Abstract
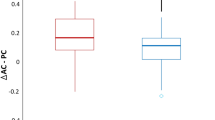
A clinical scale fully dedicated to evaluating ocular motor abnormalities is required for now. We investigated the utility of a recently developed Scale for Ocular motor Disorders in Ataxia (SODA) in patients with multiple system atrophy (MSA). We prospectively assessed SODA in consecutive patients with MSA between August 2021 and August 2023 at the Korea University Medical Center. The results of the clinical exam-based SODA were compared with those measured using video-oculography (VOG-guided SODA). We also compared the findings with other established clinical scales targeting patients with MSA, including the Unified Multiple System Atrophy Rating Scale (UMSARS) I-II, Movement Disorder Society-Unified Parkinson’s Disease Rating Scale motor part (UPDRS-III), Scale for Assessment of Rating of Ataxia (SARA), Composite Autonomic Symptom Score-31 (COMPASS-31), and Composite Autonomic Severity Score (CASS). Twenty patients were enrolled in our study (17 with cerebellar-type MSA and three with Parkinson-type MSA). Scores ranged from 1 to 14 (median [interquartile range (IQR)] = 8 [5−10]). Among the subscales, saccades had a median score of 2.5 (IQR = 1–3), followed by ocular pursuit (1 [0–1]), nystagmus (1 [0–2]), saccadic intrusions (1 [0–1]), vestibulo-ocular reflex (VOR) (0.5 [0–1]), ocular alignment (0 [0–1]), and VOR cancellation (1 [0–1]). The clinical-exam-based SODA (p = 0.020) and VOG-guided SODA (p = 0.034) positively correlated with disease duration. No correlation was found between clinical exam-based SODA and other scales. Skew deviation, gaze-evoked nystagmus, VOR cancellation, and smooth pursuit had the highest precision among the items. Ocular misalignment and spontaneous and positional nystagmus were frequently false positive and were poorly detected with clinical exam-based SODA. Six patients with repeated evaluation exhibited higher scores, along with deterioration documented on other clinical scales. The SODA can reliably predict neurodegeneration as an additional clinical surrogate in MSA.


Similar content being viewed by others
Data Availability
Anonymized data will be shared by request from any qualified investigator.
References
Gai W, Power J, Blumbergs P, Blessing W. Multiple-system atrophy: a new α-synuclein disease? Lancet. 1998;352:547–8.
Koga S, Aoki N, Uitti RJ, Van Gerpen JA, Cheshire WP, Josephs KA, Wszolek ZK, Langston JW, Dickson DW. When DLB, PD, and PSP masquerade as MSA: an autopsy study of 134 patients. Neurology. 2015;85:404–12.
Litvan I, Goetz CG, Jankovic J, Wenning GK, Booth V, Bartko JJ, McKee A, Jellinger K, Lai EC, Brandel J-P. What is the accuracy of the clinical diagnosis of multiple system atrophy? A clinicopathologic study. Arch Neurol. 1997;54:937–44.
Miki Y, Foti SC, Asi YT, Tsushima E, Quinn N, Ling H, Holton JL. Improving diagnostic accuracy of Multiple System Atrophy: a clinicopathological study. Brain. 2019;142:2813–27.
Kim HJ, Stamelou M, Jeon B. Multiple system atrophy-mimicking conditions: diagnostic challenges. Parkinsonism Relat Disord. 2016;22:12–S15.
Wenning GK, Tison F, Seppi K, Sampaio C, Diem A, Yekhlef F, Ghorayeb I, Ory F, Galitzky M, Scaravilli T. Development and validation of the unified Multiple System Atrophy rating scale (UMSARS). Mov Disord. 2004;19:1391–402.
Schmahmann JD, Gardner R, MacMore J, Vangel MG. Development of a brief ataxia rating scale (BARS) based on a modified form of the ICARS. Mov Disord. 2009;24:1820–8.
Shaikh AG, Kim J-S, Froment C, Koo YJ, Dupre N, Hadjivassiliou M, Honnorat J, Kothari S, Mitoma H, Rodrigue X. Scale for Ocular Motor Disorders in Ataxia (SODA): Procedures and Basic Understanding. 347–361. In: Trials for Cerebellar Ataxias: From Cellular Models to Human Therapies. Springer-Verlag: Berlin Heidelberg; 2023.
Shaikh AG, Kim J-S, Froment C, Koo YJ, Dupre N, Hadjivassiliou M, Honnorat J, Kothari S, Mitoma H, Rodrigue X. Scale for Ocular motor Disorders in Ataxia (SODA). J Neurol Sci. 2022;443120472.
Wenning GK, Stankovic I, Vignatelli L, Fanciulli A, Calandra-Buonaura G, Seppi K, Palma JA, Meissner WG, Krismer F, Berg D. The movement disorder society criteria for the diagnosis of Multiple System Atrophy. Mov Disord. 2022;37:1131–48.
Kim JG, Kim SH, Lee SU, Lee CN, Kim BJ, Kim JS, Park KW. Head-impulse tests aid in differentiation of multiple system atrophy from Parkinson’s disease. J Neurol. 2022;269:2972–9.
Kim SH, Lee SU, Cho BH, Cho KH, Yu S, Kim BJ, Kim JS. Analyses of head-impulse tests in patients with posterior circulation stroke and vestibular neuritis. Neurology. 2023;100:e2374–85.
Scheiman M, Wick B. Clinical management of binocular vision: heterophoric, accommodative, and eye movement disorders. 3rd ed. Philadelphia: Lippincott Williams & Wilkins; 2008.
Schmitz-Hübsch T, Du Montcel ST, Baliko L, Berciano J, Boesch S, Depondt C, Giunti P, Globas C, Infante J, Kang JS. Scale for the assessment and rating of ataxia: development of a new clinical scale. Neurology. 2006;66:1717–20.
Goetz CG, Tilley BC, Shaftman SR, Stebbins GT, Fahn S, Martinez-Martin P, Poewe W, Sampaio C, Stern MB, Dodel R. Movement Disorder Society‐sponsored revision of the Unified Parkinson’s Disease Rating Scale (MDS‐UPDRS): scale presentation and clinimetric testing results. Mov Disord. 2008;23:2129–70.
Sletten DM, Suarez GA, Low PA, Mandrekar J, Singer W. COMPASS 31: a refined and abbreviated composite autonomic symptom score. Mayo Clin Proc. 2012;87:1196–201.
Low PA. Composite autonomic scoring scale for laboratory quantification of generalized autonomic failure. Mayo Clin Proc. 1993;68:748–52.
Kim JB, Kim H, Sung JH, Baek SH, Kim BJ. Heart-rate-based machine-learning algorithms for screening orthostatic hypotension. J Clin Neurol. 2020;16:448–54.
Kim JG, Lee JH, Lee SU, Choi JY, Kim BJ, Kim JS. Utricular dysfunction in patients with orthostatic hypotension. Clin Aut Res. 2022;32:431–44.
Sarva H, Shanker VL. Treatment options in degenerative cerebellar ataxia: a systematic review. Mov Didsord Clin Pract. 2014;1:291–8.
Maaß S, Levin J, Höglinger G. Current treatment of multiple system atrophy. Curr Curr Treat Options Neurol. 2016;18:51.
Young AS, Rosengren SM, D’Souza M, Bradshaw AP, Welgampola MS. Nystagmus characteristics of healthy controls. J Vestib Res. 2020;30:345–52.
Martens C, Goplen FK, Nordfalk KF, Aasen T, Nordahl SHG. Prevalence and characteristics of positional nystagmus in normal subjects. Otolaryngol Head Neck Surg. 2016;154:861–7.
Choi JY, Kim JH, Kim HJ, Glasauer S, Kim JS. Central paroxysmal positional nystagmus: characteristics and possible mechanisms. Neurology. 2015;84:2238–46.
Choi JY, Glasauer S, Kim JH, Zee DS, Kim JS. Characteristics and mechanism of apogeotropic central positional nystagmus. Brain. 2018;141:762–75.
Shin JH, Shin DA, Lee CY, Chang HJ, Woo KA, Kim HJ, Lee JC, Jeon B. Inability to suppress head rotation during the saccade test as a clinical biomarker for cognitive dysfunction in Parkinson’s disease. Neurosci Lett. 2023;812:137356.
Funding
This study was supported by the Basic Research Program through the National Research Foundation of Korea (NRF), funded by the MSIT (2022R1A4A1018869).
Author information
Authors and Affiliations
Contributions
Dr. H. Yoon analyzed and interpreted the data and wrote the manuscript.Drs. H. Kwon, E. Park, C.N. Lee, B.J. Kim, J.S. Kim, and K.W. Park analyzed and interpreted the data, and revised the manuscript.Dr. S.U. Lee designed and conceptualized the study, interpreted the data, and revised the manuscript.
Corresponding author
Ethics declarations
Ethical Approval
This study followed the tenets of the Declaration of Helsinki and was performed according to the guidelines of the Institutional Review Board of Korea University Anam Hospital (2021AN0173).
Competing Interests
Drs. H. Yoon, H. Kwon, E. Park, S.U. Lee, C.N. Lee, and K.W. Park report no disclosures. BJ Kim serves as an Editor-in-Chief of the Journal of Clinical Neurology. JS Kim serves as an Associate Editor of Frontiers in Neuro-otology and on the editorial boards of the Journal of Clinical Neurology, Frontiers in Neuro-ophthalmology, Journal of Neuro-ophthalmology, Journal of Vestibular Research, Medicine, and Clinical and Translational Neuroscience.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yoon, H., Kwon, H., Lee, SU. et al. Scale for Ocular Motor Disorders in Ataxia (SODA) in Patients with Multiple System Atrophy. Cerebellum (2023). https://doi.org/10.1007/s12311-023-01653-y
Accepted:
Published:
DOI: https://doi.org/10.1007/s12311-023-01653-y