Abstract
Background
Despite a plethora of literature reporting on the use of tranexamic acid (TXA) in total hip arthroplasty (THA), little is available on its effect on post-operative hidden blood loss and even less on its use in the direct anterior approach (DAA), which is gaining popularity.
Materials and methods
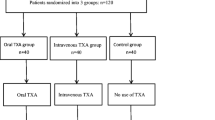
This study was designed as a prospective, double blind, single centre, randomized controlled trial. Sixty patients were allocated to intravenous administration of 1.5 g of TXA just before wound closure while 60 patients were allocated to topical application of 3.0 g of TXA via a subfascial drain at the end of the procedure. Post-operative blood loss was (1) calculated via a well-established formula based on pre- and post-operative Hb levels, patients characteristics and intra-operative blood loss and (2) measured via the amount that collected in the subfascial drain over time.
Results
No statistical significant difference in post-operative blood loss was found, neither when the formula was used (0.55 L [topical] vs 0.67 L [IV]; p = .140) nor when looking at the drain output (0.25 L [topical] vs 0.29 L [IV]; p = .108). No significant difference in secondary outcome measures, such as transfusion of units of packed red blood cells, length of hospital stay or the occurrence of venous thromboembolisms, could be found either.
Conclusions
This study provides detailed insights into the intra- and post-operative blood loss in DAA THA and shows that topical and IV TXA have similar effects on hidden blood loss.
Clinical Trial Number: NCT01940692.
Level of evidence I
Level I—Randomized Controlled Trial.

Similar content being viewed by others
References
Learmonth ID, Young C, Rorabeck C (2007) The operation of the century: total hip replacement. Lancet 370(9597):1508–1519
LROI (2019) Trend (proportion [%] per year) in surgical approach for performing a primary total hip arthroplasty in the Netherlands in 2010–2018: Dutch Orthopaedic Society
Hallert O, Li Y, Brismar H, Lindgren U (2012) The direct anterior approach: initial experience of a minimally invasive technique for total hip arthroplasty. J Orthop Surg Res 7:17
de Steiger RN, Lorimer M, Solomon M (2015) What is the learning curve for the anterior approach for total hip arthroplasty? Clin Orthop Relat Res 473(12):3860–3866
Meermans G, Konan S, Das R, Volpin A, Haddad FS (2017) The direct anterior approach in total hip arthroplasty: a systematic review of the literature. Bone Joint J 99-B(6):732–740
Martinez V, Monsaingeon-Lion A, Cherif K, Judet T, Chauvin M, Fletcher D (2007) Transfusion strategy for primary knee and hip arthroplasty: impact of an algorithm to lower transfusion rates and hospital costs. Br J Anaesth 99(6):794–800
Browne JA, Adib F, Brown TE, Novicoff WM (2013) Transfusion rates are increasing following total hip arthroplasty: risk factors and outcomes. J Arthroplasty 28(8 Suppl):34–37
Rosencher N, Kerkkamp HE, Macheras G, Munuera LM, Menichella G, Barton DM et al (2003) Orthopedic Surgery Transfusion Hemoglobin European Overview (OSTHEO) study: blood management in elective knee and hip arthroplasty in Europe. Transfusion 43(4):459–469
Klein HG (2010) How safe is blood, really? Biologicals 38(1):100–104
Frisch NB, Wessell NM, Charters MA, Yu S, Jeffries JJ, Silverton CD (2014) Predictors and complications of blood transfusion in total hip and knee arthroplasty. J Arthroplasty 29(9 Suppl):189–192
Gandhi R, Evans HM, Mahomed SR, Mahomed NN (2013) Tranexamic acid and the reduction of blood loss in total knee and hip arthroplasty: a meta-analysis. BMC Res Notes 6:184
Zhao H, Xiang M, Xia Y, Shi X, Pei FX, Kang P (2018) Efficacy of oral tranexamic acid on blood loss in primary total hip arthroplasty using a direct anterior approach: a prospective randomized controlled trial. Int Orthop 42(11):2535–2542
Fraval A, Duncan S, Murray T, Duggan J, Tirosh O, Tran P (2019) OBTAIN E: outcome benefits of tranexamic acid in hip arthroplasty with enoxaparin: a randomised double-blinded controlled trial. Hip Int 29(3):239–244
North WT, Mehran N, Davis JJ, Silverton CD, Weir RM, Laker MW (2016) Topical vs intravenous tranexamic acid in primary total hip arthroplasty: a double-blind. Randomized Controlled Trial. J Arthroplasty 31(4):928–929
Sun X, Dong Q, Zhang YG (2016) Intravenous versus topical tranexamic acid in primary total hip replacement: a systemic review and meta-analysis. Int J Surg 32:10–18
Zhang P, Liang Y, Chen P, Fang Y, He J, Wang J (2016) Intravenous versus topical tranexamic acid in primary total hip replacement: a meta-analysis. Med (Baltimore) 95(50):e5573
Xie J, Hu Q, Huang Q, Ma J, Lei Y, Pei F (2017) Comparison of intravenous versus topical tranexamic acid in primary total hip and knee arthroplasty: an updated meta-analysis. Thromb Res 153:28–36
Luo ZY, Wang HY, Wang D, Zhou K, Pei FX, Zhou ZK (2018) Oral vs intravenous vs topical tranexamic acid in primary hip arthroplasty: a prospective, randomized, double-blind. Controlled Study. J Arthroplasty 33(3):786–793
Perez-Jimeno N, Munoz M, Mateo J, Mayoral AP, Herrera A (2018) Efficacy of topical tranexamic acid within a blood-saving programme for primary total hip arthroplasty: a pragmatic, open-label randomised study. Blood Transfus 16(6):490–497
Clave A, Gerard R, Lacroix J, Baynat C, Danguy des Deserts M, Gatineau F et al (2019) A randomized, double-blind, placebo-controlled trial on the efficacy of tranexamic acid combined with rivaroxaban thromboprophylaxis in reducing blood loss after primary cementless total hip arthroplasty. Bone Joint J 101B(2):207–212
Sabbag OD, Abdel MP, Amundson AW, Larson DR, Pagnano MW (2017) Tranexamic acid was safe in arthroplasty patients with a history of venous thromboembolism: a matched outcome study. J Arthroplasty 32(9S):S246–S250
Dastrup A, Pottegard A, Hallas J, Overgaard S (2018) Perioperative tranexamic acid treatment and risk of cardiovascular events or death after total hip arthroplasty: a population-based cohort study from national danish databases. J Bone Joint Surg Am 100(20):1742–1749
Zhou KD, Wang HY, Wang Y, Liu ZH, He C, Feng JM (2018) Is topical or intravenous tranexamic acid preferred in total hip arthroplasty? A randomized, controlled, noninferiority clinical trial. PLoS ONE 13(10):e0204551
Van Elst CVJ, Simon JP, Corten Kristoff. The effect of topical application of tranexamic acid in total hip arthroplasty conducted through the direct anterior approach [Poster presentation EFORT]. EFORT13-3703
Suarez JC, McNamara CA, Barksdale LC, Calvo C, Szubski CR, Patel PD (2016) Closed suction drainage has no benefits in anterior hip arthroplasty: a prospective. Randomized Trial. J Arthroplasty 31(9):1954–1958
Imai N, Dohmae Y, Suda K, Miyasaka D, Ito T, Endo N (2012) Tranexamic acid for reduction of blood loss during total hip arthroplasty. J Arthroplasty 27(10):1838–1843
Wei W, Wei B (2014) Comparison of topical and intravenous tranexamic acid on blood loss and transfusion rates in total hip arthroplasty. J Arthroplasty 29(11):2113–2116
Konig G, Hamlin BR, Waters JH (2013) Topical tranexamic acid reduces blood loss and transfusion rates in total hip and total knee arthroplasty. J Arthroplasty 28(9):1473–1476
Yue C, Kang P, Yang P, Xie J, Pei F (2014) Topical application of tranexamic acid in primary total hip arthroplasty: a randomized double-blind controlled trial. J Arthroplasty 29(12):2452–2456
Nadler SB, Hidalgo JH, Bloch T (1962) Prediction of blood volume in normal human adults. Surgery 51(2):224–232
Good L, Peterson E, Lisander B (2003) Tranexamic acid decreases external blood loss but not hidden blood loss in total knee replacement. Br J Anaesth 90(5):596–599
Wong J, Abrishami A, El Beheiry H, Mahomed NN, Roderick Davey J, Gandhi R et al (2010) Topical application of tranexamic acid reduces postoperative blood loss in total knee arthroplasty: a randomized, controlled trial. J Bone Joint Surg Am 92(15):2503–2513
Carling MS, Jeppsson A, Eriksson BI, Brisby H (2015) Transfusions and blood loss in total hip and knee arthroplasty: a prospective observational study. J Orthop Surg Res 10:48
Guild GN 3rd, Runner RP, Castilleja GM, Smith MJ, Vu CL (2017) Efficacy of hybrid plasma scalpel in reducing blood loss and transfusions in direct anterior total hip arthroplasty. J Arthroplasty 32(2):458–462
Li JF, Li H, Zhao H, Wang J, Liu S, Song Y et al (2017) Combined use of intravenous and topical versus intravenous tranexamic acid in primary total knee and hip arthroplasty: a meta-analysis of randomised controlled trials. J Orthop Surg Res 12(1):22
Lopez-Picado A, Albinarrate A, Barrachina B (2017) Determination of perioperative blood loss: accuracy or approximation? Anesth Analg 125(1):280–286
Acknowledgements
Brecht Jacobs is acknowledged for help with collecting the data.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Authorship credit was given in accordance with the standard proposed by the International Committee of Medical Journal Editors.
Corresponding author
Ethics declarations
Conflict of interest
All authors report no proprietary or commercial interest in any product mentioned or concept discussed in this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Vles, G.F., Corten, K., Driesen, R. et al. Hidden blood loss in direct anterior total hip arthroplasty: a prospective, double blind, randomized controlled trial on topical versus intravenous tranexamic acid. Musculoskelet Surg 105, 267–273 (2021). https://doi.org/10.1007/s12306-020-00652-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12306-020-00652-0