol. 2020;115(2):165–78.
Almazar AE, Talley NJ, Larson JJ, Atkinson EJ, Murray JA, Saito YA. Celiac disease is uncommon in irritable bowel syndrome in the USA. Eur J Gastroenterol Hepatol. 2018;30(2):149–54.
Szałwińska P, Włodarczyk J, Spinelli A, Fichna J, Włodarczyk M. IBS-symptoms in IBD patients–manifestation of concomitant or different entities. J Clin Med. 2020;10(1):31.
Liu AH, Jaramillo R, Sicherer SH, et al. National prevalence and risk factors for food allergy and relationship to asthma: results from the National Health and Nutrition Examination Survey 2005–2006. J Allergy Clin Immunol. 2010;126(4):798–806.
Foley A, Halmos EP, Husein DM, et al. Adult sucrase-isomaltase deficiency masquerading as IBS. Gut. 2022;71(6):1237–8.
Henstrom M, Diekmann L, Bonfiglio F, et al. Functional variants in the sucrase-isomaltase gene associate with increased risk of irritable bowel syndrome. Gut. 2018;67(2):263–70.
Baker J, Eswaran S, Saad R, et al. Abdominal symptoms are common and benefit from biofeedback therapy in patients with dyssynergic defecation. Clin Transl Gastroenterol. 2015;6: e105.
Bharucha AE, Zinsmeister AR, Schleck CD, Melton LJ III. Bowel disturbances are the most important risk factors for late onset fecal incontinence: a population-based case-control study in women. Gastroenterology. 2010;139(5):1559–66.
Camilleri M, Vijayvargiya P. The role of bile acids in chronic diarrhea. Am J Gastroenterol. 2020;115(10):1596–603.
Chen B, Kim JJ, Zhang Y, Du L, Dai N. Prevalence and predictors of small intestinal bacterial overgrowth in irritable bowel syndrome: a systematic review and meta-analysis. J Gastroenterol. 2018;53(7):807–18.
Rezaie A, Buresi M, Lembo A, et al. Hydrogen and methane-based breath testing in gastrointestinal disorders: the North American Consensus. Am J Gastroenterol. 2017;112(5):775–84.
Chey WD, Hashash JG, Manning L, Chang L. AGA Clinical Practice Update on the role of diet in irritable bowel syndrome: expert review. Gastroenterology. 2022;162(6):1737–45.
Sturkenboom R, Keszthelyi D, Masclee AAM, Essers BAB. Discrete choice experiment reveals strong preference for dietary treatment among patients with irritable bowel syndrome. Clin Gastroenterol Hepatol. 2022. https://doi.org/10.1016/j.cgh.2022.02.016.
Kamal A, Pimentel M. Influence of dietary restriction on irritable bowel syndrome. Am J Gastroenterol. 2019;114(2):212–20.
Sayuk GS, Wolf R, Chang L. Comparison of symptoms, healthcare utilization, and treatment in diagnosed and undiagnosed individuals with diarrhea-predominant irritable bowel syndrome. Am J Gastroenterol. 2017;112(6):892–9.
Wright-McNaughton M, Ten Bokkel HS, Frampton CMA, et al. Measuring diet intake and gastrointestinal symptoms in irritable bowel syndrome: validation of the food and symptom times diary. Clin Transl Gastroenterol. 2019;10(12): e00103.
Halmos EP, Power VA, Shepherd SJ, Gibson PR, Muir JG. A diet low in FODMAPS reduces symptoms of irritable bowel syndrome. Gastroenterology. 2014;146(1):67–75.
Questran (cholestyramine for oral suspension USP) [press release]. Chestnut Ridge, NY: Par Pharmaceutical; 2018.
Skodje GI, Sarna VK, Minelle IH, et al. Fructan, rather than gluten, induces symptoms in patients with self-reported non-celiac gluten sensitivity. Gastroenterology. 2018;154(3):529–39.
Rangan V, Ballou S, Shin A, Camilleri M, Beth Israel Deaconess Medical Center GI Motility Working Group, Lembo A. Use of treatments for irritable bowel syndrome and patient satisfaction based on the IBS in America survey. Gastroenterology. 2020;158(3):786–88.
Ford AC, Harris LA, Lacy BE, Quigley EMM, Moayyedi P. Systematic review with meta-analysis: the efficacy of prebiotics, probiotics, synbiotics and antibiotics in irritable bowel syndrome. Aliment Pharmacol Ther. 2018;48:1044–60.
Gibson GR, Hutkins R, Sanders ME, et al. Expert consensus document: the International Scientific Association for Probiotics and Prebiotics (ISAPP) consensus statement on the definition and scope of prebiotics. Nat Rev Gastroenterol Hepatol. 2017;14(8):491–502.
Swanson KS, Gibson GR, Hutkins R, et al. The International Scientific Association for Probiotics and Prebiotics (ISAPP) consensus statement on the definition and scope of synbiotics. Nat Rev Gastroenterol Hepatol. 2020;17(11):687–701.
Hawthorn M, Ferrante J, Luchowski E, Rutledge A, Wei XY, Triggle DJ. The actions of peppermint oil and menthol on calcium channel dependent processes in intestinal, neuronal and cardiac preparations. Aliment Pharmacol Ther. 1988;2(2):101–18.
Alammar N, Wang L, Saberi B, et al. The impact of peppermint oil on the irritable bowel syndrome: a meta-analysis of the pooled clinical data. BMC Complement Altern Med. 2019;19(1):21.
Zhou Q, Verne ML, Fields JZ, et al. Randomised placebo-controlled trial of dietary glutamine supplements for postinfectious irritable bowel syndrome. Gut. 2019;68(6):996–1002.
Efskind PS, Bernklev T, Vatn MH. A double-blind placebo-controlled trial with loperamide in irritable bowel syndrome. Scand J Gastroenterol. 1996;31(5):463–8.
Lomotil Cv (diphenoxylate hydrochloride and atropine sulfate tablets, USP) tablets; (diphenoxylate hydrochloride and atropine sulfate oral solution, USP) liquid [package insert]. New York, NY: Pfizer; 2005.
Harford WV, Krejs GJ, Santa Ana CA, Fordtran JS. Acute effect of diphenoxylate with atropine (Lomotil) in patients with chronic diarrhea and fecal incontinence. Gastroenterology. 1980;78(3):440–3.
Xifaxan (rifaximin) tablets, for oral use [package insert]. Bridgewater, NJ: Salix Pharmaceuticals; 2020.
Pimentel M, Lembo A, Chey WD, et al. Rifaximin therapy for patients with irritable bowel syndrome without constipation. N Engl J Med. 2011;364(1):22–32.
Lembo A, Pimentel M, Rao SS, et al. Repeat treatment with rifaximin is safe and effective in patients with diarrhea-predominant irritable bowel syndrome. Gastroenterology. 2016;151(6):1113–21.
Lotronex (alosetron hydrochloride) tablets [package insert]. Roswell, GA: Sebela Pharmaceuticals Inc.; 2019.
US Food and Drug Administration. Postmarket drug safety information for patients and providers. Lotronex (alosetron hydrochloride) information. http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/ucm110450.htm. Accessed April 22 2022.
Alosetron REMS - Homepage. https://www.alosetronrems.com/AlosetronUI/rems/home.action. Accessed April 22 2022.
Zheng Y, Yu T, Tang Y, et al. Efficacy and safety of 5-hydroxytryptamine 3 receptor antagonists in irritable bowel syndrome: a systematic review and meta-analysis of randomized controlled trials. PLoS ONE. 2017;12(3): e0172846.
Tong K, Nicandro JP, Shringarpure R, Chuang E, Chang L. A 9-year evaluation of temporal trends in alosetron postmarketing safety under the risk management program. Therap Adv Gastroenterol. 2013;6(5):344–57.
Viberzi (eluxadoline) tablets, for oral use, CIV [package insert]. Madison, NJ: Allergan USA, Inc.; 2020.
Lembo AJ, Lacy BE, Zuckerman MJ, et al. Eluxadoline for irritable bowel syndrome with diarrhea. N Engl J Med. 2016;374(3):242–53.
Shah E, Kim S, Chong K, Lembo A, Pimentel M. Evaluation of harm in the pharmacotherapy of irritable bowel syndrome. Am J Med. 2012;125(4):381–93.
Ford AC, Moayyedi P, Chey WD, et al. American College of Gastroenterology monograph on management of irritable bowel syndrome. Am J Gastroenterol. 2018;113(Suppl 2):1–18.
Ford AC, Quigley EM, Lacy BE, et al. Efficacy of prebiotics, probiotics, and synbiotics in irritable bowel syndrome and chronic idiopathic constipation: systematic review and meta-analysis. Am J Gastroenterol. 2014;109(10):1547–61.
Lee C, Doo E, Choi JM, et al. The increased level of depression and anxiety in irritable bowel syndrome patients compared with healthy controls: systematic review and meta-analysis. J Neurogastroenterol Motil. 2017;23(3):349–62.
Fond G, Loundou A, Hamdani N, et al. Anxiety and depression comorbidities in irritable bowel syndrome (IBS): a systematic review and meta-analysis. Eur Arch Psychiatry Clin Neurosci. 2014;264(8):651–60.
Hu Z, Li M, Yao L, et al. The level and prevalence of depression and anxiety among patients with different subtypes of irritable bowel syndrome: a network meta-analysis. BMC Gastroenterol. 2021;21(1):23.
Ford AC, Lacy BE, Harris LA, Quigley EMM, Moayyedi P. Effect of antidepressants and psychological therapies in irritable bowel syndrome: an updated systematic review and meta-analysis. Am J Gastroenterol. 2019;114(1):21–39.
Drossman DA, Tack J, Ford AC, Szigethy E, Törnblom H, Van Oudenhove L. Neuromodulators for functional gastrointestinal disorders (disorders of gut-brain interaction): a Rome Foundation Working Team report. Gastroenterology. 2018;154(4):1140–71.
Camilleri M, Acosta A, Busciglio I, et al. Effect of colesevelam on faecal bile acids and bowel functions in diarrhoea-predominant irritable bowel syndrome. Aliment Pharmacol Ther. 2015;41(5):438–48.
Vijayvargiya P, Camilleri M, Taylor A, Busciglio I, Loftus EV Jr, Donato LJ. Combined fasting serum C4 and primary bile acids from a single stool sample to diagnose bile acid diarrhea. Gastroenterology. 2020;159(5):1952–4.
Fernández-Bañares F, Rosinach M, Piqueras M, et al. Randomised clinical trial: colestyramine vs hydroxypropyl cellulose in patients with functional chronic watery diarrhoea. Aliment Pharmacol Ther. 2015;41(11):1132–40.
Johannesson E, Simrén M, Strid H, Bajor A, Sadik R. Physical activity improves symptoms in irritable bowel syndrome: a randomized controlled trial. Am J Gastroenterol. 2011;106(5):915–22.
Billings W, Mathur K, Craven HJ, Xu H, Shin A. Potential benefit with complementary and alternative medicine in irritable bowel syndrome: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2021;19(8):1538–53.
Vaughn BP, Rank KM, Khoruts A. Fecal microbiota transplantation: current status in treatment of GI and liver disease. Clin Gastroenterol Hepatol. 2019;17(2):353–61.
Wu J, Lv L, Wang C. Efficacy of fecal microbiota transplantation in irritable bowel syndrome: a meta-analysis of randomized controlled trials. Front Cell Infect Microbiol. 2022;12: 827395.
Acknowledgements
Funding
Salix Pharmaceuticals provided funding and support for technical editorial and medical writing assistance and funded the journal’s Rapid Service and Open Access fees. Salix Pharmaceuticals did not actively contribute to the content or have a role in the decision to submit, but did review the final copy. The authors did not receive any compensation for development of this manuscript.
Medical Writing and Editorial Assistance
Technical editorial and medical writing assistance were provided, under direction of the authors, by Mary Beth Moncrief, PhD, and Sophie Bolick, PhD, Synchrony Medical Communications, LLC, West Chester, PA. Funding for this assistance was provided by Salix Pharmaceuticals, Bridgewater, NJ.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship of this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Authors’ Contributions
All authors were involved in planning of the manuscript, collecting resources, interpreting the data, writing, and critically revising the manuscript. All authors read and approved the final manuscript.
Disclosures
Baha Moshiree is a consultant for Salix Pharmaceuticals. She is also on advisory boards for Allergan, AbbVie, Alnylam, and Ironwood Pharmaceuticals; and has research support from Salix, AbbVie, and Medtronic. Grant support: Bausch Pharmaceuticals and Phathom. Joel J. Heidelbaugh reports no conflicts of interest. Gregory S. Sayuk reports having served as a consultant for AbbVie, Ironwood, Salix, and Alnylam Pharmaceuticals; and as a speaker for Salix Pharmaceuticals, Synergy, AbbVie, Ironwood, and Alnylam Pharmaceuticals.
Compliance with Ethics Guidelines
This review is based on previously conducted studies and does not contain any new data from human or animal studies conducted by any of the authors.
Data Availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Moshiree, B., Heidelbaugh, J.J. & Sayuk, G.S. A Narrative Review of Irritable Bowel Syndrome with Diarrhea: A Primer for Primary Care Providers. Adv Ther 39, 4003–4020 (2022). https://doi.org/10.1007/s12325-022-02224-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-022-02224-z