Abstract
Introduction
Reliable cost and resource use data for COVID-19 hospitalizations are crucial to better inform local healthcare resource decisions; however, available data are limited and vary significantly.
Methods
COVID-19 hospital admissions data from the Premier Healthcare Database were evaluated to estimate hospital costs, length of stay (LOS), and discharge status. Adult COVID-19 patients (ICD-10-CM: U07.1) hospitalized in the US from April 1 to December 31, 2020, were identified. Analyses were stratified by patient and hospital characteristics, levels of care during hospitalization, and discharge status. Factors associated with changes in costs, LOS, and discharge status were estimated using regression analyses. Monthly trends in costs, LOS, and discharge status were examined.
Results
Of the 247,590 hospitalized COVID-19 patients, 49% were women, 76% were aged ≥ 50, and 36% were admitted to intensive care units (ICU). Overall median hospital LOS, cost, and cost/day were 6 days, US$11,267, and $1772, respectively; overall median ICU LOS, cost, and cost/day were 5 days, $13,443, and $2902, respectively. Patients requiring mechanical ventilation had the highest hospital and ICU median costs ($47,454 and $41,510) and LOS (16 and 11 days), respectively. Overall, 14% of patients died in hospital and 52% were discharged home. Older age, Black and Caucasian race, hypertension and obesity, treatment with extracorporeal membrane oxygenation, and discharge to long-term care facilities were major drivers of costs, LOS, and risk of death. Admissions in December had significantly lower median hospital and ICU costs and LOS compared to April.
Conclusion
The burden from COVID-19 in terms of hospital and ICU costs and LOS has been substantial, though significant decreases in cost and LOS and increases in the share of hospital discharges to home were observed from April to December 2020. These estimates will be useful for inputs to economic models, disease burden forecasts, and local healthcare resource planning.
Similar content being viewed by others
Why carry out this study? |
Published reports citing healthcare resource utilization and costs for COVID-19 hospitalization in the United States vary widely |
Some reports also confuse hospital costs with hospital charges, and most were not from COVID-19 patient data |
A comprehensive analysis of COVID-19 hospitalization costs is essential to identify underlying determinants and observed trends for this rapidly evolving pandemic |
What was learned from the study? |
Overall median hospital length of stay, cost, and cost/day were 6 days, $11,267, and $1772, respectively. Older age, comorbidities, and mechanical ventilation were major drivers of costs, hospital length of stay, and risk of death. A downward trend of cost and hospital stay was observed from April to December 2020 |
These results highlight the significant burden from COVID-19 in the US in terms of hospital costs and length of stay |
These estimates will be useful for inputs to economic models, disease burden forecasts, and local healthcare resource decisions |
Introduction
Coronavirus disease 2019 (COVID-19) is imposing a substantial burden on the United States (US) healthcare system [1]. As of July 2021, 33.8 million confirmed COVID-19 cases and 605,905 associated deaths have been reported by the Centers for Disease Control and Prevention in the US. [2]. Precautionary measures such as social distancing and quarantine to slow the spread of COVID-19 have impacted psychological health and inter-personal lives, while also leading to economic downturn and job losses, especially in socioeconomically disadvantaged communities [1, 3].
COVID-19 primarily affects the respiratory system, followed by cardiovascular, hepatic, renal, gastrointestinal, and central nervous systems. Pneumonia-related respiratory symptoms including breathlessness and respiratory failure are the common clinical manifestations of COVID-19 [4]. According to previous reports, among all hospitalized patients with COVID-19, approximately 14–30% developed acute respiratory distress syndrome, with an associated mortality rate of 45–75% [5, 6]. Approximately one-third of COVID-19 survivors who had severe or critical disease are likely to have long-term clinical and mental health complications with an increased risk of premature death [7]. The severity of the disease is positively correlated with age, males, and underlying comorbidities, including cardiovascular disease, chronic kidney disease, chronic lung disease, diabetes, obesity, and malignancy.
The US Food and Drug Administration recommends multiple therapies to reduce inflammation and repair damage to ailing lungs due to COVID-19. Such treatments include neutralizing antibodies (bamlanivimab, etesevimab, casirivimab, and imdevimab), and anti-inflammatory and antiviral therapies (baricitinib and remdesivir) [8]. However, all these medications are approved under emergency use authorization and require more data to support their effectiveness in patients with severe disease. In addition, although an increasing number of patients are being vaccinated, questions related to dose and administrations are yet to be answered [9]. Therefore, supplemental oxygenation via mechanical ventilation (MV) or non-MV remains an essential part of the management of hospitalized COVID-19 patients with severe respiratory failure.
Published reports citing healthcare resource utilization and costs for COVID-19 hospitalization in the US vary widely between studies, and the majority were not derived from data from actual COVID-19 patients [10,11,12]. In addition, some reports conflate hospital costs with hospital charges [13]. A recent observational study reported descriptive data for COVID-19 hospitalization [14]; however, the underlying factors for the reported increases in hospitalization costs have not been assessed.
Due to the wide variation in estimates from multiple sources, a more comprehensive analysis of the healthcare resource utilization and costs associated with COVID-19 hospitalization is required. In addition, identifying important underlying determinants and examining observed trends is essential for this rapidly evolving pandemic. Here, we present estimates of COVID-19-related inpatient costs and length of stay (LOS), at both overall hospital and intensive care unit (ICU)-specific level, for various patient subgroups and investigate the factors influencing these estimates using a large and nationally representative hospital database.
Methods
Data Source and Population
This observational study utilized inpatient hospital admissions and discharge records of adult patients with a diagnosis for COVID-19 from the Premier Healthcare Database (PHD) [15]. The PHD is a large patient-level information system that can be used for clinical and financial comparative analysis. It includes discharge records from more than 800 non-governmental, community, and academic hospitals across the US. The database represents about one in five of all-cause inpatient discharges in the US. The PHD records were de-identified to protect patients’ privacy and are fully compliant with the US health information privacy requirements, including the Health Insurance Portability and Accountability Act of 1996. This is an observational study that uses previously collected data and does not impose any form of intervention, and was performed in accordance with the Helsinki Declaration of 1964 and its later amendments.
Adult patients (aged ≥ 18 years) who had at least one report of COVID-19 diagnosis [International Classification of Disease, Tenth Revision, Clinical Modification (ICD-10-CM) code: U07.1], and valid discharge status during the study period, April 1 to December 31, 2020, were included in this analysis. The diagnostic code U07.1 was shown to have high sensitivity (98.01%) and specificity (99.04%) to identify COVID-19 cases in real-world data since it has been widely adopted by hospitals in the US [16].
Outcomes and Measures
Total and daily hospital costs, total and daily ICU costs, hospital LOS, ICU LOS, and discharge status were the main outcomes of this study. Only the first hospitalization for each patient was included in this analysis (approximately 4% of patients had more than 1 hospitalization in the PHD).
Patient characteristics included sex, age, race, ethnicity, and comorbidities [asthma, autoimmune disease, chronic obstructive pulmonary disease (COPD), diabetes, hypertension, and obesity]. Hospital characteristics included geographic region, area of hospitalization (urban or rural), hospital status (community or academic), hospital size (based on number of beds), and insurance payer mix.
ICU admissions were identified based on recorded ICU Current Procedural Terminology, 4th Edition (CPT-4) codes or charge master codes. Total hospital and ICU costs were calculated as the sum of medical and medication costs accrued during the hospital or ICU stay. Daily hospital or ICU costs were calculated as total hospital cost divided by LOS at the hospital or ICU, respectively.
The main outcomes were stratified based on subgroups including patient characteristics, hospital characteristics, levels of care according to the ordinal scale defined in the Adaptive COVID-19 Treatment Trial Ordinal Scale (ACTT OS) [17, 18], and 15 most frequent Medicare Severity Diagnosis-Related Groups (MS-DRG).
The level of care was estimated according to the ACTT OS scores based on oxygen procedures received by patients during hospitalization. Patients were categorized into five ACTT OS groups based on oxygen treatments: no supplemental oxygen (ACTT OS 3/4), supplemental oxygen (ACTT OS 5), non-invasive ventilation or high-flow oxygen (ACTT OS 6), invasive MV or extracorporeal membrane oxygenation (ECMO) (ACTT OS 7), and death (ACTT OS 8).
The underlying determinants or predictors for the differences in costs, LOS, and discharge status were analyzed using univariate and multivariate regression analyses with the following variables: patient characteristics, hospital characteristics, (level of care) ACTT OS, MS-DRG codes, month of discharge status, and month of hospitalization.
For patients with zero total hospital and ICU costs reported on the hospital record, no imputations were performed, thus these patients were not included in the cost analyses. In addition, costs were trimmed to reduce the impact of extremely low (below 1st percentile) or high costs (above 99th percentile), as done in other hospital cost studies [19].
Statistical Analysis
Descriptive analysis of the data is reported as frequency, mean, median, and standard deviation. To compare the costs and LOS within groups, adjusting for patient and hospital level characteristics, a multivariate log-linear regression was fitted including age groups, sex, race, ethnicity, geographic region, comorbidity, hospital type, urban status, payer type, ACTT OS, MS-DRG codes, discharge status, and admission month, while dependent variables (costs, LOS) were log-transformed. The least square (LS) means and LS means differences, along with 95% confidence intervals (CIs) and P values were presented. Discharge status within groups was compared, adjusting for patient- and hospital-level characteristics, by using a logistic regression fitted with covariates of age groups, sex, race, ethnicity, geographic region, comorbidity, hospital type, urban status, payer type, ACTT OS, MS-DRG codes, and admission month. Odds ratios (OR), CIs, and a P values were reported. A P value of ≤ 0.05 was considered as statistically significant. Multiple group comparisons were adjusted with a Bonferroni correction. A comparison of key outcomes (inpatient costs, LOS, hospital discharge status) by month was conducted. Sample selection and the creation of analytic variables were performed using the Instant Health Data platform (Panalgo, Boston, MA, USA). The regression models were estimated using SAS v.9.4 (SAS Institute, Cary, NC, USA).
Results
From a total of 770,397 patients with a diagnosis of COVID-19 in the PHD database, 247,590 hospitalized patients were included in this study. Attrition of patients is presented in Fig. 1.
Overall, 49% of patients were women, 87% were aged above 40 years, and 60% were Caucasian. The most frequent comorbidity was hypertension, followed by diabetes, and obesity. About 90% of patients were hospitalized in urban areas and 48% patients were from the Southern region of the US. Almost two-thirds (> 65%) of the patients had government (Medicare or Medicaid) insurance and 24% were commercially insured. In total, 198,806 patients were evaluated for hospital costs after excluding low- and high-cost outliers. The median total hospital costs were $11,267 and hospital costs/day were $1772. Among all hospitalized patients, 88,530 were admitted to ICU and 70,054 (with cost information) were included in the ICU cost analyses. Median ICU total costs were $13,443 and costs/day were $2902. Overall, the median LOS in hospital was 6 days and, among patients admitted to ICU, the median ICU LOS was 5 days (Fig. 2a, b; Tables S1a, S1b, S4).
Hospital Cost and Length of Stay by Patient Characteristics
Cost and LOS estimates stratified by patient characteristics are presented in Fig. 2a, b (hospital and ICU) and Tables S1a (hospital), and S1b (ICU). Among all hospitalized patients, the median cost was highest for men ($12,237), Asians ($12,785), patients aged 70–79 ($13,181), and those with COPD ($13,582). The median LOS generally was similar across patient demographic groups; the highest LOS (7 days) was for men, those aged > 60 years, and those with autoimmune disease, COPD, diabetes, hypertension, and obesity (Table S1a). Among patients admitted to ICU, the median costs were highest for men ($14,468), other race ($18,247), patients aged 60–69 ($16,540), and those with obesity ($16,330). The median ICU cost/day was comparable across the groups. The median ICU LOS was highest for patients with obesity (6 days) (Table S1b).
Hospital Cost and Length of Stay by Hospital Characteristics
Cost and LOS estimates stratified by hospital characteristics are presented in Fig. 3a, b (hospital and ICU) and Tables S2a (hospital) and S2b (ICU). The median total hospital costs and median hospital cost/day were highest for patients from the Northeast region ($14,497 and $2263, respectively). The highest median LOS (7 days) was for patients from the Western region, admitted to hospitals with over 500 beds, or with Medicare insurance (Table S2a). Among patients who were admitted to ICU, the highest median costs and median cost/day were recorded in patients from the Northeast ($19,727, and $4136, respectively). The median LOS was 5 days for patients hospitalized from the Midwest, Northeast, and Western regions, in urban hospitals, academic and community hospitals, and hospitals with over 300 beds, and who had Medicare or Medicaid insurance (Table S2b).
Hospital Cost and Length of Stay by ACTT OS Scores, and MS-DRG Codes
The main outcomes stratified based on the levels of care (ACTT OS) are presented in Fig. 4a, b (hospital and ICU) and Tables S3a (hospital) and S3b (ICU); and the most frequent MS-DRGs (9 respiratory, 3 sepsis, 2 renal failure, and 1 cardiovascular-related) are presented in Tables S3a (hospital) and S3b (ICU). Over half (n/N: 106,924/198,806 = 54%) of patients did not require supplemental oxygen (ACTT OS 3/4), while 28% (n = 54,772) required supplemental oxygen (ACTT OS 5), 7% (n = 13,705) required non-invasive MV or high-flow oxygen (ACTT OS 6) and 12% (n = 23,405) required invasive MV or ECMO (ACTT OS 7). Hospital and ICU costs and LOS increased with the requirement of supplemental oxygen and the use of non-invasive to invasive MV. The highest median hospital costs were reported for ACTT OS 7 (required ECMO) ($47,454) (Fig. 4a, Table S3a).
COVID-19 hospital and ICU total costs (a) and costs/day (b) by level of care (ACTT OS). ACTT OS were estimated using the oxygen procedures received by patients during the hospitalization. ACTT OS 3/4 no supplemental oxygen, ACTT OS 5 supplemental oxygen, ACTT OS 6 non-invasive ventilation or high-flow oxygen, ACTT OS 7 ECMO using invasive mechanical ventilation, ACTT OS 8 death; ACTT OS Adaptive COVID-19 Treatment Trial ordinal scale
Among patients who died in hospital (ACTT OS 8), the median hospital cost was $24,973 and median hospital cost/day was $2,685 (Fig. 4a; Table S3a), the median ICU cost was $27,742 and ICU cost/day was $3,757 (Fig. 4b; Table S3b), while the median hospital LOS was 10 days (Table S3a), and the median ICU LOS was 8 days (Table S3b).
The most frequent MS-DRG code was 177 [respiratory infections and inflammations with major complication or comorbidity (MCC)] (50.3%: 99,963 of 198,806 patients). Although infrequent, the median hospital cost and LOS were highest for MS-DRG code 4 (tracheostomy with MV > 96 h or principal diagnosis except face, mouth, and neck without major operating room procedure: $114,182, and 40 days, respectively) (Table S3a). Among patients who were admitted to ICU, the median cost and LOS were highest for MS-DRG code 4) ($114,674, and 33 days, respectively) (Table S3b).
Discharge Status by Patients and Hospital Characteristics, ACTT OS, and MS-DRG Codes
Discharge status stratified by patient and hospital characteristics is presented in Table 1. Discharges to home were similar by sex; however, males were more likely to be deceased at discharge (16%) compared with females (12%). The proportion of patients who died or were discharged to a skilled nursing facility was seen to increase with age. Death or discharge to a skilled nursing facility was common among older patients who were aged > 60 years (> 70%), with comorbid COPD (> 20%), from the Northeast region (> 17%), hospitalized in urban areas (> 25%), and covered by Medicare insurance (~ 20%). Overall, 52% (129,046/247,590) of patients were discharged home, 12% (25,599/247,590) were discharged to a skilled nursing facility, and 13.7% (33,917/247,590) died in hospital (Table S5).
Discharge status stratified by levels of care and MS-DRG groups is presented in Table 2. With the increase in ACTT OS, home discharge decreased while discharge due to death increased. While discharge home was most frequent for ACTT OS 3/4 (62%), discharge due to death was more common in ACTT OS 7 (61%). Among patients stratified based on MS-DRG codes, discharge due to death was more frequent for MS-DRG codes 189, 190, 193 (pulmonary edema and respiratory failure, COPD with MCC, and simple pneumonia and pleurisy with MCC, respectively; > 65%).
Determinants of Costs and Length of Stay
Determinants of hospital and ICU costs and LOS are presented in Tables 3 (hospital) and 4 (ICU), and Table S3 (descriptive analysis of cost versus month of admission). Hospital costs for males were significantly higher compared to females [least square mean difference (△) $2474; P < 0.0001], while costs versus patients aged 18–29 years ranged from △ $952 for age 30–39 years to △ $5196 for age 60–69; both P < 0.001). The mean cost was significantly higher in patients from the Northeast (△ $7283) and West (△ $5817) compared with the Midwest (P < 0.0001). Patients hospitalized in urban areas accrued higher mean costs (△ $2131) compared with rural areas (P < 0.0001).
By race/ethnicity, mean costs were significantly lower in Blacks and Caucasians (− △ $2872 and − △ $2794, respectively) versus Asians (all P < 0.0001). Non-Hispanics had a lower mean cost (− △ $3284) compared with Hispanics (P < 0.0001).
Among patients with comorbid conditions, mean cost was higher in obese patients (△ $2161) and in diabetic patients (△ $1892) versus those without obesity or diabetes (both P < 0.0001), respectively. Overall cost increased with the intensity of oxygen care (e.g., invasive MV). Patients who received the highest level of care (ACTT OS 7) had a higher mean hospital cost (△ $44,517) and longer mean LOS (△ 12 days) compared with patients who did not receive oxygen during the hospital stay (all P < 0.0001). Patients discharged to long-term hospital care were associated with a significantly higher mean hospital cost (△ $24,110) compared with patients discharged home (P < 0.0001). Compared with patients hospitalized in April 2020, for patients hospitalized in May 2020 the cost was significantly higher (△ $1054, P < 0.0001), while the costs of hospitalization in all months from June to December were significantly lower (all P < 0.0001) (Table 3). Further, a descriptive analysis showed a decreasing trend in median hospital and ICU costs from April 2020 ($14,412, and $19,034, respectively) to December 2020 ($6967, and $6657, respectively). The median hospital and ICU LOS was decreased from April 2020 (7 days and 6 days, respectively) to December 2020 (4 days and 3 days, respectively) (Table S6).
Among patients admitted to ICU, the mean cost and LOS also increased with the following regressors: male sex, older age, Asian race (vs. Blacks and Caucasians), Hispanic ethnicity (vs. non-Hispanics), Medicaid insurance (vs. Commercial insurance), asthma, diabetes and obesity (without respective comorbidities), levels of care (vs. ACTT OS 3/4), hospital size (> 99 vs. < 99 beds), and all discharge categories (vs. home discharge). Mean ICU cost/day differences versus April 2020 ranged from △ $319 (September) to − △ $235 (November) (Table 4).
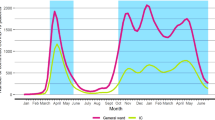
Determinants of Discharge Status
Multivariable logistic regression analyses on predictors of discharge status are provided in Table 5, Fig. 5a and b (discharge status versus month of admission), and Table S7 (descriptive data discharge status versus month of admission). The odds to be discharged to home decreased with age, (for age 70–79, the OR was 0.156 and for age 80–89, the OR was 0.054 relative to patients aged 18–29), and by ACTT OS level (for ACTT OS 6, the OR was 0.383 and for ACTT OS 7, the OR was 0.04 relative to ACTT OS 3/4 level), while the odds of death increased in age and by ACTT OS levels. Requirement of supplemental oxygen including ECMO (ACTT OS 5 to 7) increased the odds of discharge to long-term care facilities [for ECMO OR (95% CI): 10.112 (8.799–11.621) compared to ACTT OS 3/4] (Table 5).
The odds of home discharge were higher from June to December, compared to April, with the highest odds of home discharge in December [OR (95% CI): 2.221 (1.950–2.529)]. In addition, the odds of death were lower from May to December, compared to April, with the lowest odds of death in December [OR (95% CI): 0.411 (0.328–0.514)] (Fig. 5a, b). Further, a descriptive analysis showed that discharge status varied with the month of hospital admissions. Overall, the proportion of specialty care (other than home) discharge decreased from April to December 2020. Maximum death was reported in the month of April, which decreased to the month of December, while the proportion of patients discharged home increased from 41 to 61%, discharge to a skilled nursing facility decreased from 15.3% to 9.4%, and deaths decreased from 21.8 to 7.3% by December 2020 (Table S7).
Discussion
Demographics and clinical characteristics of patients analyzed in this study are consistent with previous studies on hospitalized COVID-19 patients identified from the PHD, with some differences [14, 20, 21]. Our results revealed that COVID-19 imposes a substantial burden on hospitals and patients, resulting in high costs, LOS, and ICU use, a large proportion of patients requiring post-acute care, and significant mortality among several patient subgroups. Previous studies that reported the cost of hospitalization in patients with COVID-19 were mostly based on assumptions or non-COVID-19 cost data reported with respect to related disease conditions such as pneumonia [10, 19].
To the best of our knowledge, the only study that reported hospital charges and costs data for COVID-19 patients was conducted by Di Fusco et al. [14] and studied 173,942 patients hospitalized with COVID-19 identified from the PHD during April 1 to October 31, 2020. Results from that study showed that 22% of all patients were admitted to the ICU and 16.9% received invasive MV. Consistent with our study, Di Fusco et al. also reported that the median hospital LOS was 5 days and median hospital costs were $12,046. The hospital LOS and costs increased up to 15 days in patients who used invasive MV in ICU admission. They also reported that government insurance and severity of disease were associated with increased LOS and costs [14]. However, unlike previous studies, more patients were admitted to ICU in our study (10–19% vs. ~ 36% in our study, respectively) [6, 14, 20, 21].
Although there are some similarities with the study conducted by Di Fusco et al., the present study is unique in several ways. Firstly, our study is the first to report adjusted results using multivariate log-linear and logistic regression analyses to identify the major drivers of costs, LOS, and discharge status. In addition, we have stratified cost, LOS, and discharge data based on ACTT OS scores and MS-DRG codes. Furthermore, our study provides important new results by month to show significant time trends in costs and outcomes.
Treatments that can reduce time to recovery and limit progression of disease towards requiring higher levels of oxygen support (invasive/non-invasive MV) may lead to better outcomes for patients, as well as conserving scarce resources for hospitals. The multivariate analyses further confirmed the trend observed in the descriptive analysis. The log-linear regression showed that age, comorbidity, Northeast region, and Medicare insurance, along with requirement of supplemental oxygen including ECMO via invasive MV, and discharge of patients to long-term care facilities or death were the major drivers of costs and LOS. The multivariable logistic regression showed that major factors for discharge due to death were higher age and ACTT OS 7. The OR for death was 11.6 for patients aged 70–79 versus those aged 18–29 years. Similarly, the OR for death was 54.1 for patients with ACTT OS of 7. Overall, teaching status and the size of hospitals had little impact on cost and discharge status.
We also observed a downward trend of LOS, cost, discharge to post-acute care, and discharge due to death from April to December 2020. Over this time period, there was almost a 50% reduction in median hospital costs. The median LOS and median ICU LOS both fell by 3 days over the study period, while the median ICU costs decreased by 35%. Discharge status improved from April to December 2020 with an increase of home discharge by 20%, whereas discharge due to death fell by 14%. A recent report also showed that in-hospital mortality, LOS, and use of mechanical ventilation in patients with COVID-19 decreased from March/April to September/November 2020 (mortality fell from 19 to 11%, LOS fell from 10.7 to 7.5 days, and use of mechanical ventilation fell from 23.3 to 13.9% of patients) [22]. The trend of decrease in mortality and cost from our analyses may be associated with improved understanding of the pathophysiology of COVID-19 with time and the associated availability and implementation of newer treatment protocols, including increased use of medications such as glucocorticoids and remdesivir [22].
The results of our study suggest that reducing time to recovery by only one hospital day may save $2118 per patient/day on average, and, if applied to the 198,806 patients in our cost analysis alone, the cost savings would exceed $421 million. Reducing ICU LOS by one day would save $3586 per patient/day on average, and over $251 million based on the 70,054 ICU patients in our cost analysis. In addition, efficacious therapies could reduce the burden on post-acute care facilities. These data will be useful as inputs for cost-effectiveness models to evaluate the potential impacts of COVID-19 prevention and treatment efforts.
Although the present study has multiple strengths, including a large sample size, robust analyses, and predictor model of inpatient hospitalization costs and trends, it has several limitations which can be expected from any observational study; hence, results of this study should be interpreted with caution. Apart from the possibility of coding errors, these results may not be generalizable to other populations beyond those identified in the PHD. In addition, private for-profit hospitals are underrepresented in the study sample. Moreover, indirect costs and rehospitalizations were not assessed, although previous research has shown that 9% of COVID-19 survivors required readmission during the early phase of this pandemic [20]. Overall, ~ 18% of the patients did not have cost information due to incomplete financial reconciliation and a resultant delay in submission of hospital cost data to the PHD system. For this reason, incomplete cost information was more common among patients hospitalized later in the study period. Furthermore, a subset of patients with cost data outside the 1st and 99th percentiles were excluded in the cost analysis to reduce skewness in cost data.
Therefore, further studies are warranted in other care settings and databases. Nevertheless, results of this study provide important insights into the economic burden and changes over time associated with COVID-19 in the US.
Conclusions
Results of this study showed that the total median length of stay in hospital was 6 days and the median total hospital cost was $11,267. The median length of stay in ICU was 5 days and median total ICU cost was $13,443. This study is the first comprehensive analysis of healthcare resource use and hospital costs due to COVID-19 cases in the United States, using a large, nationally representative hospital database. These estimates will be useful for inputs to economic models, disease burden forecasts, and local healthcare resource decisions.
References
Nicola M, Alsafi Z, Sohrabi C, et al. The socio-economic implications of the coronavirus pandemic (COVID-19): a review. Int J Surg. 2020;78:185–93.
Centers for Disease Control and Prevention. COVID data tracker weekly review. 2021. https://www.cdc.gov/coronavirus/2019-ncov/covid-data/covidview/index.html.
Hatef E, Chang H-Y, Kitchen C, Weiner JP, Kharrazi H. Assessing the impact of neighborhood socioeconomic characteristics on COVID-19 prevalence across seven states in the United States. Front Public Health. 2020;8:571808.
Miller IF, Becker AD, Grenfell BT, Metcalf CJE. Disease and healthcare burden of COVID-19 in the United States. Nat Med. 2020;26:1212–7.
Tzotzos SJ, Fischer B, Fischer H, Zeitlinger M. Incidence of ARDS and outcomes in hospitalized patients with COVID-19: a global literature survey. Crit Care. 2020;24:516.
Potere N, Valeriani E, Candeloro M, et al. Acute complications and mortality in hospitalized patients with coronavirus disease 2019: a systematic review and meta-analysis. Crit Care. 2020;24:389.
Best JH, Mohan SV, Kong AM, et al. Baseline demographics and clinical characteristics among 3471 US patients hospitalized with COVID-19 and pulmonary involvement: a retrospective study. Adv Ther. 2020;37:4981–95.
US Food and Drug Administration. Coronavirus disease 2019 (COVID-19) EUA information. 2019. https://www.fda.gov/emergency-preparedness-and-response/mcm-legal-regulatory-and-policy-framework/emergency-use-authorization.
US Food and Drug Administration. FDA statement on following the authorized dosing schedules for COVID-19. 2020. https://www.fda.gov/news-events/press-announcements/fda-statement-following-authorized-dosing-schedules-covid-19 vaccines.
Bartsch SM, Ferguson MC, McKinnell JA, et al. The potential health care costs and resource use associated with COVID-19 in the United States. Health Aff (Millwood). 2020;39:927–35.
America's Health Insurance Plans. COVID-19 cost scenario modeling: treatment estimating the cost of COVID-19 treatment for US private insurer providers. 2020. https://www.ahip.org/wp-content/uploads/AHIP-COVID-19-Modeling-Update_Wakely-2020.06.pdf.
Avalere Health: Sloan C, Markward N, Young J, et al. COVID-19 hospitalizations projected to cost up to $17B in US in 2020. 2020. https://avalere.com/insights/covid-19-hospitalizations-projected-to-cost-up-to-17b-in-us-in-2020.
Cision PR Newswire. Fair Health. Total charges for all hospitalized COVID-19 patients may reach up to $1.4 trillion, FAIR Health study finds. 2020. https://www.prnewswire.com/news-releases/total-charges-for-all-hospitalized-covid-19-patients-may-reach-up-to-1-4-trillion-fair-health-study-finds-301029480.html.
Di Fusco M, Shea KM, Lin J, et al. Health outcomes and economic burden of hospitalized COVID-19 patients in the United States. J Med Econ. 2021;24:308–17.
Premier Applied Sciences®. Premier Healthcare Database white paper: data that informs and performs. 2020. https://learn.premierinc.com/white-papers/premierhealthcaredatabase.
Kadri SS, Gundrum J, Warner S, et al. Uptake and accuracy of the diagnosis code for COVID-19 among US hospitalizations. JAMA. 2020;324:2553–4.
Beigel JH, Tomashek KM, Dodd LE, et al. Remdesivir for the treatment of Covid-19—final report. N Engl J Med. 2020;383:1813–26.
Kalil AC, Patterson TF, Mehta AK, et al. Baricitinib plus remdesivir for hospitalized adults with Covid-19. N Engl J Med. 2020;384:795–807.
Rae M, Claxton G, Kurani N, McDermott D, Cox C. Peterson-KFF Health System Tracker; San Francisco, CA: 2020. Potential costs of COVID-19 treatment for people with employer coverage. https://www.healthsystemtracker.org/brief/potential-costs-of-coronavirus-treatment-for-people-with-employer-coverage/.
Lavery AM, Preston LE, Ko JY, et al. Characteristics of hospitalized COVID-19 patients discharged and experiencing same-hospital readmission—United States, March–August 2020. Morb Mortal Wkly Rep. 2020;69:1695–9.
Rosenthal N, Cao Z, Gundrum J, Sianis J, Safo S. Risk factors associated with in-hospital mortality in a US national sample of patients with COVID-19. JAMA Netw Open. 2020;3:e2029058-e.
Roth GA, Emmons-Bell S, Alger HM, et al. Trends in patient characteristics and COVID-19 in-hospital mortality in the united states during the COVID-19 pandemic. JAMA Netw Open. 2021;4(5):e218828-e.
Acknowledgements
Funding
This study was funded by Eli Lilly and Company. The Journal’s Rapid Service Fees were funded by Eli Lilly and Company.
Medical Writing, Editorial, and Other Assistance
Authors would like to acknowledge Siew Hoong Wong-Jacobson, Mingyang Shan, Xian Zhou, Diane Haldane and David R Nelson for their contributions in statistical analyses. Medical writing and editorial support were provided by Santanu Bhadra, PhD, full-time employees of Eli Lilly Services India Private Limited, Bengaluru, India.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole.
Authorship Contributions
Robert L. Ohsfeldt, Casey Kar-Chan Choong, Patrick L Mc Collam, Hamed Abedtash, Kari A. Kelton and Russel Burge all made substantial contributions to conception, interpretation of data, drafting the manuscript, and revising it critically for important intellectual content, and have given their approval for this version of manuscript to be published.
Disclosures
Robert L. Ohsfeldt is a consultant to Medical Decision Modeling Inc. for projects sponsored by various pharmaceutical companies. He received grants or contracts from Texas Dept of Human Health Services, Texas A&M University as co-principal investigator, and Blue Cross/Blue Shield of Texas, Texas A&M University as principal investigator. Casey Kar-Chan Choong, Patrick L Mc Collam, Hamed Abedtash, and Russel Burge are employees and shareholders of Eli Lilly and Company. Kari A. Kelton is an employee of Medical Decision Modeling Inc. which was contracted to perform consulting work for Eli Lilly and Company.
Compliance with Ethics Guidelines
This is an observational study that uses previously collected data and does not impose any form of intervention, and was performed in accordance with the Helsinki Declaration of 1964 and its later amendments. Data have been deidentified to protect subject privacy and to be fully compliant with the US patient confidentiality requirements, including the Health Insurance Portability and Accountability Act of 1996, and did not require institutional review board waiver or approval.
Data Availability
The datasets generated and/or analyzed during the current study are not publicly available due to individual data privacy but may be available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ohsfeldt, R.L., Choong, C.KC., Mc Collam, P.L. et al. Inpatient Hospital Costs for COVID-19 Patients in the United States. Adv Ther 38, 5557–5595 (2021). https://doi.org/10.1007/s12325-021-01887-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-021-01887-4