Abstract
The bloodstream infections (BSIs) are among the most common infectious complications after hematopoietic stem-cell transplantation (HSCT), often associated with high mortality rates. The aim of this study was to evaluate the incidence, risk factors and outcome of BSIs in HSCT recipients from the Transplantation Center of the University Hospital in Varna, Bulgaria during the period January 2019–December 2021. The role of patient- and transplantation-related variables was studied as potential risk factors for BSIs and survival after HSCT. Seventy-four patients were included in the study. The cumulative incidence of BSIs was 35%. The mean period of BSI onset after HSCT was 8 days. The Gram-positive bacteria were more commonly isolated as causative agents (52.3%). The mortality rate 30 days after the diagnosis of BSI was 23%. Fecal colonization with multidrug-resistant (MDR) bacteria (p = 0.005) and pre-transplant BSI (p = 0.05) were associated with significantly increased risk for post-HSCT BSIs. The overall 4-month survival was 86.5%. A statistical significance was found between the type of the underlying disease (acute leukemia and lymphoma, p = 0.043), previous HSCT (p = 0.001) and 4-month survival. This study confirms that the fecal colonization with MDR bacteria before transplantation and pre-transplant BSIs are independent risk factors for the occurrence of BSI in the early period after HSCT. Pre- and posttransplant monitoring of the patient fecal colonization status with MDR organisms, could contribute considerably to the prevention and successful management of the infectious complications in patients after HSCT.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The hematopoietic stem-cell transplantation (HSCT) is an effective treatment method for different malignancies, syndromes with bone marrow failure, as well as immunodeficiency conditions in children, adolescents and adult individuals. More than 50,000 HSCTs per year are carried out globally [1]. The development of transplant strategies and the advancement of the supportive care led to an improvement in the patient outcome after transplantation [2]. However, different infectious complications constantly accompany HSCT. The bloodstream infections (BSIs) are a major cause of morbidity and mortality after HSCT [3].
The aim of this study is to evaluate the incidence, risk factors, outcome of bloodstream infections and 4-month survival of HSCT recipients from the Transplantation Center of the University Hospital of Medical University, Varna, Bulgaria during the period January 2019–December 2021.
Materials and Methods
This is a prospective epidemiological and microbiological study performed in the Transplantation Center at the University Hospital of Medical University, Varna, Bulgaria between January 2019 and December 2021. All consecutive patients who underwent HSCT (autologous and allogeneic) during this period were included in the study. The study was approved by the Ethical Committee of Varna Medical University (№ 92/02.04.2020) and informed consent was obtained from the patients.
Data Collection
For each enrolled patient information regarding the following variables was collected: demographic information (sex, age), underlying diseases, clinical findings (mucositis, graft vs host disease, GVHD), patient’s history (previous HSCT, BSI before HSCT), diagnostic test results (fecal screening, positive blood cultures, Cytomegalovirus status, neutropenia for more than 7 days) and transplantation-related data (type of HSCT, donor type, stem-cell source, time to neutrophil and platelet engraftment, use of antithymocyte globulin). Demographics and patient characteristics at HSCT are shown in Table 1.
Microbiological Investigation
In case of suspected infectious complication (chills, high fever, elevated C - reactive protein), blood samples (simultaneously from the central venous catheter and a peripheral vein) were collected and further incubated in Bactec FX40 (BD, USA) for 5 days at 35 °C or for 14 days when fungemia was suspected. A single positive blood culture was considered significant when bacteria or fungi different from the resident skin flora (Corynebacterium spp., Bacillus spp. and Coagulase-negative staphylococci) were detected. In case of isolation of normal skin microbial flora, two or more consecutive blood cultures with the same pathogen were interpreted as clinically significant.
As part of the routine pre- and posttransplant monitoring of the patient colonization status, all patients were screened for fecal colonization by 3rd generation cephalosporin- and carbapenem-resistant representatives of order Enterobacterales and multidrug-resistant (MDR) glucose-nonfermenting Gram-negative bacteria and vancomycin-resistant enterococci by testing rectal swab samples. All patients received antimicrobial prophylaxis in the pre-engraftment period with piperacillin/tazobactam and amikacin or trimethoprim/sulfamethoxazole and acyclovir.
Statistical Analysis
Data for categorical variables were summarized as frequencies and percentages, and for continuous variables as the median and interquartile range. Cumulative incidence of BSIs was calculated for the total studied cohort and by HSCT type with 95% confidence intervals (CI). The probability of 4-month survival after HSCT was calculated using Kaplan-Meier estimates. For univariate analysis of predictors of BSI, Cox proportional hazards regression was used. All significant variables in the univariate analysis were included in the multivariate analysis. Two-sided p values ≤ 0.05 were considered statistically significant. Statistical analyses were performed using IBM SPSS ver 21.
Results
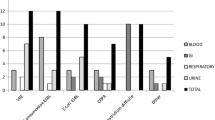
A total of seventy-four patients who underwent HSCT between January 2019 and December 2021 at the Transplantation Center of Varna University Hospital, Bulgaria were included in the study. The average days with neutropenia in the autologous HSCT group was 10.3 (8–15 days) and 15.5 days (8–29) in the allogeneic one. The incidence of BSI among patients who had an autologous HSCT was 30.6% (n = 15) (95% CI 18.2–45.4) and among the patients with allogeneic HSCT was 44% (n = 11) (95% CI 24.2–65.1). The mean period of onset of BSIs after HSCT was 8 days (SD ± 20.1). During the studied period, a total of 35 episodes of BSIs were identified in 26 of all 74 patients who underwent HSCT. The cumulative incidence of BSI was 35% (95% CI 24.4–47.1) in the studied cohort for the studied period. Bacteremia was documented as a single episode in 15 patients (58%). Seven and 2 patients were presented with two and three episodes, respectively. Four different bacteremia episodes with different causative agents and diagnosed more than 5 days apart were detected in only one patient. The Gram-positive bacteria were more commonly isolated as causative agents of BSIs (52.3%), mainly presented by Coagulase-negative staphylococci (dominated by Staphylococcus epidermidis), followed by Gram-negative bacteria (45.2%) from Enterobacteriaceae family and glucose-nonfermenting Gram-negative bacteria (dominated by Escherichia coli), and fungi (2.4%, Candida krusei). All Coagulase-negative staphylococci were methicillin-resistant. In the group of Gram-negative bacteria 15.8% were resistant to 3rd generation cephalosporins and 5.3% were carbapenem-resistant. The rest of the microorganisms demonstrated the wild-type susceptibility profiles.
Bloodstream infections before day 30 after HSCT occurred in 25 (96.2%) оf the 26 patients with bacteremia and after day 30—in one patient (3.8%) with autologous HSCT. Pre-engraftment infections were diagnosed in 24 patients (92.3%), presented with 29 episodes of BSI. In this study only a single episode of fungemia was documented. It was diagnosed on day 6 after allogeneic HSCT in a 61-year-old male with myelodysplastic syndrome and matched unrelated donor used as a stem-cell donor. The variables associated with significantly increased risk for post-transplant bacteremia were fecal colonization with MDR bacteria (p = 0.005) and pre-transplant BSI (p = 0.05).
The mortality rate 30 days after diagnosis of bacteremia/fungemia was 23% (6 of 26 patients). In three (50%) of the six patients who died before day 30, the infection was the primary cause of death. A statistical significance was not found between all evaluated variables and the survival 30 days after BSI (p > 0.05).
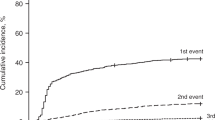
The overall 4-month survival after transplantation was 86.5%. A statistically significant difference in the survival rates between auto- and allo-HSCT recipients was found (p < 0.001) – 98% and 64% for autologous and allogeneic HSCT, respectively. In addition, regarding the average survival after transplantation, the autologous HSCT patients have much longer survival (206.8 days, SD ± 95) than allogeneic HSCT recipients (63.2 days, SD ± 48) (p = 0.002). A statistically significant association was also found between the type of the underlying disease and 4-month survival (p = 0.043). We documented 100% survival rate at 4 months after transplantation for patients with multiple myeloma, aplastic anemia, multiple sclerosis and germ cell testicular carcinoma. Previous transplantation (p = 0.001) and type of the underlying disease (acute leukemia and lymphoma) (p = 0.043) were factors independently associated with increased mortality rate.
Discussion
The HSCT recipients are prone to infectious complications caused by various microorganisms. The reported incidence of these complications varies between 22.8% and 38.3%, respectively [4]. BSIs are among the most common infectious complications in HSCT recipients, mainly during the early stages of the transplantation and BSI incidence ranges between 13.6% and 38.9% [5]. Тhe development of BSI is identified as an essential risk factor for mortality early after HSCT [6]. Major risk factors for BSIs after HSCT are the absolute neutropenia, mucositis and the presence of a central venous catheter (CVC). The type of underlying disease, severe form of GVHD and the corticosteroid treatment are considered as additional factors, contributing to the occurrence of this infectious complication [7].
This prospective study conducted during the period 2019–2021 aimed to identify and evaluate the risk for bloodstream infections, the factors associated with increased risk for BSI incidence after the transplantation and their impact on the patient outcome.
During the 3-year study period, 35% of the patients developed at least one episode of BSI, with the average BSI period being approximately 8 days after HSCT. These results comply with the data reported by other researchers. Ferreira et al. reported an average period of 8 days after HSCT of BSI among 232 patients [8]. Similarly, Akinboyo, Youssef and Ge reported 15.5 and 4.5 days, respectively [3, 7, 9].
In the current study, the cumulative incidence of BSIs after auto- and allo-HSCT was 30.6% and 44%, respectively. Closer to these findings have been reported by Ferreira et al. − 25.4% [8]. In contrast, in a large-scale Italian study collecting data from 54 transplant centers for more than 2500 HSCTs, a cumulative bloodstream infection rate of 9% for auto-HSCT and 17.3% for allo-HSCT was documented [10]. The reported incidence in the study of Dandoy et al. was 21% [2].
In our study а single-factor and multiple regression analyses were used to assess the role of potential risk factors for the development of bloodstream infection after HSCT. Fecal colonization with MDR organisms and a pre-transplant episode of BSI were identified as independent risk factors for pre-engraftment infection. Similar findings have been reported by other authors too. Youssef et al. in a study conducted in Egypt among pediatric patients, who underwent HSCT between 2013 and 2017, found a statistically significant relation between the occurrence of bloodstream infection after HSCT and an episode before the transplantation [7]. Girmenia et al. reported statistical significance between colonization with MDR bacteria and occurrence of BSI both in autologous and allogeneic transplant patients [10]. These data are also supported by a study conducted in Brazil, which identifies intestinal colonization with bacteria demonstrating multidrug resistance as a risk factor for BSI occurrence [8].
In our study, the mortality rate 4 months after transplantation was 36% for allo-HSCT and 2% for auto-HSCT. The BSIs were identified as the primary cause for death in the first month after transplantation in 50% of the patients. Allogeneic HSCT (p < 0.001), previous HSCT (p = 0.001), and type of underlying disease (acute leukemia and lymphoma, p = 0.043) were confirmed as factors associated with poor outcome and prognosis. A large Italian Prospective Multicenter Survey on epidemiology of pre-engraftment BSIs in auto- and allo-HSCT recipients from 54 transplant centers reported 13.5% and 3% mortality rate for allo-HSCT and auto-HSCT, respectively. The acute leukemia, previous transplantation, prolonged neutropenia, a transplant from a HLA-mismatched donor and no antibacterial prophylaxis were reported as factors with negative impact on the patient’s survival [10].
Limitations
Our study had the following limitations: inclusion and follow-up of patients only from a single transplant center; relatively small number of the studied patients; the COVID-19 pandemic negatively impacted the patient hospitalization and the conduction of HSCT.
Conclusion
To the best of our knowledge this is the first study in Bulgaria that identifies and evaluates the incidence, risk factors and outcome of BSIs in patients who underwent HSCT. Our findings confirm that the fecal colonization with MDR bacteria before transplantation and pre-transplant BSIs are independent risk factors for the occurrence of BSI in the early period after HSCT. The allogeneic type of transplantation, acute leukemia and lymphoma, and previous transplantation are factors significantly associated with poor outcome. The results from this study demonstrate that monitoring of some of the most important risk factors for BSIs such as the fecal colonization with MDR organisms, could contribute considerably to the successful management of the infectious complications in patients after HSCT.
References
World Health Organization (WHO) (2018) Haematopoietic stem cell transplantation HSCtx. WHO, Geneva
Dandoy CE, Kim S, Chen M et al (2020) Incidence, risk factors, and outcomes of patients who develop mucosal barrier injury-laboratory confirmed bloodstream infections in the first 100 days after allogeneic hematopoietic stem cell transplant. JAMA Netw Open 3(1):e1918668. https://doi.org/10.1001/jamanetworkopen.2019.18668
Ge J, Yang T, Zhang L et al (2018) The incidence, risk factors and outcomes of early bloodstream infection in patients with malignant hematologic disease after unrelated cord blood transplantation: a retrospective study. BMC Infect Dis 18(1):654. https://doi.org/10.1186/s12879-018-3575-x
Styczynski J, Czyzewski K, Wysocki M et al (2016) Increased risk of infections and infection-related mortality in children undergoing haematopoietic stem cell transplantation compared to conventional anticancer therapy: a multicentre nationwide study. Clin Microbiol Infect 22(2):179.e1-179.e10. https://doi.org/10.1016/j.cmi.2015.10.017
Cao W, Zhang J, Bian Z et al (2022) Active screening of intestinal colonization of carbapenem-resistant Enterobacteriaceae for subsequent bloodstream infection in allogeneic hematopoietic stem cell transplantation. Infect Drug Resist 15:5993–6006. https://doi.org/10.2147/idr.s387615
Cao W, Guan L, Li X et al (2021) Clinical analysis of bloodstream infections during agranulocytosis after allogeneic hematopoietic stem cell transplantation. Infect Drug Resist 14:185–192. https://doi.org/10.2147/IDR.S280869
Youssef A, Hafez H, Madney Y et al (2020) Incidence, risk factors, and outcome of blood stream infections during the first 100 days post-pediatric allogeneic and autologous hematopoietic stem cell transplantations. Pediatr Transplant 24(1):e13610. https://doi.org/10.1111/petr.13610
Ferreira AM, Moreira F, Guimaraes T et al (2018) Epidemiology, risk factors and outcomes of multi-drug-resistant bloodstream infections in haematopoietic stem cell transplant recipients: importance of previous gut colonization. J Hosp Infect 100(1):83–91. https://doi.org/10.1016/j.jhin.2018.03.004
Akinboyo IC, Young RR, Spees LP et al (2020) Microbiology and risk factors for hospital-associated bloodstream infections among pediatric hematopoietic stem cell transplant recipients. Open Forum Infect Dis 7(4):ofaa03. https://doi.org/10.1093/ofid/ofaa093
Girmenia C, Bertaina A, Piciocchi A et al (2017) Incidence, risk factors and outcome of pre-engraftment Gram-negative bacteremia after allogeneic and autologous hematopoietic stem cell transplantation: an Italian prospective multicenter survey. Clin Infect Dis 65(11):1884–1896. https://doi.org/10.1093/cid/cix690
Acknowledgements
Financial support by Medical University of Varna (19019/2019).
Funding
This study was supported by Medical University of Varna, Bulgaria, grant No: 19019/2019.
Author information
Authors and Affiliations
Contributions
Conceptualization: [Denis Niyazi], [Temenuga Stoeva], [Klara Dokova]; Methodology: [Denis Niyazi], [Temenuga Stoeva], [Ilina Micheva]; Formal analysis and investigation: [Klara Dokova]; Writing—original draft preparation: [Denis Niyazi]; Writing—review and editing: [Temenuga Stoeva]; Funding acquisition: [Denis Niyazi], [Temenuga Stoeva]; Resources: [Ilina Micheva]; Supervision: [Temenuga Stoeva].
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Medical University of Varna (02.04.2020/No. 92).
Informed Consent
Obtained from the included patients in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Niyazi, D., Micheva, I., Dokova, K. et al. Incidence, Risk Factors and Outcome of Bloodstream Infections in Patients After Hematopoietic Stem-Cell Transplantation: A Single Center Study. Indian J Hematol Blood Transfus 39, 610–614 (2023). https://doi.org/10.1007/s12288-023-01645-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12288-023-01645-2