Abstract
Antibody–drug conjugates (ADCs) are an emerging class of anticancer therapy that combines the specificity and long circulation half-life of monoclonal antibodies with the cytotoxic potency of the payload connected through a chemical linker. The optimal management of toxicities is crucial for improving quality of life in patients undergoing ADCs and for avoiding improper dose reductions or discontinuations. This article focuses on the characteristics and management of nausea and vomiting (NV) induced by three ADCs: trastuzumab deruxtecan (T-DXd), sacituzumab govitecan (SG), and datopotamab deruxtecan (Dato-DXd). We summarize the proposed mechanism of NV, clinical study data on NV, and recommendations from clinical guidelines. We also discuss three prospective studies evaluating prophylactic antiemetic therapy in patients receiving T-DXd, along with future perspectives.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Antibody‒drug conjugates (ADCs) have revolutionized cancer treatment by providing a more targeted approach to delivering chemotherapy. ADCs are designed to combine the specificity and long circulation half-life of monoclonal antibodies with the cytotoxic potency of the payload connected through a chemical linker [1]. The antibody in the ADC specifically binds to a target antigen on the surface of cancer cells, allowing the attached cytotoxic drug to be delivered directly to the tumor [1]. This precision minimizes the exposure of healthy cells to toxic agents, thereby reducing off-target side effects; however, patients receiving ADC treatment experience various side effects [2,3,4,5].
Nausea and vomiting (NV) are common side effects associated with trastuzumab deruxtecan (T-DXd), sacituzumab govitecan (SG), and datopotamab deruxtecan (Dato-DXd) [2,3,4,5]. Clinicians need to understand the symptom characteristics of NV induced by these ADCs and manage these symptoms effectively because NV can induce medical complications and distress and impair the quality of life of patients [6].
The purpose of this narrative review is to summarize the characteristics of NV induced by these ADCs and to outline strategies for their prevention and management.
Pathophysiology of CINV
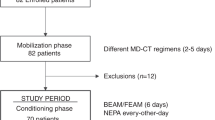
Although the mechanism of NV induced by ADCs has not been fully described, cytotoxic payloads are suspected to cause NV in a manner similar to that of cytotoxic chemotherapeutic drugs (Fig. 1).
Central and peripheral mechanisms of CINV. The pathways by which antineoplastic agents, including antibody–drug conjugates, may produce an emetic response are shown. VC vomiting center, CTZ chemoreceptor trigger zone, EC cells enterochromaffin cells, NK1R neurokinin 1 receptor, D2R dopamine D2 receptor, 5-HT3 R serotonin type 3 receptor
The emetic response involves multiple organs and neurotransmitters, with two main pathways playing key roles: a peripheral pathway and a central pathway [7, 8]. The peripheral pathway, which is predominantly involved in the acute phase of emesis, begins with the release of serotonin from enterochromaffin cells in the gastrointestinal tract in response to chemotherapy-induced damage. Serotonin activates 5-hydroxytryptamine type 3 receptors (5-HT3 R) on vagal afferent nerves, which transmit the stimulus to the nucleus tractus solitarius (NTS) and dorsal motor nucleus of the vagus (DMNV), triggering the emetic response [7,8,9]. The central pathway is predominantly involved in the delayed phase of emesis. The chemoreceptor trigger zone (CTZ), also known as the area postrema, is located in the medulla oblongata at the base of the fourth ventricle, outside the blood‒brain barrier. This location allows it to be more susceptible to circulating substances, such as cytotoxic agents. When the CTZ is activated, it releases neurotransmitters such as serotonin, dopamine, and substance P. These neurotransmitters then stimulate the NTS and the DMNV through serotonin, dopamine, and neurokinin 1 (NK1) receptors [7, 8]. In addition, other pathways, such as the limbic system, vestibular system, and cerebral cortex, can stimulate emesis under conditions such as pain, depression, vertigo, motion sickness, or anticipatory NV. However, the neurotransmitters involved in these pathways are less well understood [10].
The mechanism of nausea is more complex than that of vomiting. The sensation of nausea is thought to arise from the activation of cortical structures involved in conscious perception [9]. Controlling nausea is usually more difficult than controlling vomiting, even when treatment with an NK1 receptor antagonist (NK1RA) or 5-HT3 receptor antagonist (5-HT3 RA) is administered [9, 11].
NV caused by T-DXd can persist for more than 120 h. However, it remains unclear whether this prolonged NV is solely due to the drug’s long half-life (approximately 6 days) or if other factors are involved [12]. T-DXd has demonstrated efficacy in treating brain metastases, suggesting that it penetrates the blood–brain barrier [13]. The potential direct effects of intracranial T-DXd on NV are yet to be fully understood, and it is anticipated that further investigations through basic and translational research will shed light on these mechanisms.
Risk factors for NV
The risk of NV during chemotherapy varies with clinical factors, including the drug type and host-related variables. Chemotherapies are categorized into four risk groups according to the incidence of emesis without the use of antiemetic prophylaxis: high, moderate, low, and minimal risk [14,15,16,17]. Vomiting, rather than nausea, is used as the indicator for the appropriate category.
Previously reported risk factors for chemotherapy-induced nausea and vomiting (CINV) include younger age, female sex, a history of CINV, motion sickness, morning sickness during pregnancy, little or no alcohol use, nonsmoking, and anxiety and/or high pretreatment expectations of nausea and/or vomiting [18, 19]. There is no data to determine whether these are risk factors for ADC-induced NV.
Trastuzumab deruxtecan
T-DXd is an ADC consisting of a humanized, anti-HER2 IgG1 monoclonal antibody that is covalently linked to a topoisomerase I inhibitor payload via a cleavable tetrapeptide-based linker. The drug-to-antibody ratio (DAR) of T-DXd is 8. This high DAR allows delivery of a high concentration of the cytotoxic payload DXd to the target cells [20].
Approximately 70% of patients receiving T-DXd treatment were found to experience nausea of all grades, and approximately 40% experienced vomiting of all grades in DESTINY clinical studies (Table 1) [21]. Recent clinical trials have shown only a slight decrease in frequency. The incidence of NV is highest in the first cycle and decreases in subsequent cycles. Most patients experienced grade 1 or 2 NV. Grade 3 nausea occurred in 5.8%, Grade 3 vomiting occurred in 2.4%, and Grade 4 vomiting occurred in 0.2% of the patients who received T-DXd according to the pooled analysis of the DESTINY clinical studies [21]. In the DESTINY-Breast04 and DESTINY-Breast06 studies, the time to definitive deterioration of the NV subscale was consistently shorter in the T-DXd group than in the control group [22, 23]. Although the protocols of DESTINY clinical studies have recommended the use of prophylactic antiemetic therapy with at least two agents for T-DXd treatment since 2020, this is not mandatory [2, 3].
The emetogenic risk of T-DXd and the recommended antiemetic therapy are inconsistent across clinical guidelines. The MASCC and ESMO guidelines classify T-DXd at the high end of the moderate-risk category, similar to carboplatin [15]. The National Comprehensive Cancer Network (NCCN) guidelines recently upgraded the emetogenic risk of T-DXd from moderate to high [14]. This reclassification was based on the clinical experience of NCCN panel members and retrospective institutional data showing that some patients, who initially received standard prophylaxis for moderately emetogenic treatments, required the addition of an NK1 receptor antagonist in subsequent cycles owing to poor CINV control [14]. In other words, this reclassification is not based on data from prospective studies or large cohort studies. ASCO continues to classify T-DXd as moderate risk [16]. The Japan Society of Clinical Oncology (JSCO) guidelines classify T-DXd as the high end of the moderate-risk category. Because the classification of emetogenic risk varies across guidelines, the recommended antiemetic therapies range from two-drug regimens to four-drug regimens (Table 2).
Three prospective clinical studies evaluated antiemetic therapy for patients receiving T-DXd treatment (Table 3). The EN-hance study was a multicenter randomized open-label study in patients with HER2-positive gastric cancer undergoing the first cycle of T-DXd [24]. The dose of T-DXd used was 6.4 mg/kg, which was administered intravenously on day 1 of a triweekly cycle; this dose differs from the standard dose of 5.4 mg/kg used for other cancers. The patients (n = 60) were randomized to a doublet regimen (dexamethasone and palonosetron) or a triplet regimen (aprepitant in addition to the doublet regimen). The complete response rate, defined as no vomiting and no rescue medication use, during the overall period (days 1–21) was 37.9% in the triplet regimen group and 41.4% in the doublet regimen group, which did not meet the prespecified antiemetic CR rate (≥ 18 of 29 patients). The median time for the first emetic event or nausea was approximately 3 days, with no difference between the two regimens. Iihara et al. conducted a multicenter randomized open-label exploratory study in patients with breast cancer receiving T-DXd [25]. The patients (n = 40) were randomized to a doublet regimen (dexamethasone and granisetron) or a triplet regimen (aprepitant in addition to the doublet regimen). The CR rates during the overall phase (0–120 h) were 36.8% in the doublet regimen group and 70.0% in the triplet regimen group (odds ratio [OR]: 0.1334; 95% confidence interval [CI] 0.0232–0.7672; p = 0.0190), with a difference of 33.2%. The CR rates during the extended-overall phase (0–168 h) were 31.6% in the doublet regimen group and 70.0% in the triplet regimen group (OR: 0.1073; 95% CI 0.0185–0.6239; p = 0.0087), with a difference of 38.4%. These two studies, which compared the efficacy of adding an NK1RA to 5-HT3 RA and dexamethasone in different populations with relatively small sample sizes, yielded inconsistent results. Notably, both studies were open-label and utilized patient-reported outcomes to assess NV. The ERICA study by Sakai et al. was a multicenter randomized, double-blind, placebo-controlled study in patients with HER2-positive or HER2-low breast cancer who were undergoing the first cycle of T-DXd [26]. This study focused on persistent NV induced by T-DXd treatment and utilized patient-reported outcomes to assess NV. Patients (n = 168) were randomized to olanzapine 5 mg or placebo once daily from days 1–6 in addition to 5-HT3 RA and dexamethasone (6.6 mg intravenously or 8 mg orally on day 1). The CR rate in the delayed phase (24–120 h) was 70.0% in the olanzapine group and 56.1% in the placebo group, with a difference of 13.9% and a two-sided 60% CI of 6.9–20.7 (one-sided p = 0.047), indicating that the primary endpoint was met. The CR rate in the persistent phase (120–504 h) was also higher in the olanzapine group than in the placebo group (64.9% vs. 44.4%, difference 19.4%, 95% CI 2.4–35.3). The daily CR rate and daily no-nausea rate were higher in the olanzapine group than in the placebo group throughout the 21-day observational period. The adverse events were similar to those previously reported for olanzapine, and no new safety signals were identified in either group. The addition of olanzapine appeared to be effective in preventing NV in patients receiving T-DXd. The results revealed that patients who underwent T-DXd treatment experienced persistent NV during the 21-day cycle. However, the study left unresolved questions regarding the use of olanzapine vs. NK1RA, as well as the optimal dosage of olanzapine and duration of treatment.
Sacituzumab govitecan
Sacituzumab govitecan (SG) is composed of a humanized trophoblast cell surface antigen 2 (TROP2)-directed monoclonal antibody conjugated to a topoisomerase I inhibitor drug (SN-38) via a hydrolysable linker [34]. SN-38 is an activated form of irinotecan, and the DAR of SG is 7.6 [35]. The frequencies of NV in patients receiving SG were approximately 55% and 20%, and the frequencies of grade ≥ 3 NV were low (Table 4) [4, 36]. The median time to first-onset NV was 8 and 24.5 days after the initiation of SG treatment in the ASCENT study [37]. The protocol of ASCENT recommends prophylactic antiemetic therapy with 5-HT3 RA [4]. However, premedication or concomitant medication for NV was reported to be used in 86% of the SG group [37]. The TROPiCS-02 protocol states that sacituzumab govitecan is considered moderately emetogenic, and prophylactic 2-drug antiemetic therapy is recommended. Moreover, if NVs are persistent, a 3-drug regimen may be used, including 5-HT3 RA, an NK1RA, and dexamethasone (10 mg PO or IV) [36].
The emetogenic risk of SG and the recommended antiemetic therapy are also inconsistent across clinical guidelines (Table 5). The MASCC and ESMO guidelines classify SGs at the high end of the moderate-risk category, such as carboplatin [15]. The NCCN classifies SGs as high risk [14]. The emetic risk of SG is not still defined by ASCO guidelines [16]. The JSCO guidelines also classify SG as the high end of the moderate-risk category [17].
No prospective clinical study evaluating optimal prophylactic antiemetic therapy in patients receiving SG has been reported. Treatment with SG is scheduled for days 1 and 8 of a 21-day cycle, and given that NV tends to occur later (the median time to onset of nausea was 8 days and that of vomiting was 24.5 days in the ASCENT), it is necessary to develop an antiemetic regimen tailored to the onset of these symptoms [37]. There is no evidence indicating the efficacy of weekly administration of NK1RA. A previous randomized clinical trial revealed no difference between weekly and triweekly fosaprepitant in terms of the primary outcome of CR in patients receiving concurrent chemoradiotherapy [38].
Datopotamab deruxtecan
Datopotamab deruxtecan (Dato-DXd) is a TROP2-directed ADC with a potent Topo I inhibitor, DXd. T-DXd and Dato-DXd adopt the same linker system and payload, and Dato-DXd has a lower DAR of 4 compared to 8 for T-DXd [40]. The incidence of NV is lower than that with T-DXd, likely due to a lower DAR [2, 41]. Although the emetic risk of Dato-DXd is still not defined by the NCCN guidelines, MASCC/ESMO guidelines, or ASCO, it seems to be a moderate emetic risk considering the incidence of vomiting in pivotal studies (Table 6). The protocol of the TROPION-Breast01 study recommended that subjects receive prophylactic antiemetic therapy such as 5-HT3 RA or NK1 RA and/or steroids [41].
Discussion
ADCs represent a novel class of targeted cancer therapeutics. We believe that there are two major future challenges in managing NV induced by ADCs. First, the development of personalized antiemetic therapy that is tailored to the onset and duration of NV and to patient risk is anticipated. This approach could enhance efficacy and reduce financial toxicity. The ERICA study revealed that the degree and duration of NV induced by T-DXd varied among patients. Future studies to identify prognostic and predictive factors in a larger cohort are anticipated. Who are the most likely to benefit from using olanzapine, NK1RA, or the combination of both drugs for prophylaxis? These questions should be answered to through future clinical trials. Personalized biomarker-based approaches are also expected to be developed. There are data suggesting that certain cytokines and peptides could be potential biomarkers for CINV [44, 45]. Second, decentralizing supportive care is crucial, as more patients seek care outside traditional hospital settings. The persistent NV induced by T-DXd and the delayed onset of NV induced by SG highlight the importance of decentralizing supportive care. Advances in telemedicine and remote monitoring now allow patients to manage side effects such as nausea from home, reducing the need for hospital visits. The utility of monitoring using ePRO, which triggers alerts during symptom exacerbation, has been demonstrated in several clinical trials and is expected to be widely implemented in future trials of supportive care [46]. A possible study design could be employed in clinical trials that adjusts antiemetic regimens for the following cycles based on the symptom during the first cycle. Addressing these challenges will require collaboration among healthcare providers, researchers, patients and technologists.
In conclusion, further studies are warranted to establish more patient-centered supportive care for ADC-induced NV.
References
Tarantino P, Ricciuti B, Pradhan SM, Tolaney SM. Optimizing the safety of antibody-drug conjugates for patients with solid tumours. Nat Rev Clin Oncol. 2023;20:558–76.
Cortés J, Kim S-B, Chung W-P, Im S-A, Park YH, Hegg R, et al. Trastuzumab deruxtecan versus trastuzumab emtansine for breast cancer. N Engl J Med. 2022;386:1143–54.
Modi S, Jacot W, Yamashita T, Sohn J, Vidal M, Tokunaga E, et al. Trastuzumab deruxtecan in previously treated HER2-low advanced breast cancer. N Engl J Med. 2022. https://doi.org/10.1056/NEJMoa2203690.
Bardia A, Hurvitz SA, Tolaney SM, Loirat D, Punie K, Oliveira M, et al. Sacituzumab govitecan in metastatic triple-negative breast cancer. N Engl J Med. 2021;384:1529–41.
Bardia A, Jhaveri K, Im SA, Pernas S, De Laurentiis M, Wang S, et al. Datopotamab deruxtecan versus chemotherapy in previously treated inoperable/metastatic hormone receptor-positive human epidermal growth factor receptor 2-negative breast cancer: primary results from TROPION-Breast01. J Clin Oncol. 2024. https://doi.org/10.1200/JCO.24.00920.
Sommariva S, Pongiglione B, Tarricone R. Impact of chemotherapy-induced nausea and vomiting on health-related quality of life and resource utilization: a systematic review. Crit Rev Oncol Hematol. 2016;99:13–36.
Navari RM, Aapro M. Antiemetic prophylaxis for chemotherapy-induced nausea and vomiting. N Engl J Med. 2016;374:1356–67.
Aapro M. CINV: still troubling patients after all these years. Support Care Cancer. 2018;26:5–9.
Wickham RJ. Revisiting the physiology of nausea and vomiting-challenging the paradigm. Support Care Cancer. 2020;28:13–21.
Lohr L. Chemotherapy-induced nausea and vomiting. Cancer J. 2008;14:85–93.
Kenward H, Pelligand L, Savary-Bataille K, Elliott J. Nausea: current knowledge of mechanisms, measurement and clinical impact. Vet J. 2015;203:36–43.
Doi T, Shitara K, Naito Y, Shimomura A, Fujiwara Y, Yonemori K, et al. Safety, pharmacokinetics, and antitumour activity of trastuzumab deruxtecan (DS-8201), a HER2-targeting antibody-drug conjugate, in patients with advanced breast and gastric or gastro-oesophageal tumours: a phase 1 dose-escalation study. Lancet Oncol. 2017;18:1512–22.
Harbeck N, Ciruelos E, Jerusalem G, Müller V, Niikura N, Viale G, et al. Trastuzumab deruxtecan in HER2-positive advanced breast cancer with or without brain metastases: a phase 3b/4 trial. Nat Med. 2024. https://doi.org/10.1016/S0140-6736(22)02420-5.
NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) Antiemesis, version 2 (2024)
Scotté F, Schwartzberg L, Lihara H, Aapro M, Gralla R, Hesketh PJ, et al. 2023 updated MASCC/ESMO Consensus recommendations: Prevention of nausea and vomiting following moderately emetic risk antineoplastic agents. Support Care Cancer. 2023;32:45.
Hesketh PJ, Kris MG, Basch E, Bohlke K, Barbour SY, Clark-Snow RA, et al. Antiemetics: ASCO guideline update. J Clin Oncol. 2020;38:2782–97.
Iihara H, Abe M, Wada M, Iino K, Akechi T, Imamura CK, et al. 2023 Japan Society of clinical oncology clinical practice guidelines update for antiemesis. Int J Clin Oncol. 2024;29:873–88.
Sekine I, Segawa Y, Kubota K, Saeki T. Risk factors of chemotherapy-induced nausea and vomiting: index for personalized antiemetic prophylaxis. Cancer Sci. 2013;104:711–7.
Tsuji D, Suzuki K, Kawasaki Y, Goto K, Matsui R, Seki N, et al. Risk factors associated with chemotherapy-induced nausea and vomiting in the triplet antiemetic regimen including palonosetron or granisetron for cisplatin-based chemotherapy: analysis of a randomized, double-blind controlled trial. Support Care Cancer. 2019;27:1139–47.
Ogitani Y, Aida T, Hagihara K, Yamaguchi J, Ishii C, Harada N, et al. DS-8201a, a novel HER2-targeting ADC with a novel DNA Topoisomerase I inhibitor, demonstrates a promising antitumor efficacy with differentiation from T-DM1. Clin Cancer Res. 2016;22:5097–108.
Park YH, Cortés J, Modi S, Hurvitz SA, Bianchini G, Iwata H, et al. Pooled analysis on characteristics of nausea and vomiting in patients receiving trastuzumab deruxtecan (T-DXd) in clinical studies. J Clin Oncol. 2024;42:12118.
Ueno NT, Jacot W, Yamashita T, Sohn J, Tokunaga E, Prat A, et al. 217O Patient-reported outcomes (PROs) from DESTINY-Breast04, a randomized phase III study of trastuzumab deruxtecan (T-DXd) vs treatment of physician’s choice (TPC) in patients (pts) with HER2-low metastatic breast cancer (MBC). Ann Oncol. 2022;33:S632–3.
Hu X, Curigliano G, Yonemori K, Bardia A, Barrios CHE, Sohn J, et al. LBA22 Effects of trastuzumab deruxtecan (T-DXd) vs choice of chemotherapy (TPC) on patient-reported outcomes (PROs) in hormone receptor-positive, HER2-low or HER2-ultralow metastatic breast cancer (mBC): results from DESTINY-Breast06. Ann Oncol. 2024;35:S1214–5.
Ooki A, Aoyama T, Oba K, Nishikawa K, Kawabata R, Honda M, et al. 454P a multicenter randomized open-label phase II study investigating optimal antiemetic therapy for patients with advanced/recurrent gastric cancer treated with trastuzumab deruxtecan (T-DXd): EN-hance study. Ann Oncol. 2023;34:S1639–40.
Iihara H, Shimokawa M, Bando H, Niwa Y, Mizuno Y, Kawaguchi Y, et al. Doublet or triplet antiemetic prophylaxis for nausea and vomiting induced by trastuzumab deruxtecan: an open-label, randomized, and multicenter exploratory phase 2 study. J Cancer. 2023;14:2644–54.
Sakai H, Tsurutani J, Ozaki Y, Ishiguro H, Nozawa K, Yamanaka T, et al. A randomized, double-blind, placebo-controlled phase II study of olanzapine-based prophylactic antiemetic therapy for delayed and persistent nausea and vomiting in patients with HER2-positive or HER2-low breast cancer treated with trastuzumab deruxtecan: ERICA study (WJOG14320B). Ann Oncol. 2024. https://doi.org/10.1016/j.annonc.2024.09.001.
Modi S, Saura C, Yamashita T, Park YH, Kim S-B, Tamura K, et al. Trastuzumab deruxtecan in previously treated HER2-positive breast cancer. N Engl J Med. 2019;382:610–21.
André F, Hee Park Y, Kim S-B, Takano T, Im S-A, Borges G, et al. Trastuzumab deruxtecan versus treatment of physician’s choice in patients with HER2-positive metastatic breast cancer (DESTINY-Breast02): a randomised, open-label, multicentre, phase 3 trial. The Lancet. 2023;401:1773–85.
Li BT, Smit EF, Goto Y, Nakagawa K, Udagawa H, Mazières J, et al. Trastuzumab deruxtecan in HER2-mutant non-small-cell lung cancer. N Engl J Med. 2022;386:241–51.
Goto K, Goto Y, Kubo T, Ninomiya K, Kim SW, Planchard D, et al. Trastuzumab deruxtecan in patients with HER2-mutant metastatic non-small-cell lung cancer: primary results from the randomized, phase II DESTINY-Lung02 trial. J Clin Oncol. 2023;41:4852–63.
Shitara K, Bang YJ, Iwasa S, Sugimoto N, Ryu MH, Sakai D, et al. Trastuzumab deruxtecan in previously treated HER2-positive gastric cancer. N Engl J Med. 2020;382:2419–30.
Van Cutsem E, di Bartolomeo M, Smyth E, Chau I, Park H, Siena S, et al. Trastuzumab deruxtecan in patients in the USA and Europe with HER2-positive advanced gastric or gastroesophageal junction cancer with disease progression on or after a trastuzumab-containing regimen (DESTINY-Gastric02): primary and updated analyses from a single-arm, phase 2 study. Lancet Oncol. 2023;24:744–56.
Meric-Bernstam F, Makker V, Oaknin A, Oh D-Y, Banerjee S, González-Martín A, et al. Efficacy and safety of trastuzumab deruxtecan in patients with HER2-expressing solid tumors: primary results from the DESTINY-PanTumor02 phase II trial. J Clin Oncol. 2024;42:47–58.
Cardillo TM, Govindan SV, Sharkey RM, Trisal P, Arrojo R, Liu D, et al. Sacituzumab govitecan (IMMU-132), an anti-trop-2/SN-38 antibody-drug conjugate: characterization and efficacy in pancreatic, gastric, and other cancers. Bioconjug Chem. 2015;26:919–31.
Kopp A, Hofsess S, Cardillo TM, Govindan SV, Donnell J, Thurber GM. Antibody-drug conjugate sacituzumab govitecan drives efficient tissue penetration and rapid intracellular drug release. Mol Cancer Ther. 2023;22:102–11.
Rugo HS, Bardia A, Marmé F, Cortés J, Schmid P, Loirat D, et al. Overall survival with sacituzumab govitecan in hormone receptor-positive and human epidermal growth factor receptor 2-negative metastatic breast cancer (TROPiCS-02): a randomised, open-label, multicentre, phase 3 trial. The Lancet. 2023;402:1423–33.
Rugo HS, Tolaney SM, Loirat D, Punie K, Bardia A, Hurvitz SA, et al. Safety analyses from the phase 3 ASCENT trial of sacituzumab govitecan in metastatic triple-negative breast cancer. NPJ Breast Cancer. 2022;8:98.
Yang Q, Zou X, Xie YL, Lin C, Ouyang YF, Liu YL, et al. Fosaprepitant weekly vs every 3 weeks for the prevention of concurrent chemoradiotherapy-induced nausea and vomiting: a pilot randomized clinical trial. JAMA Netw Open. 2023;6: e2326127.
Tagawa ST, Balar AV, Petrylak DP, Kalebasty AR, Loriot Y, Fléchon A, et al. TROPHY-U-01: a phase II open-label study of sacituzumab govitecan in patients with metastatic urothelial carcinoma progressing after platinum-based chemotherapy and checkpoint inhibitors. J Clin Oncol. 2021;39:2474–85.
Okajima D, Yasuda S, Maejima T, Karibe T, Sakurai K, Aida T, et al. Datopotamab deruxtecan, a novel TROP2-directed antibody-drug conjugate, demonstrates potent antitumor activity by efficient drug delivery to tumor cells. Mol Cancer Ther. 2021;20:2329–40.
Bardia A, Jhaveri K, Im S-A, Pernas S, Laurentiis MD, Wang S, et al. Datopotamab deruxtecan versus chemotherapy in previously treated inoperable/metastatic hormone receptor-positive human epidermal growth factor receptor 2–negative breast cancer: primary results from TROPION-Breast01. J Clin Oncol. 2025. https://doi.org/10.1200/JCO.24.00920.
Bardia A, Krop IE, Kogawa T, Juric D, Tolcher AW, Hamilton EP, et al. Datopotamab deruxtecan in advanced or metastatic HR+/HER2- and triple-negative breast cancer: results from the phase I TROPION-PanTumor01 study. J Clin Oncol. 2024;42:2281–94.
Shimizu T, Sands J, Yoh K, Spira A, Garon EB, Kitazono S, et al. First-in-human, phase I dose-escalation and dose-expansion study of trophoblast cell-surface antigen 2–directed antibody-drug conjugate datopotamab deruxtecan in non–small-cell lung cancer: TROPION-PanTumor01. J Clin Oncol. 2023;41:4678–87.
Breen DM, Kim H, Bennett D, Calle RA, Collins S, Esquejo RM, et al. GDF-15 neutralization alleviates platinum-based chemotherapy-induced emesis, anorexia, and weight loss in mice and nonhuman primates. Cell Metab. 2020;32:938-50.e6.
Park HS, Won HS, An HJ, Cho SS, Kim HH, Sun S, et al. Elevated serum substance P level as a predictive marker for moderately emetogenic chemotherapy-induced nausea and vomiting: a prospective cohort study. Cancer Med. 2021;10:1057–65.
Kikawa Y, Uemura Y, Taira T, Kitagawa C, Maeda H, Kato H, et al. A randomized study comparing electronic patient-reported outcome (ePRO) monitoring with routine follow-up during trastuzumab deruxtecan treatment in patients with metastatic breast cancer (PRO-DUCE study). J Clin Oncol. 2024;42:1504.
Acknowledgment
Figure 1 was created using illustrations purchased from LAIMAN Stockweb https://laimanstockweb.com/.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. The first draft of the manuscript was written by Jawhara Farhat and Hitomi Sakai. Junji Tsurutani commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
HS has received support for the present manuscript (to institution) and medical writing support from Daiichi Sankyo, lecture fees for Daiichi Sankyo, Chugai Pharmaceutical, and Eli Lilly, advisory role fee from Gilead Sciences. JT has received support for the present manuscript from Daiichi Sankyo (to institution), research grants from Eli Lilly, Daiichi Sankyo, and AstraZeneca (to institution), personal fees for Consulting/honoraria for lectures, presentations, speakers’ bureaus, manuscript writing or educational events/advisory board from Daiichi Sankyo and AstraZeneca.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Farhat, J., Sakai, H. & Tsurutani, J. Management of nausea and vomiting induced by antibody–drug conjugates. Breast Cancer 32, 278–285 (2025). https://doi.org/10.1007/s12282-025-01670-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12282-025-01670-1