Abstract
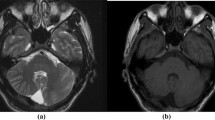
We report on seven patients with a novel neuroimaging finding that involves exclusively the cerebellar gray matter at the bottom of several fissures of both hemispheres but spares the vermis. The abnormal fissures were predominantly located in the lower and lateral parts of the cerebellar hemispheres. The affected cerebellar cortex was hypointense on T1-weighted and hyperintense on T2-weighted and fluid attenuation inversion recovery sequences. In some patients, the involved cerebellar gray matter was mildly thickened and the affected fissures slightly widened. In three of seven patients, the neuroimaging findings were unchanged on follow-up studies up to 6 years. The seven patients had various indications for the brain magnetic resonance imaging studies, and none of them had cerebellar dysfunction. Based on the similarity of the neuroimaging pattern with the cerebral “bottom-of-sulcus dysplasia,” we coined the term “cerebellar bottom-of-fissure dysplasia” to refer to this novel neuroimaging finding. The neuroimaging characteristic as well as the unchanged findings on follow-up favors a stable “developmental” (malformative) nature. The lack of cerebellar dysfunction in the affected patients suggests that cerebellar bottom-of-fissure dysplasia represents most likely an incidental finding that does not require specific diagnostic investigation but allows a reassuring attitude.



Similar content being viewed by others
Abbreviations
- BOFD:
-
Bottom-of-fissure dysplasia
- BOSD:
-
Bottom-of-sulcus dysplasia
- FLAIR:
-
Fluid attenuation inversion recovery
- MRI:
-
Magnetic resonance imaging
References
Barkovich AJ, Millen KJ, Dobyns WB. A developmental and genetic classification for midbrain-hindbrain malformations. Brain. 2009;132:3199–230.
Barth PG, Majoie CB, Caan MW, et al. Pontine tegmental cap dysplasia: a novel brain malformation with a defect in axonal guidance. Brain. 2007;130:2258–66.
Poretti A, Mall V, Smitka M, et al. Macrocerebellum: significance and pathogenic considerations. Cerebellum. 2012;11:1026–36.
Aldinger KA, Mosca SJ, Tetreault M, et al. Mutations in LAMA1 cause cerebellar dysplasia and cysts with and without retinal dystrophy. Am J Hum Genet. 2014;95:227–34.
Poretti A, Hausler M, von Moers A, et al. Ataxia, intellectual disability, and ocular apraxia with cerebellar cysts: a new disease? Cerebellum. 2014;13:79–88.
Hofman PA, Fitt GJ, Harvey AS, Kuzniecky RI, Jackson G. Bottom-of-sulcus dysplasia: imaging features. AJR Am J Roentgenol. 2011;196:881–5.
Harvey AS, Mandelstam SA, Maixner WJ, et al. The surgically remediable syndrome of epilepsy associated with bottom-of-sulcus dysplasia. Neurology. 2015;84:2021–8.
Miller JW, Gonzalez-Martinez J. Epilepsy and the funny sulcus. Neurology. 2015;84:2012–3.
Besson P, Andermann F, Dubeau F, Bernasconi A. Small focal cortical dysplasia lesions are located at the bottom of a deep sulcus. Brain. 2008;131:3246–55.
Wagner J, Weber B, Urbach H, Elger CE, Huppertz HJ. Morphometric MRI analysis improves detection of focal cortical dysplasia type II. Brain. 2011;134:2844–54.
Mellerio C, Labeyrie MA, Chassoux F, et al. 3T MRI improves the detection of transmantle sign in type 2 focal cortical dysplasia. Epilepsia. 2014;55:117–22.
Krsek P, Jahodova A, Maton B, et al. Low-grade focal cortical dysplasia is associated with prenatal and perinatal brain injury. Epilepsia. 2010;51:2440–8.
Blumcke I, Thom M, Aronica E, et al. The clinicopathologic spectrum of focal cortical dysplasias: a consensus classification proposed by an ad hoc Task Force of the ILAE Diagnostic Methods Commission. Epilepsia. 2011;52:158–74.
Blumcke I, Spreafico R. An international consensus classification for focal cortical dysplasias. Lancet Neurol. 2011;10:26–7.
Barkovich AJ, Guerrini R, Kuzniecky RI, Jackson GD, Dobyns WB. A developmental and genetic classification for malformations of cortical development: update 2012. Brain. 2012;135:1348–69.
Wang DD, Deans AE, Barkovich AJ, et al. Transmantle sign in focal cortical dysplasia: a unique radiological entity with excellent prognosis for seizure control. J Neurosurg. 2013;118:337–44.
Doherty D, Chudley AE, Coghlan G, et al. GPSM2 mutations cause the brain malformations and hearing loss in Chudley-McCullough syndrome. Am J Hum Genet. 2012;90:1088–93.
Kau T, Veraguth D, Schiegl H, Scheer I, Boltshauser E. Chudley-McCullough syndrome: case report and review of the neuroimaging spectrum. Neuropediatrics. 2012;43:44–7.
Bahi-Buisson N, Poirier K, Boddaert N, et al. GPR56-related bilateral frontoparietal polymicrogyria: further evidence for an overlap with the cobblestone complex. Brain. 2010;133:3194–209.
Bosemani T, Orman G, Boltshauser E, et al. Congenital abnormalities of the posterior fossa. Radiographics. 2015;35:200–20.
Berger JR, Weaver A, Greenlee J. Neurologic consequences of autoimmune polyglandular syndrome type 1. Neurology. 2008;70:2248–51.
Tabarki B, Al-Shafi S, Al-Shahwan S, et al. Biotin-responsive basal ganglia disease revisited: clinical, radiologic, and genetic findings. Neurology. 2013;80:261–7.
Kevelam SH, Rodenburg RJ, Wolf NI, et al. NUBPL mutations in patients with complex I deficiency and a distinct MRI pattern. Neurology. 2013;80:1577–83.
Te Riele MG, Verrips A. Severe hypomagnesaemia causing reversible cerebellopathy. Cerebellum. 2014;13:659–62.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of Interest
All co-authors do not report conflicts of interest.
Funding
This work was not supported by grants.
Rights and permissions
About this article
Cite this article
Poretti, A., Capone, A., Hackenberg, A. et al. Cerebellar Bottom-of-Fissure Dysplasia—a Novel Cerebellar Gray Matter Neuroimaging Pattern. Cerebellum 15, 705–709 (2016). https://doi.org/10.1007/s12311-015-0736-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12311-015-0736-y